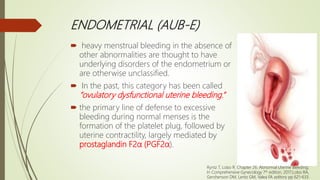
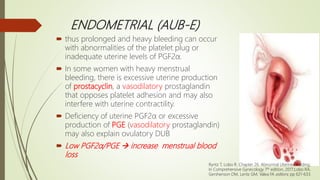
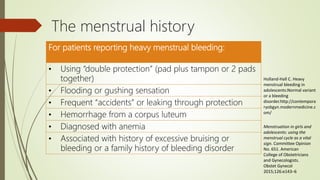
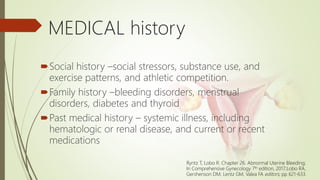
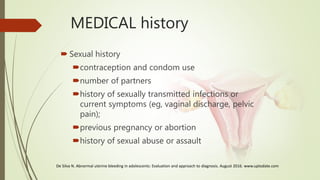
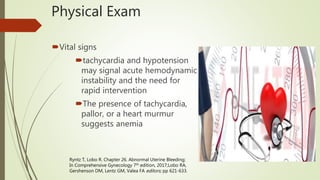
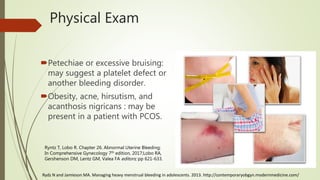
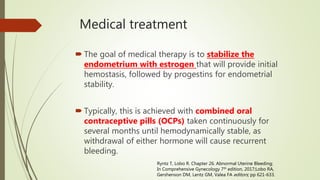
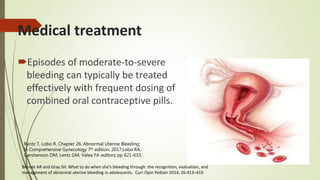
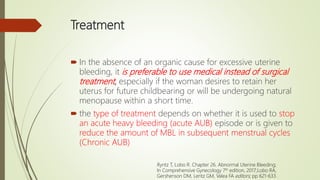
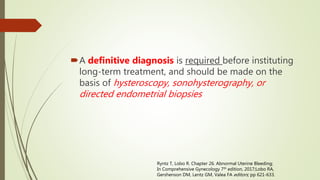
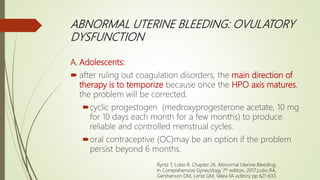
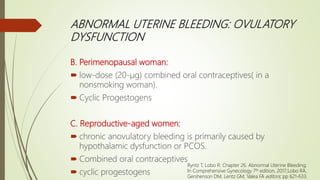
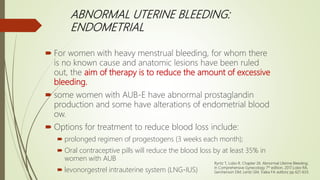
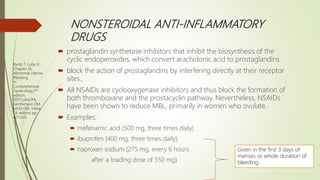
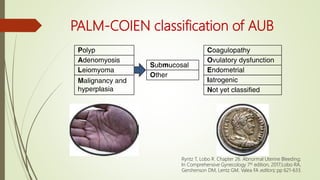
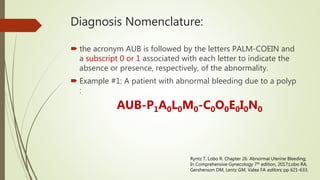
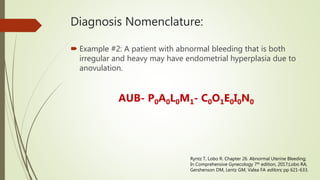
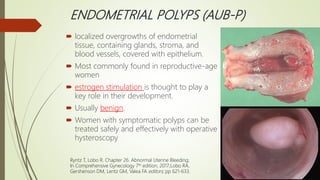
The document discusses abnormal uterine bleeding (AUB), a common health concern among women characterized by heavy menstrual bleeding, irregular cycles, and prolonged duration. It provides definitions, classifications, diagnostic approaches, examples of underlying causes including endometrial polyps, adenomyosis, malignancies, coagulopathies, and ovulatory dysfunction, as well as management strategies. Treatment options vary based on the specific cause of AUB and may include medical and surgical interventions.


![CH ristocetin cofactor should be obtained to rule out a coagula-
Adults with HMB and h/o either
One of the following Two of the following
Testing
Figure 26.6 Diagnostic approach to adults with abnormal uterine
bleeding due to coagulopathy. (Data from Kouides PA, Conard J,
Peyvandi F, et al. Hemostasis and menstruation: appropriate investi -
gation for underlying disorders of hemostasis in women with exces -
sive menstrual bleeding. Fertil Steril. 2005;84[5]:1345-1351.)
100 1000
al blood loss (mL)
5
ratio of endogenous concentra -
prostaglandin E and menstrual
endometrium; persistent endo -
H, Kelly RW, et al. The synthesis
roliferative endometrium. JClin
289.)
Ryntz T, Lobo R. Chapter 26. Abnormal Uterine Bleeding;
In Comprehensive Gynecology 7th edition, 2017;Lobo RA,
Gershenson DM, Lentz GM, Valea FA editors; pp 621-633.](https://image.slidesharecdn.com/aub-180620141421/85/Abnormal-Uterine-Bleeding-15-320.jpg)