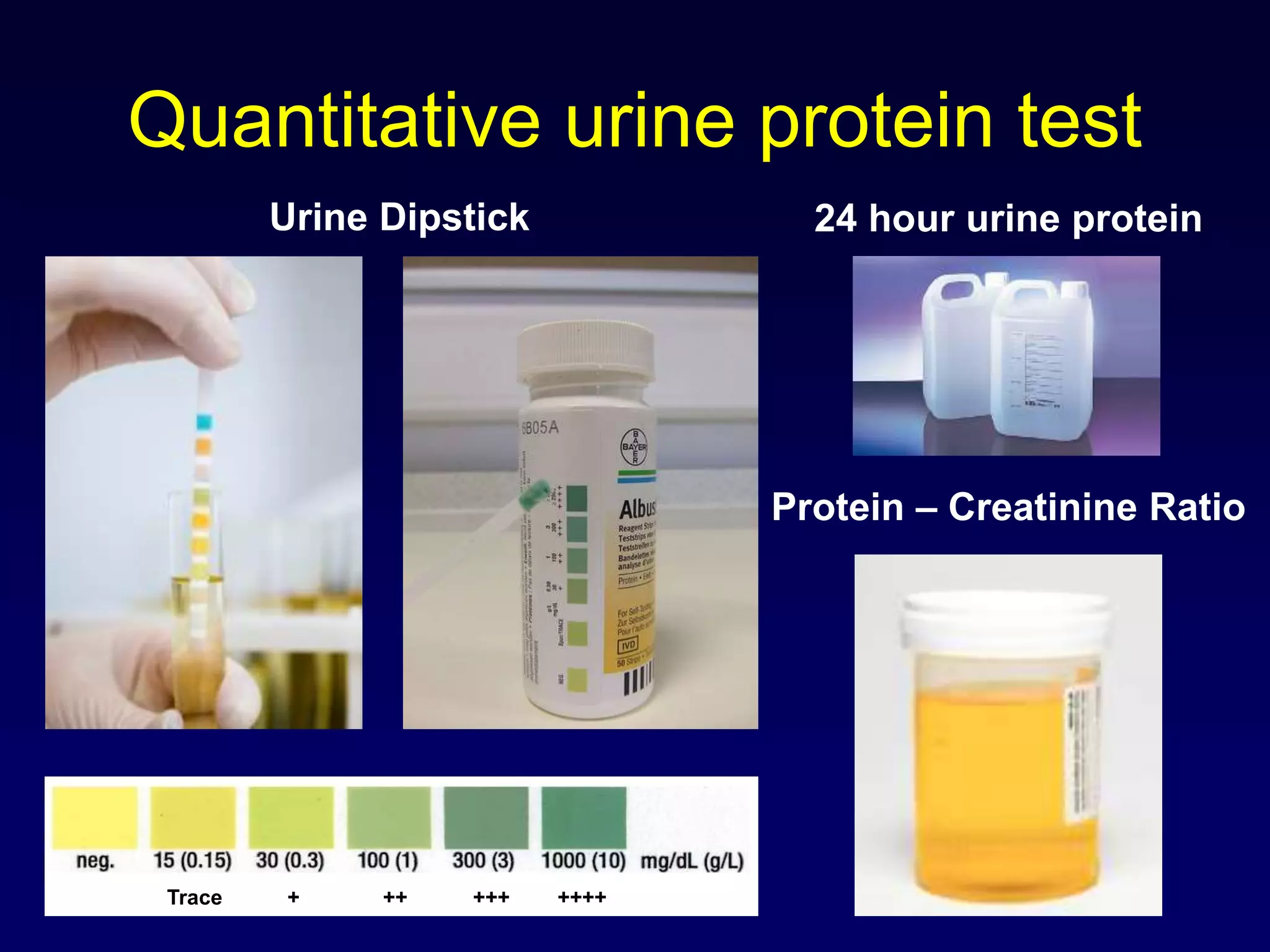
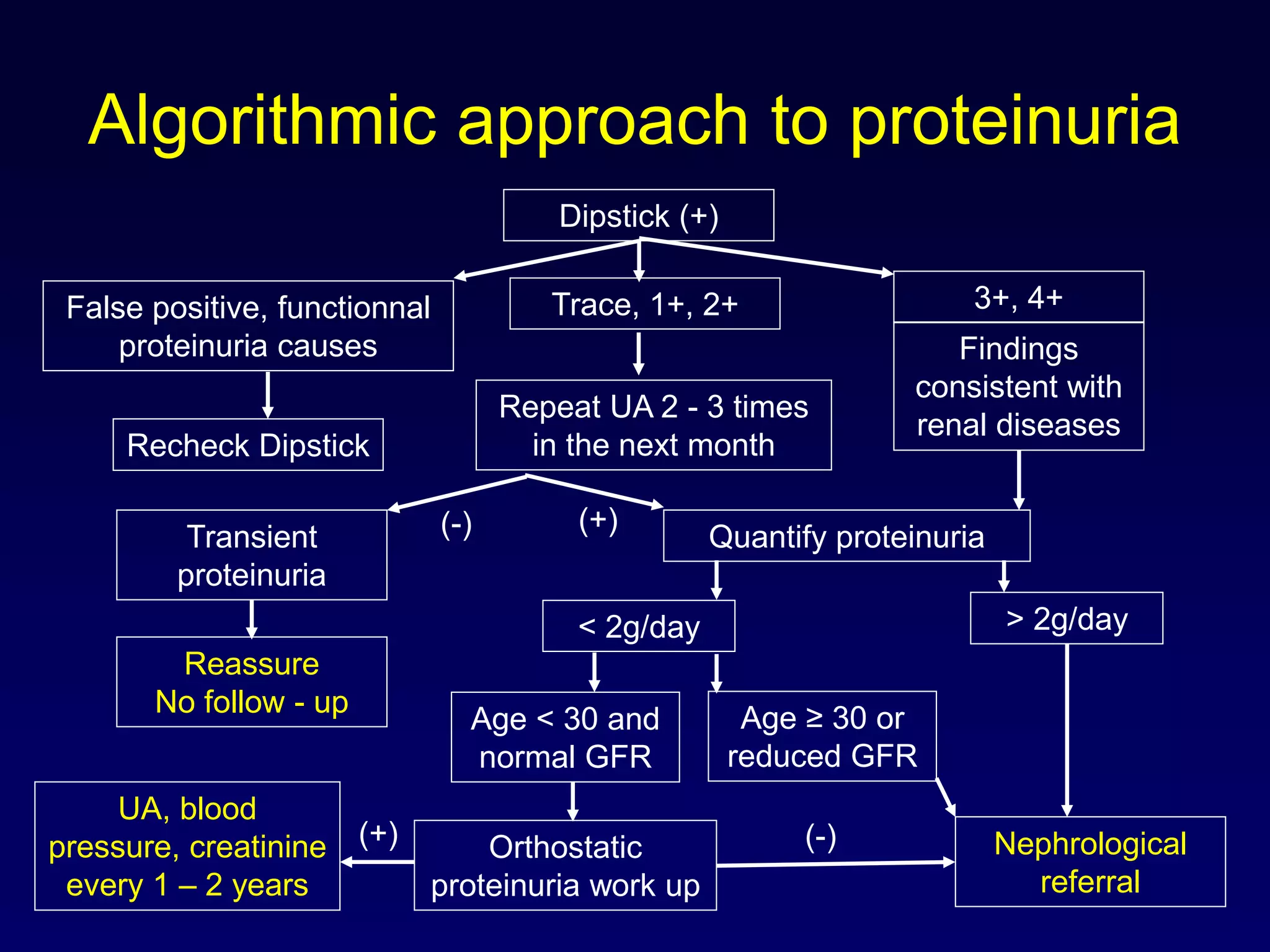
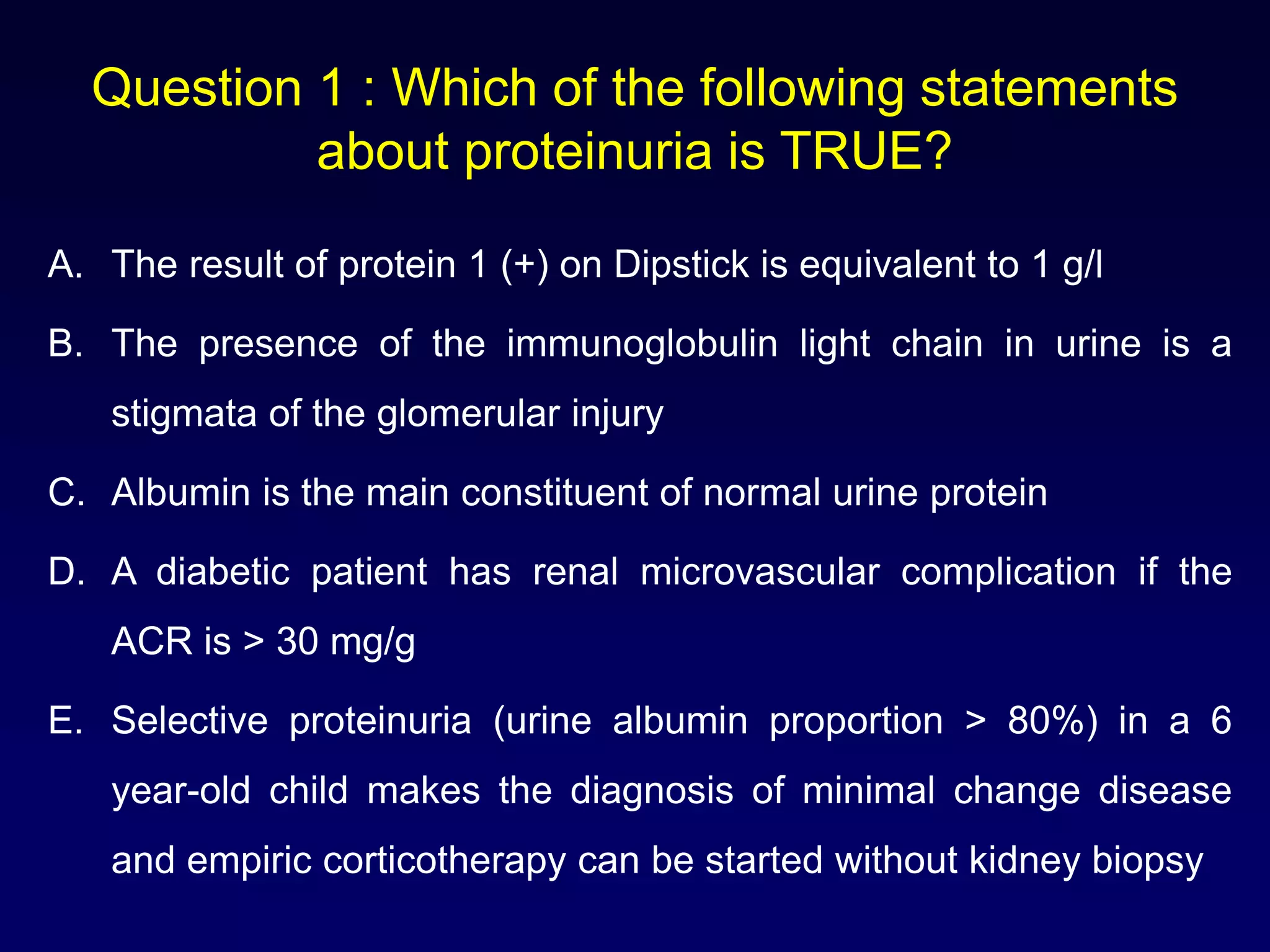
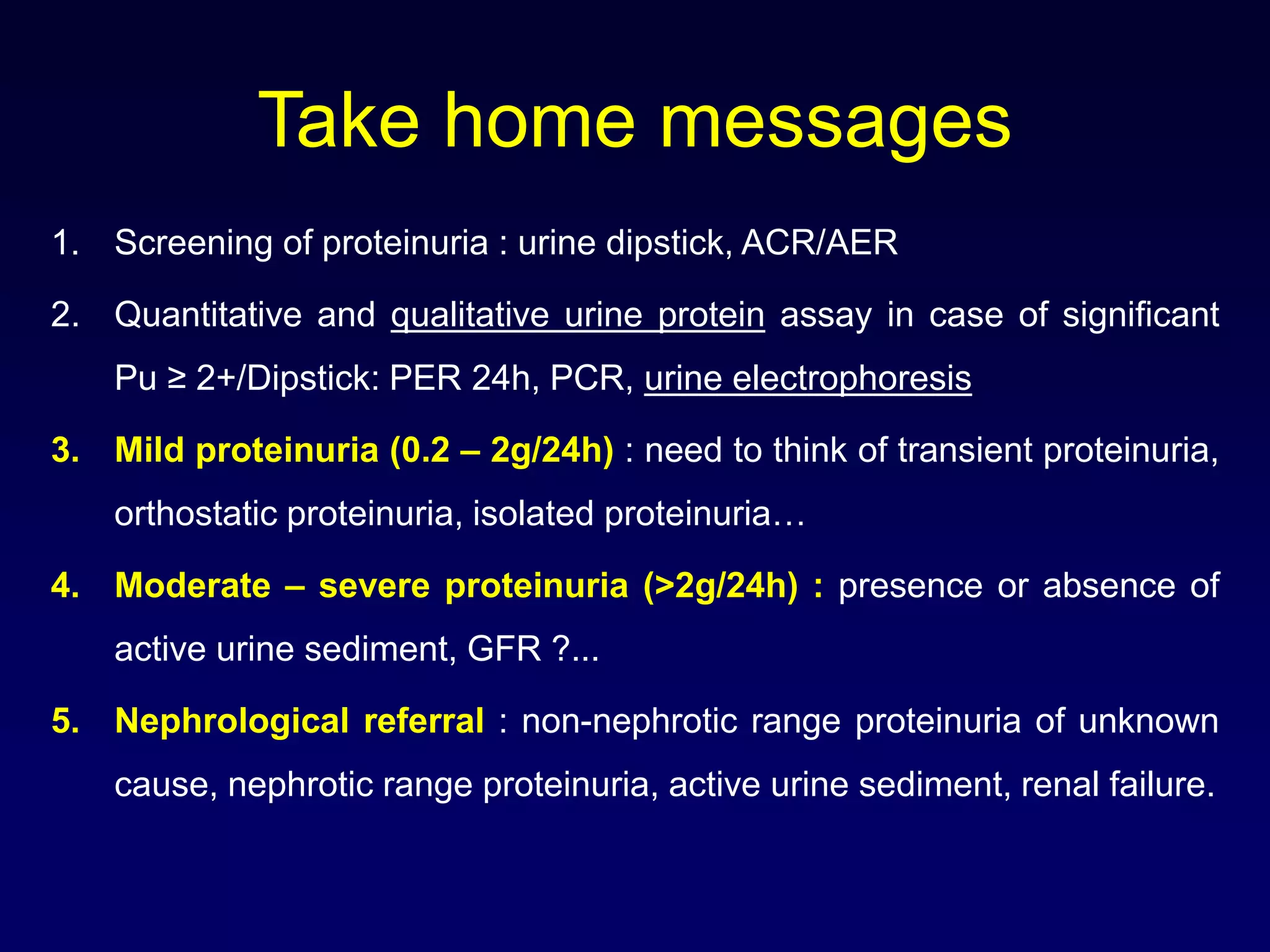
The document provides an in-depth approach to diagnosing and managing proteinuria, outlining definitions, types, and causes of proteinuria along with quantitative and qualitative testing methods. It discusses benign proteinuria, clinical examinations, laboratory tests, and algorithmic approaches for referrals to nephrologists based on specific patient criteria. Key take-home messages emphasize the importance of urine dipstick screening, further assays for significant proteinuria, and when to consider nephrological referrals.