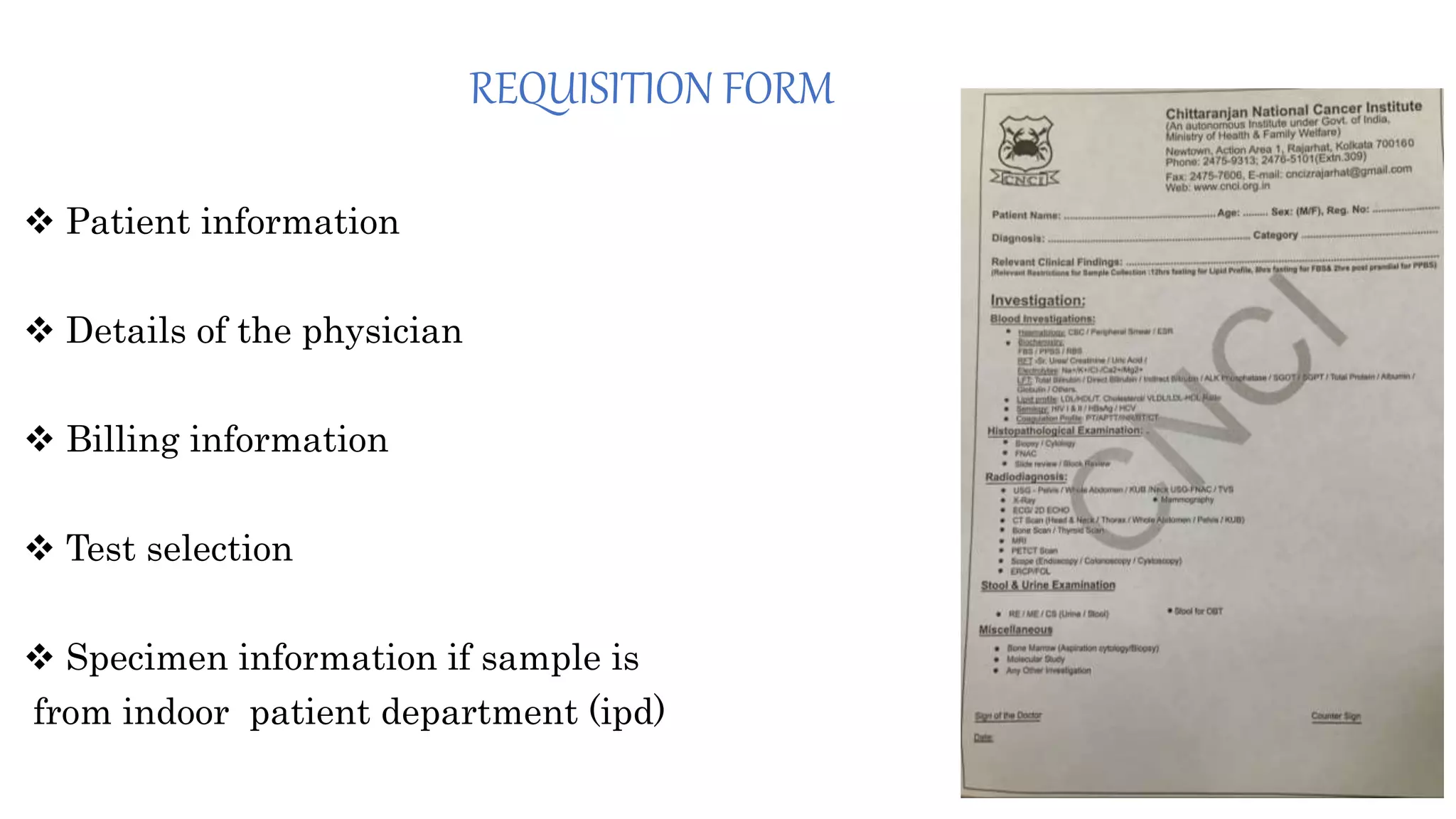
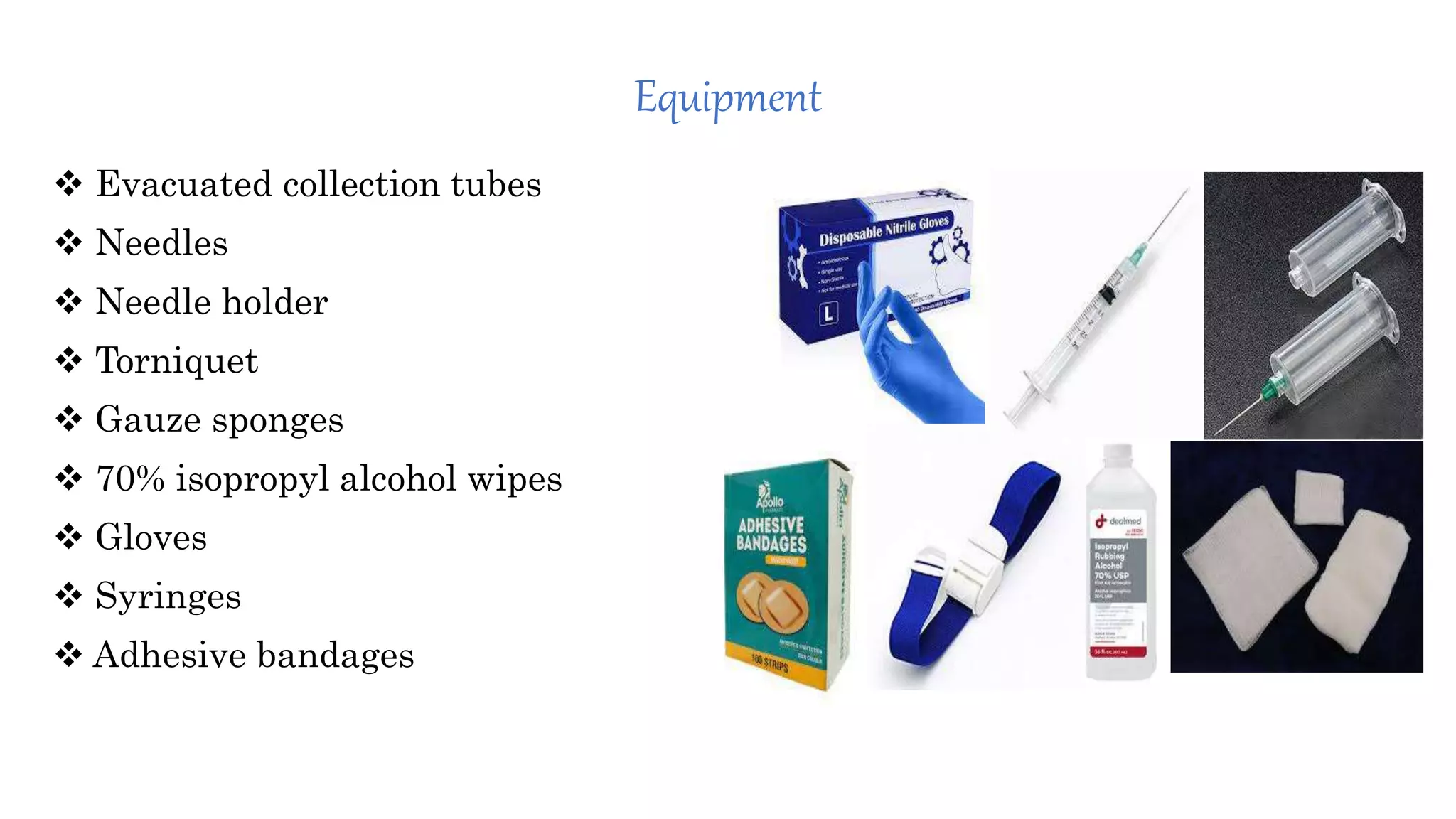
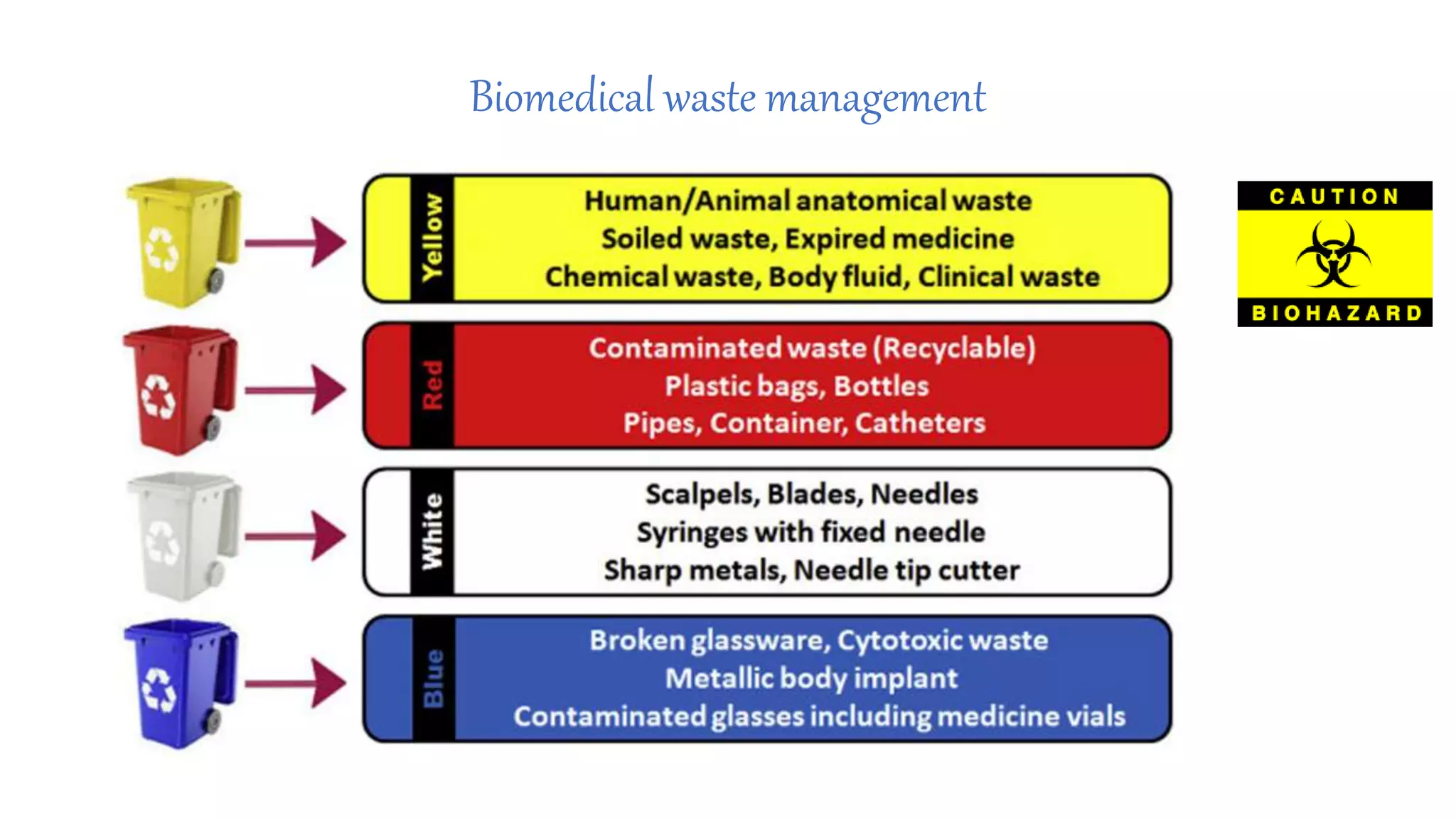
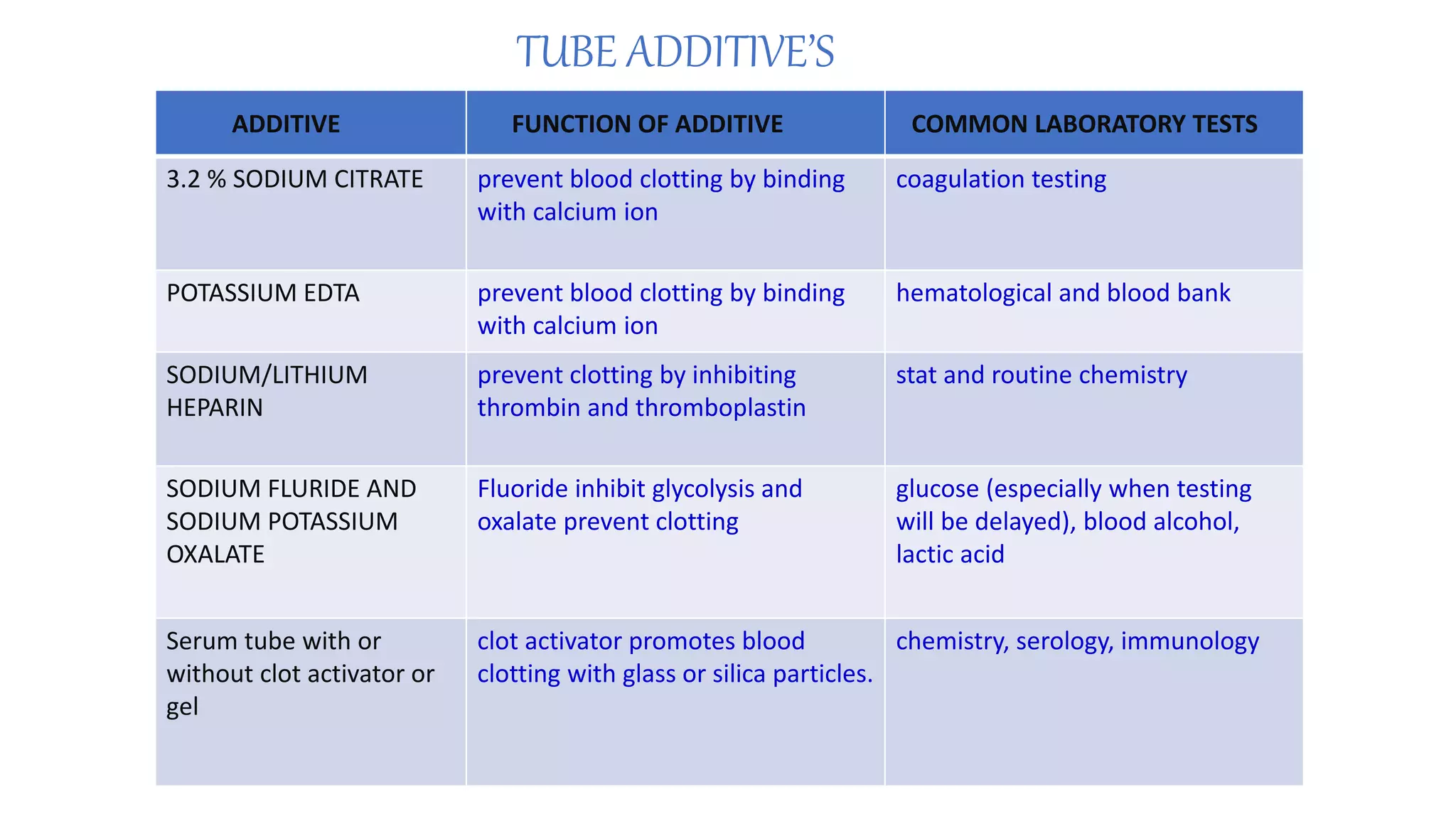
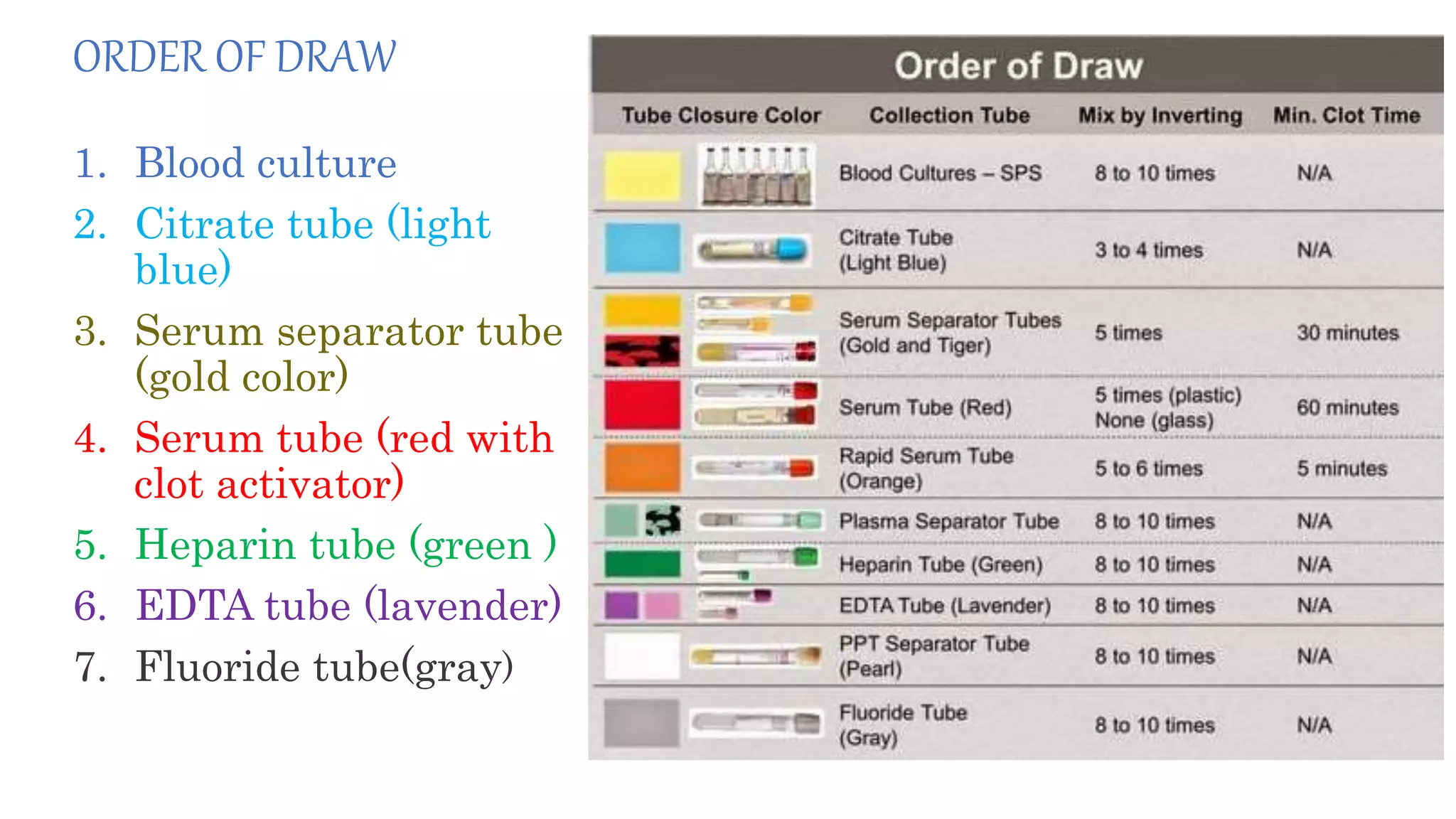
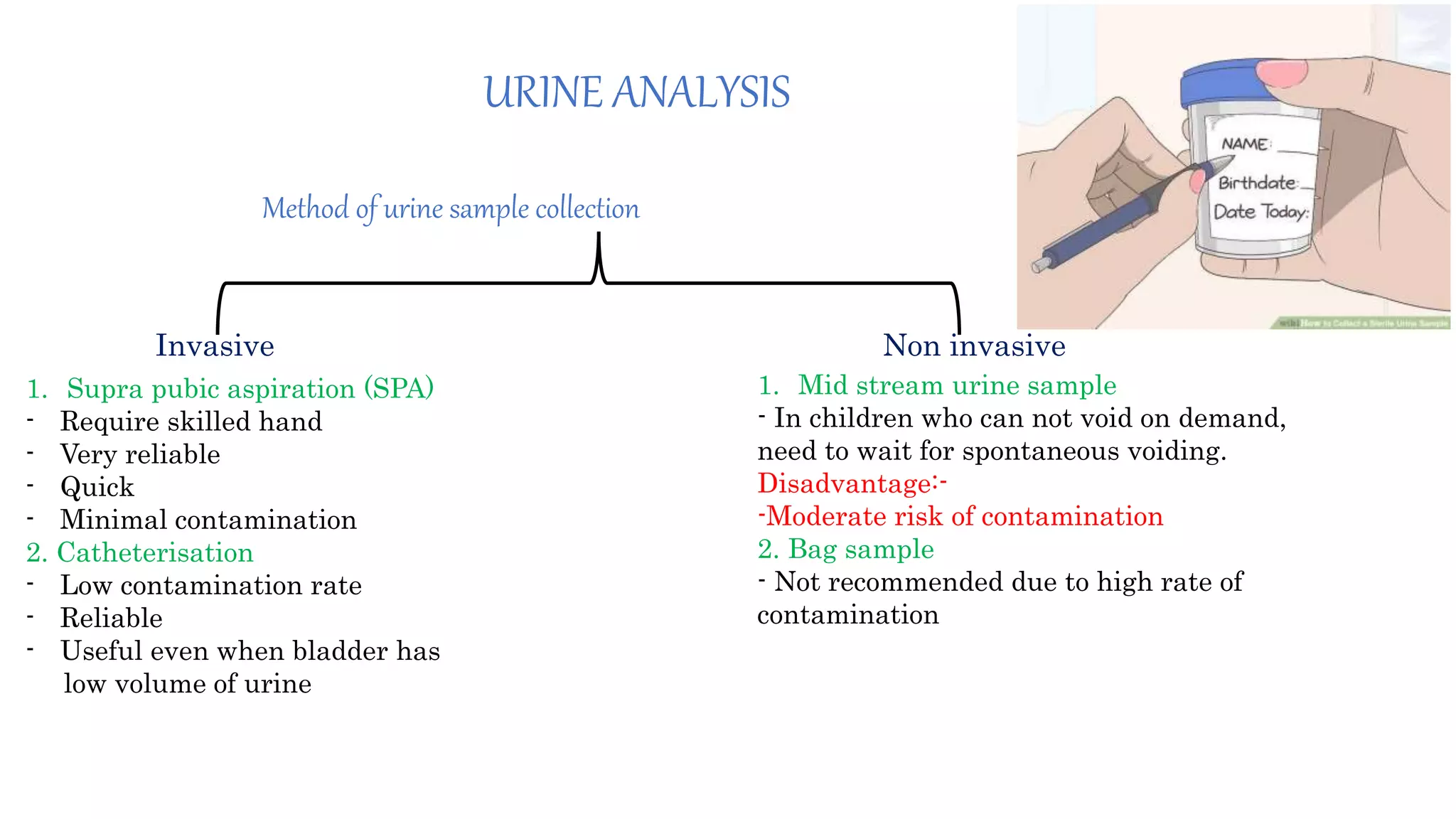
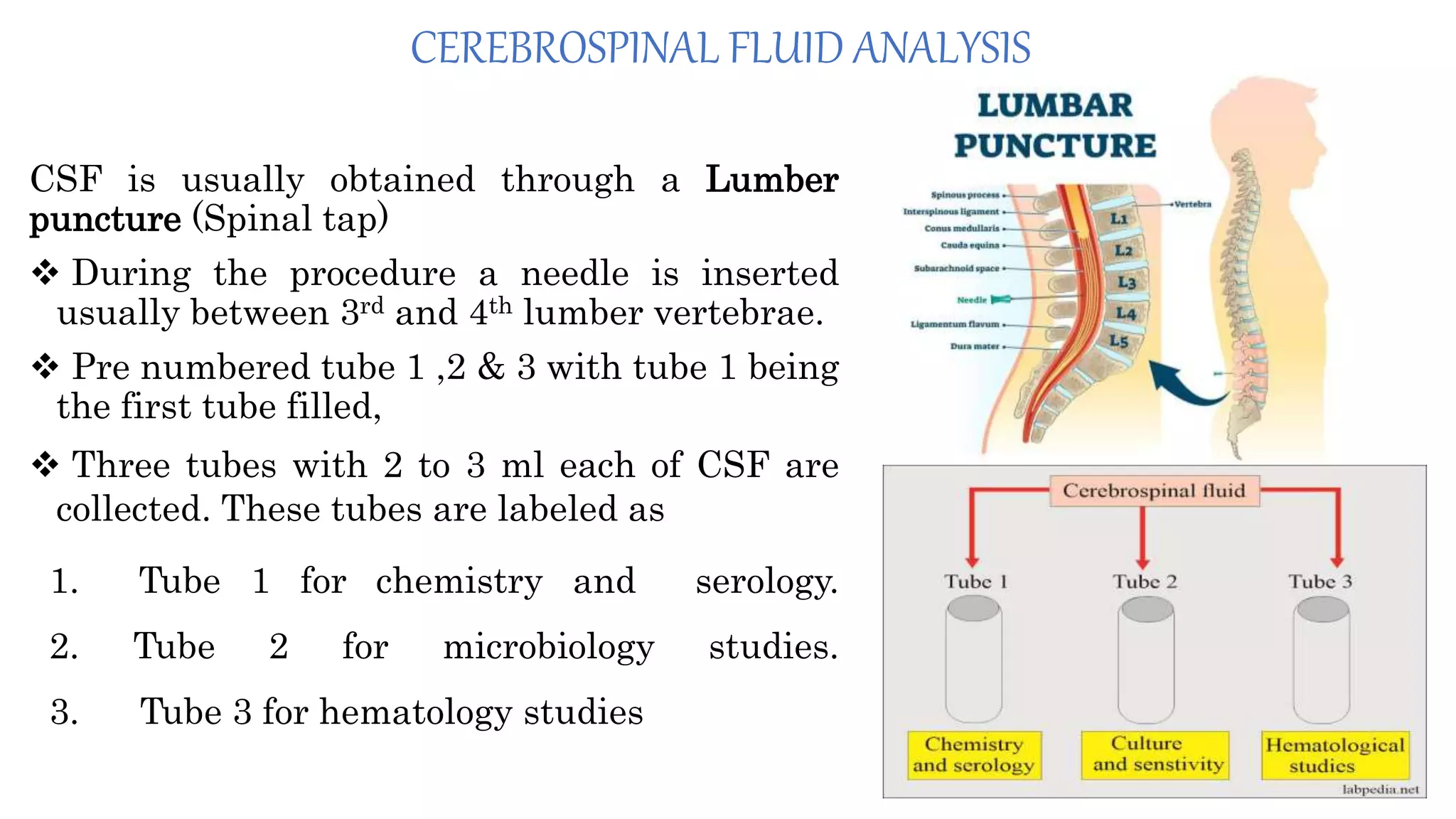
This document discusses sample collection in clinical biochemistry. It outlines the essential steps in sample collection including patient identification, sample collection and processing, and storage and transport. It describes the proper procedures, equipment, and additives used for collecting different sample types like blood, urine, cerebrospinal fluid, and arterial blood gas. Potential errors are discussed along with ways to avoid errors like hemolysis, clotting, and contamination. Maintaining proper procedures is important for obtaining accurate laboratory test results.