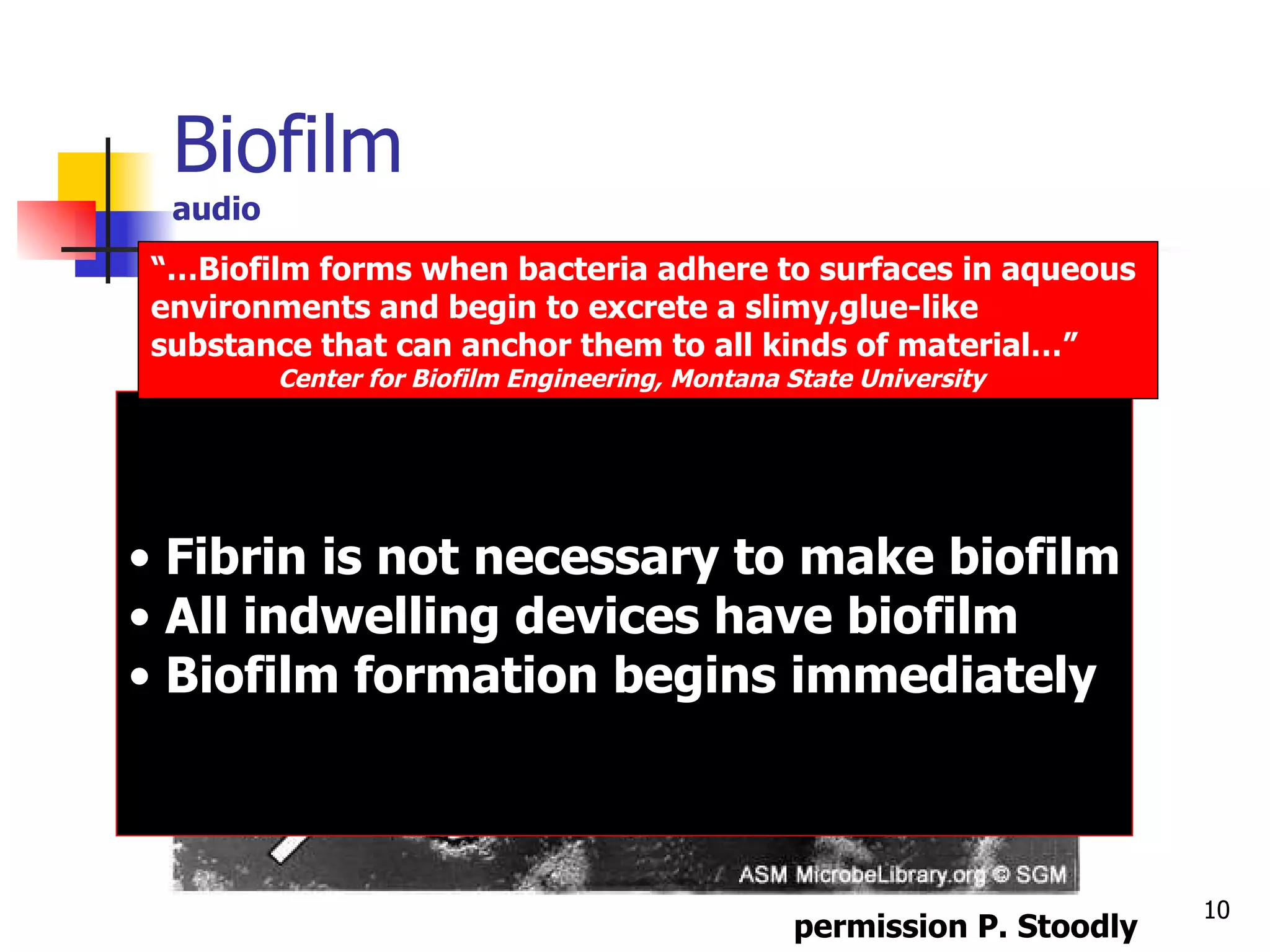
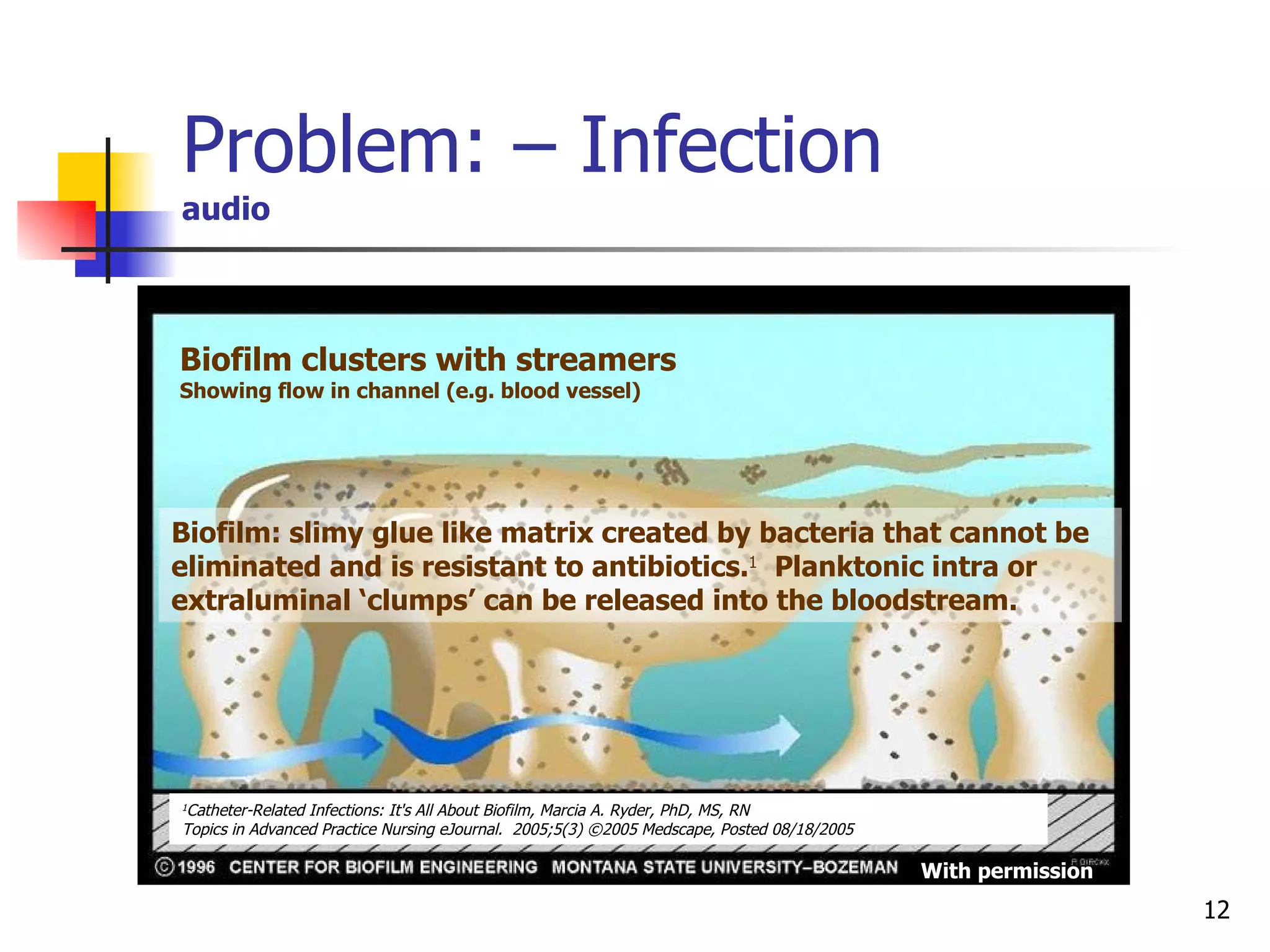
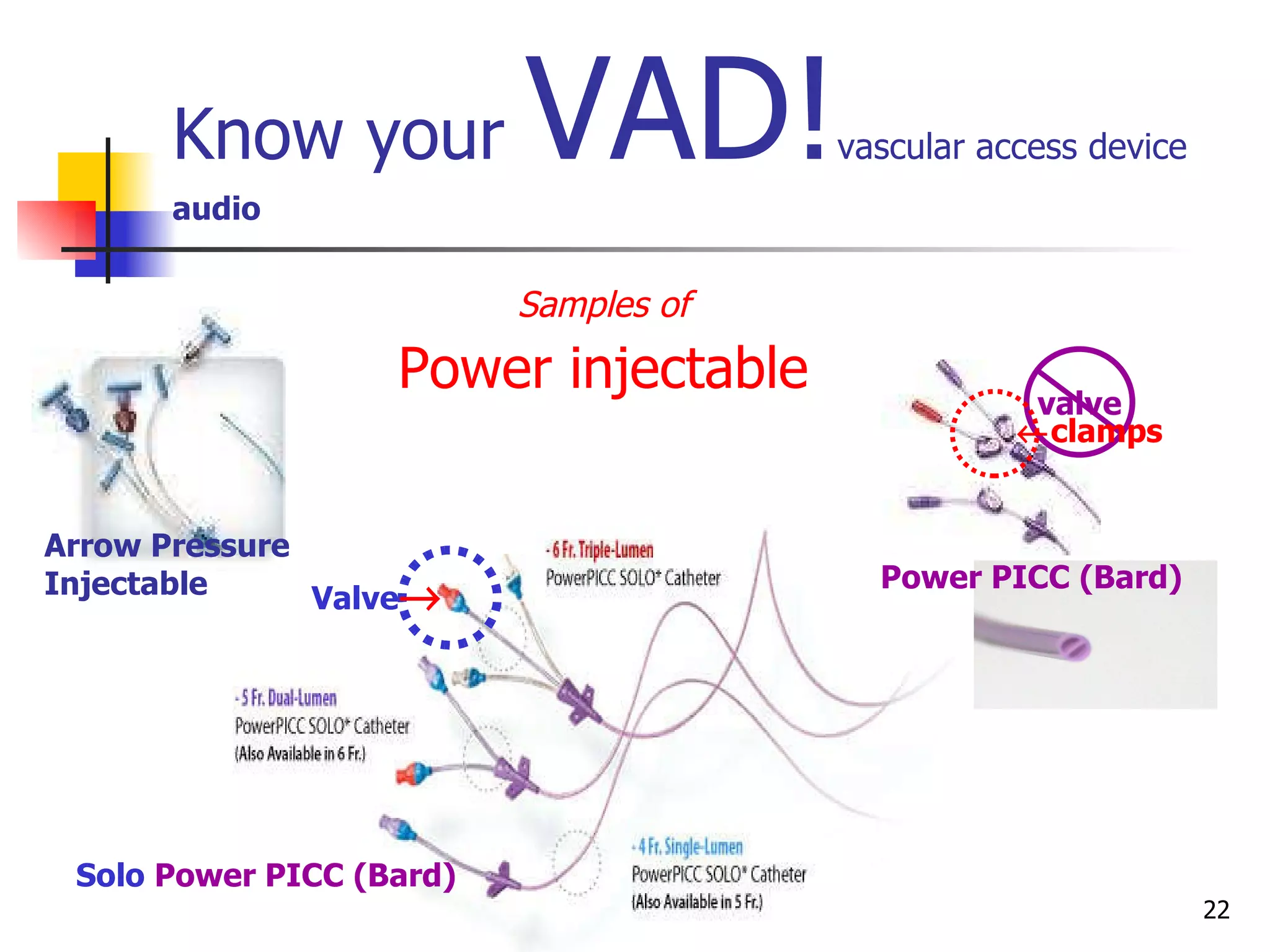
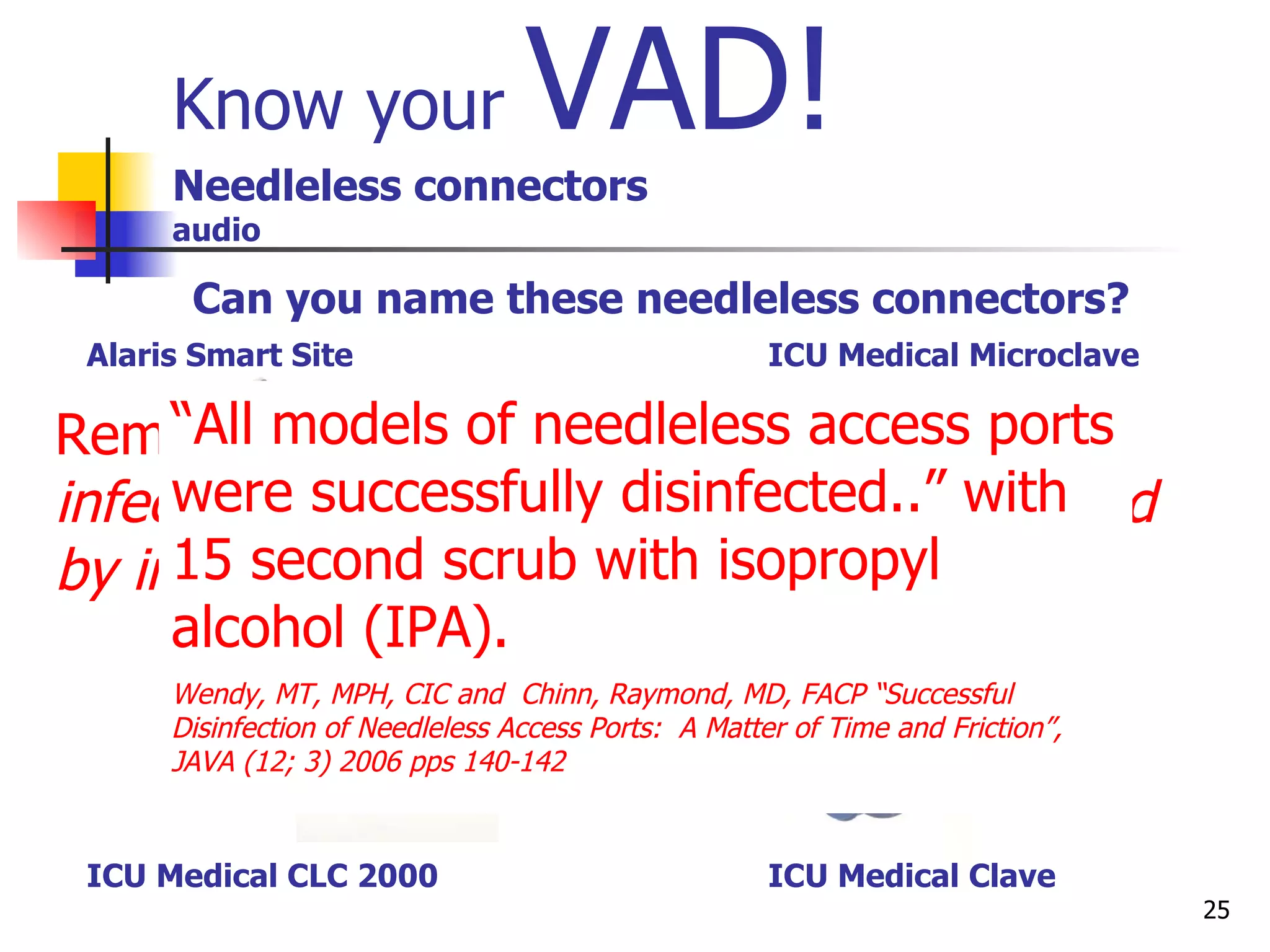
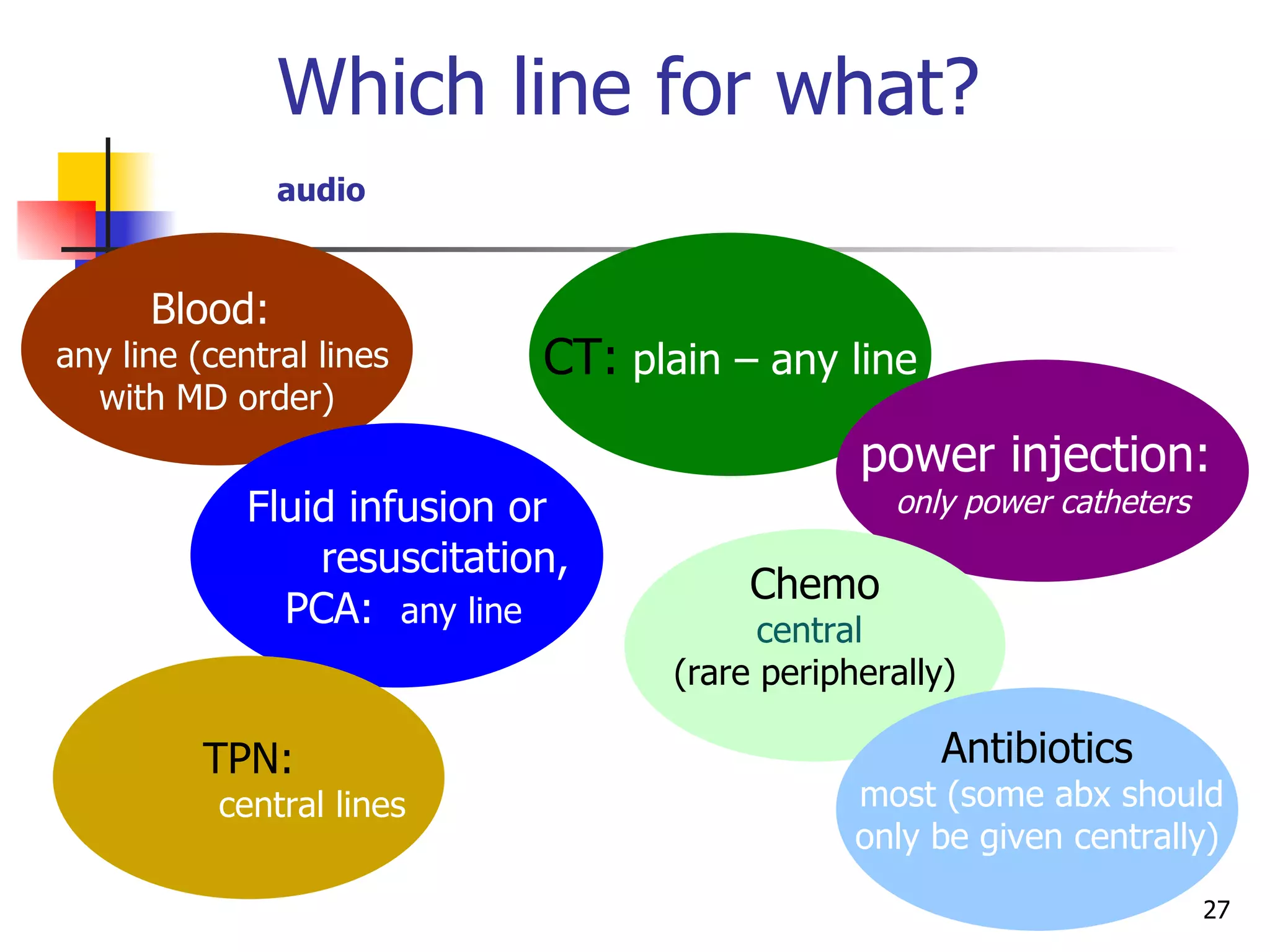
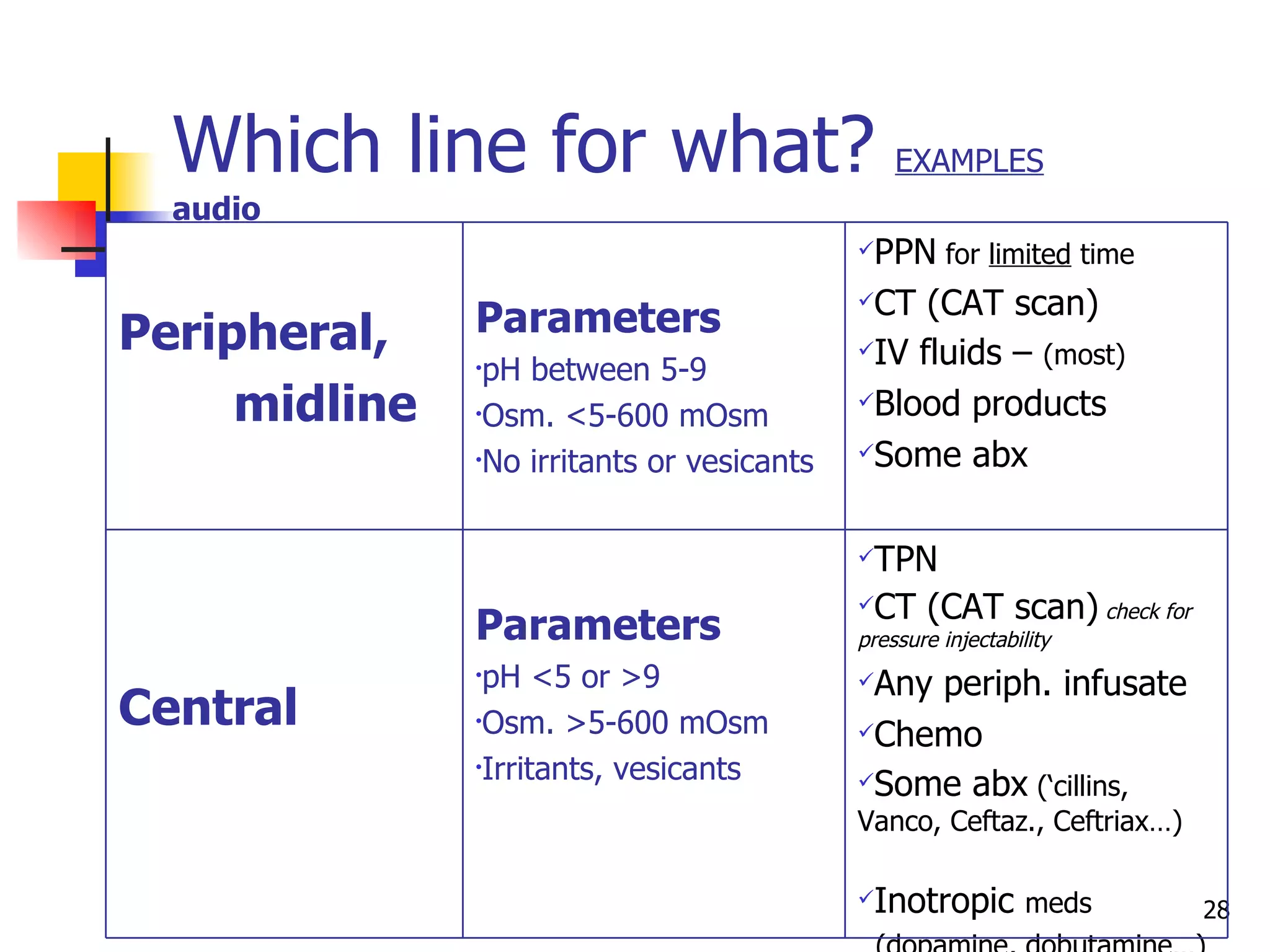
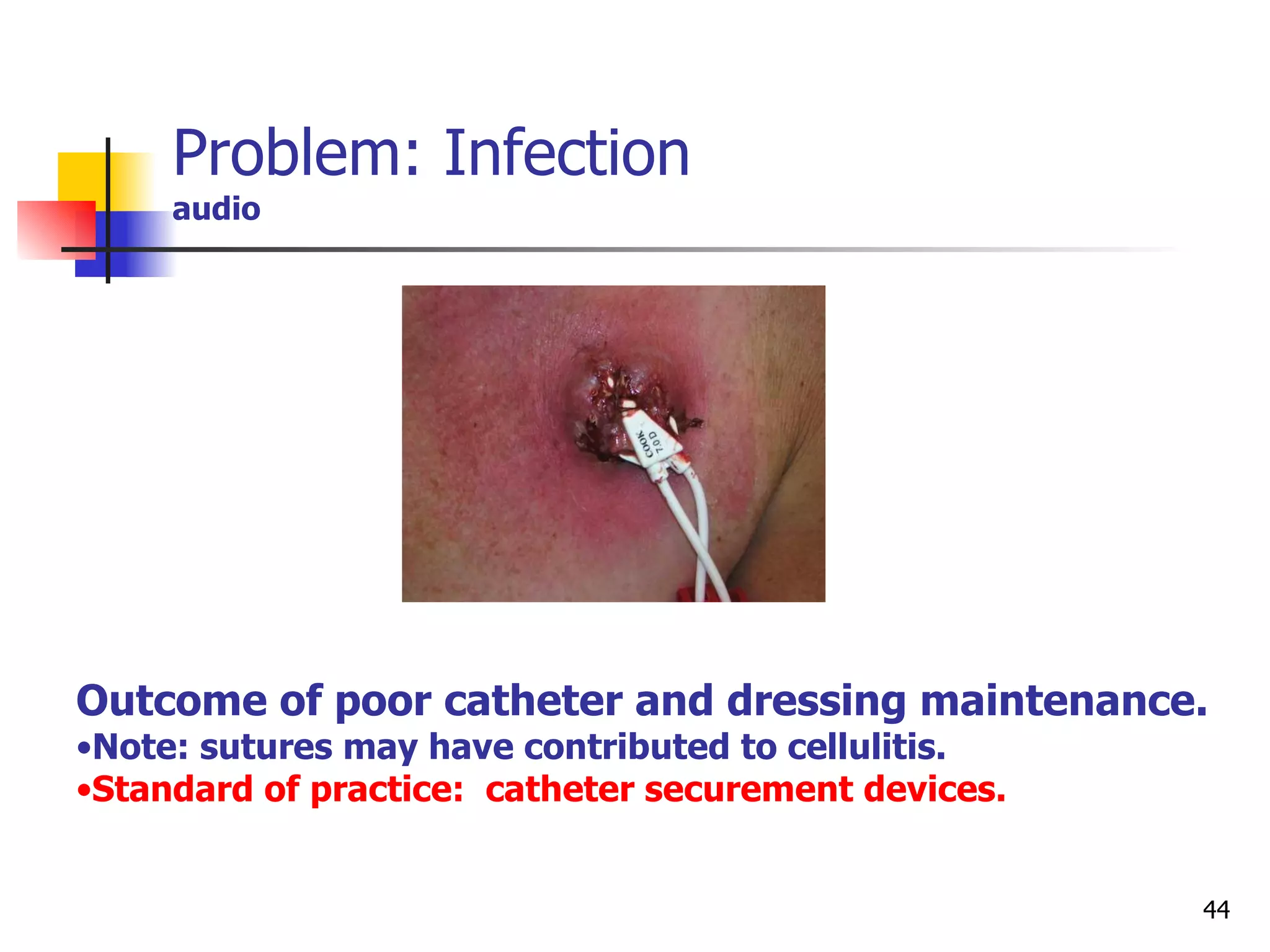
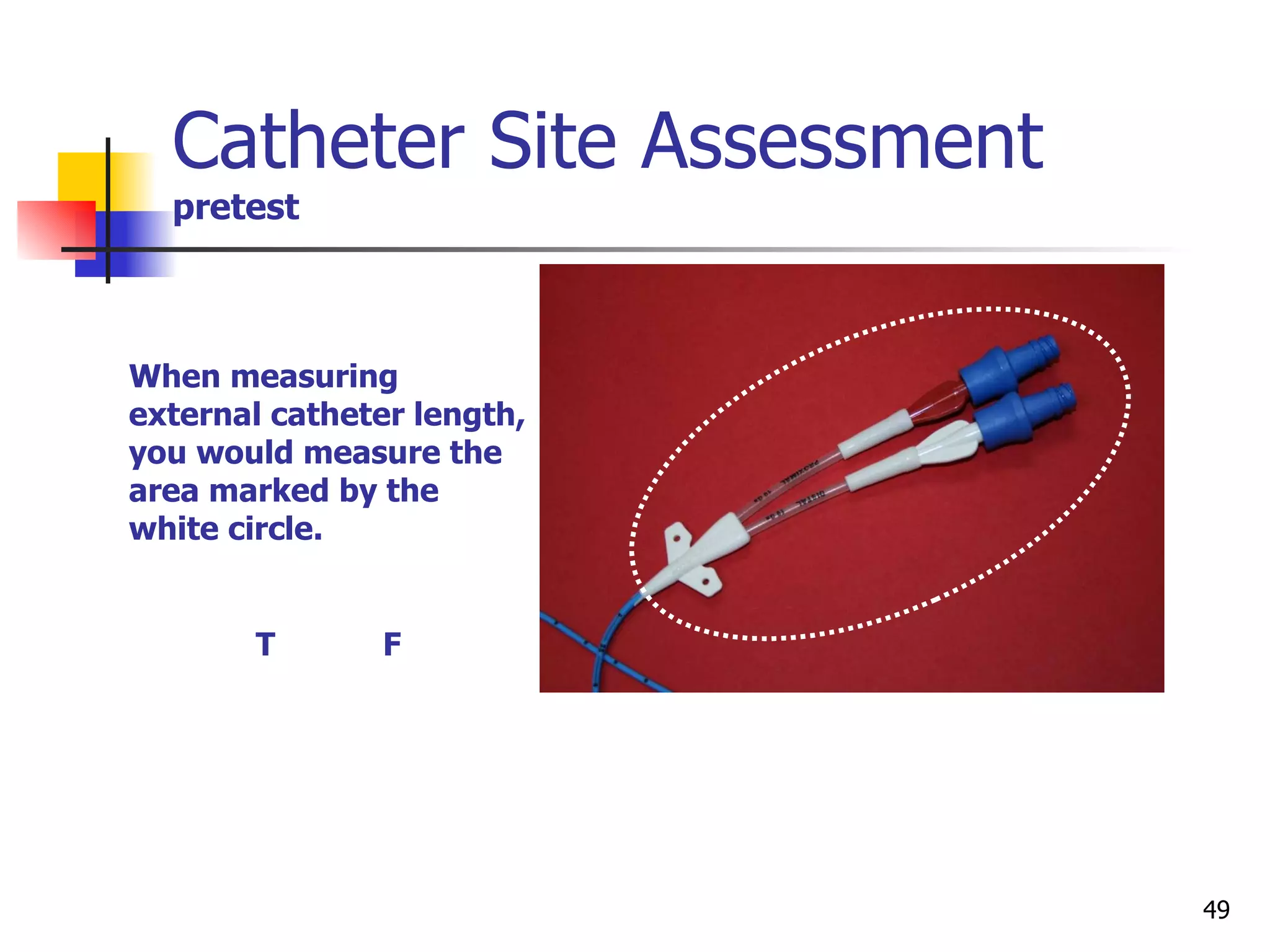
This document discusses proper vascular access device care and prevention of catheter-related infections. It emphasizes that standardization of care practices like hand hygiene, maximal barrier precautions during insertion, and disinfecting catheter hubs can significantly reduce infections. It also explains the risks of biofilm formation on devices and how microbes within biofilms are highly resistant to antibiotics. Education of healthcare workers and patients on infection prevention is vital to improving outcomes.