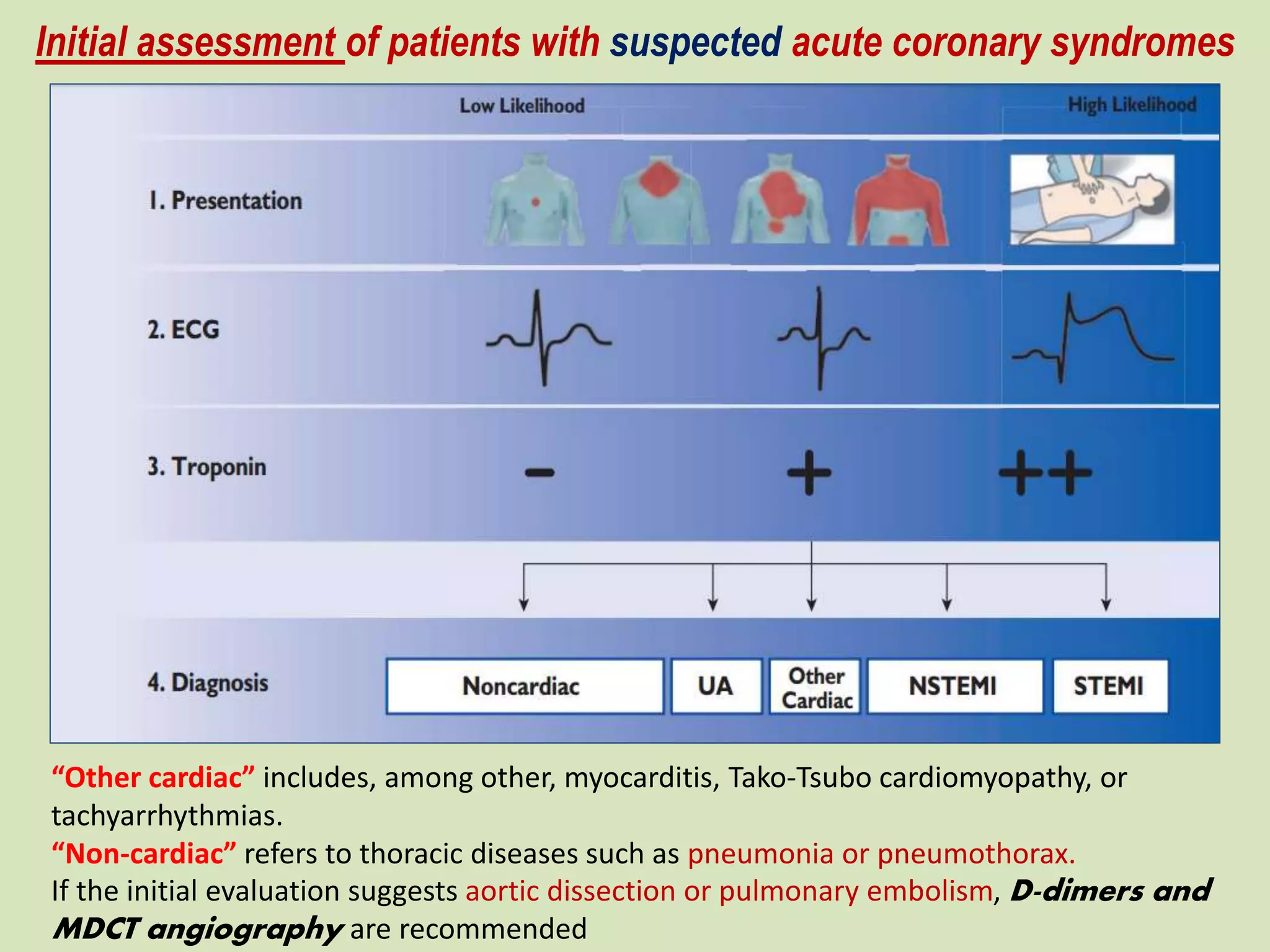
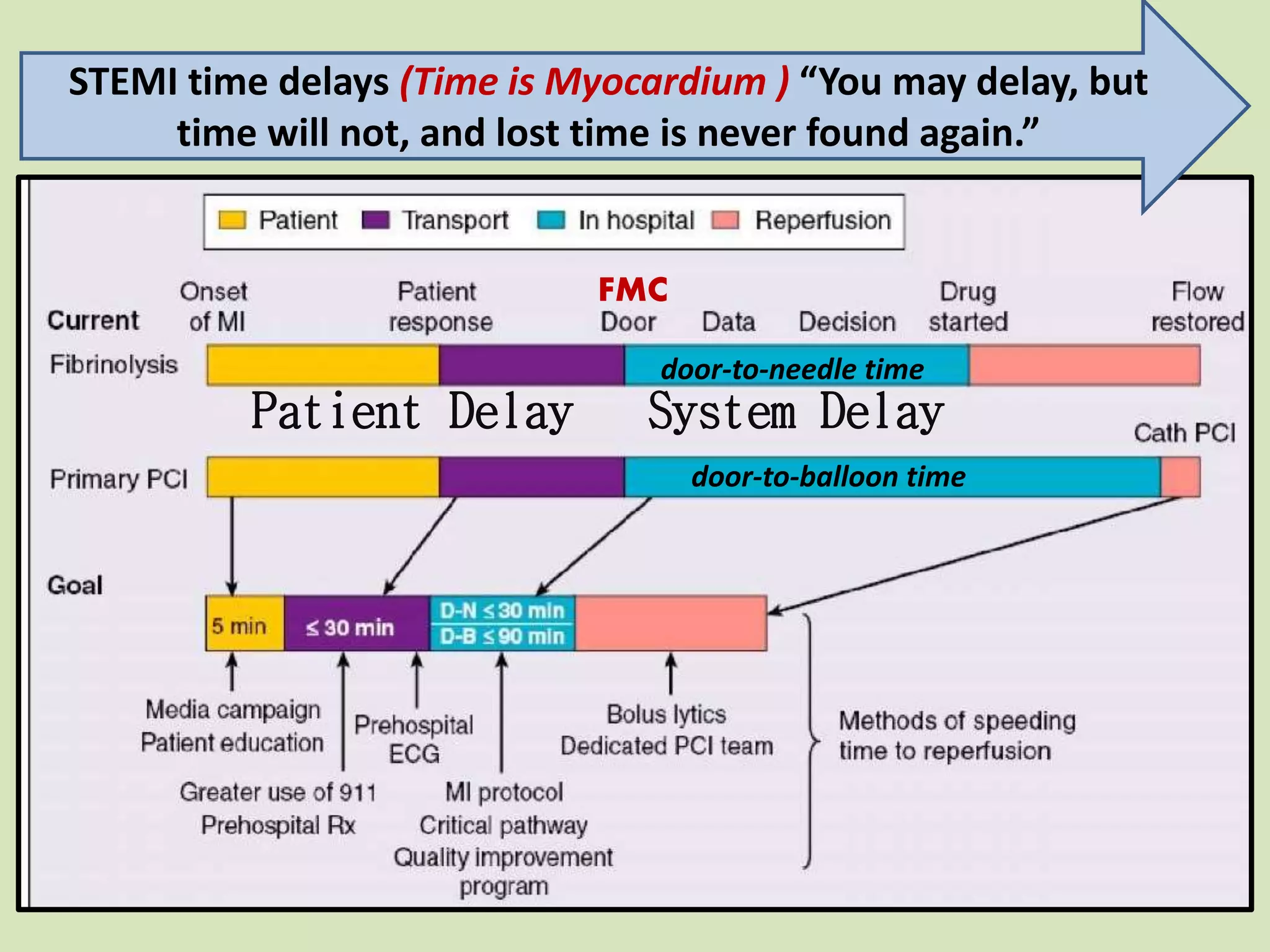
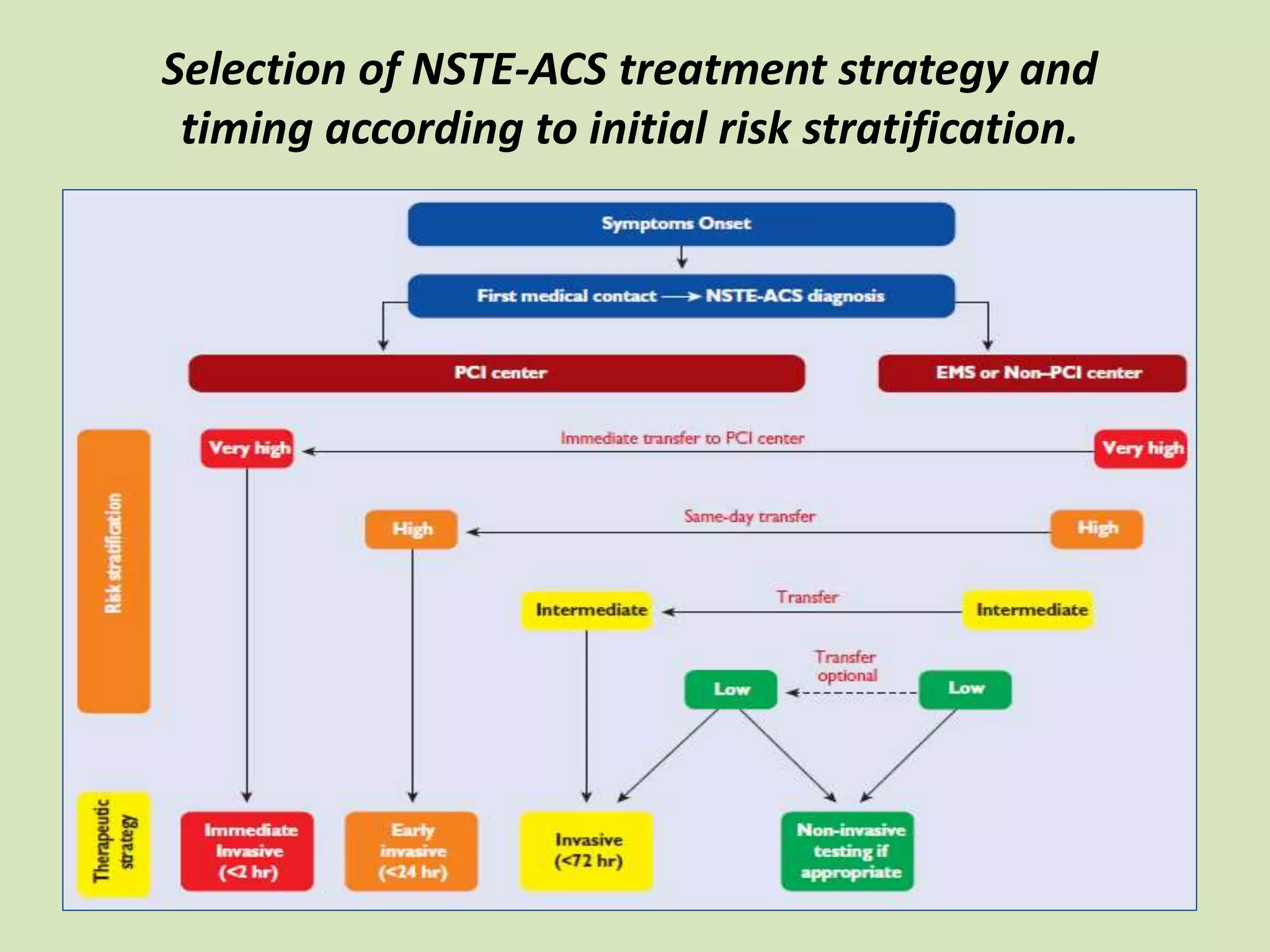
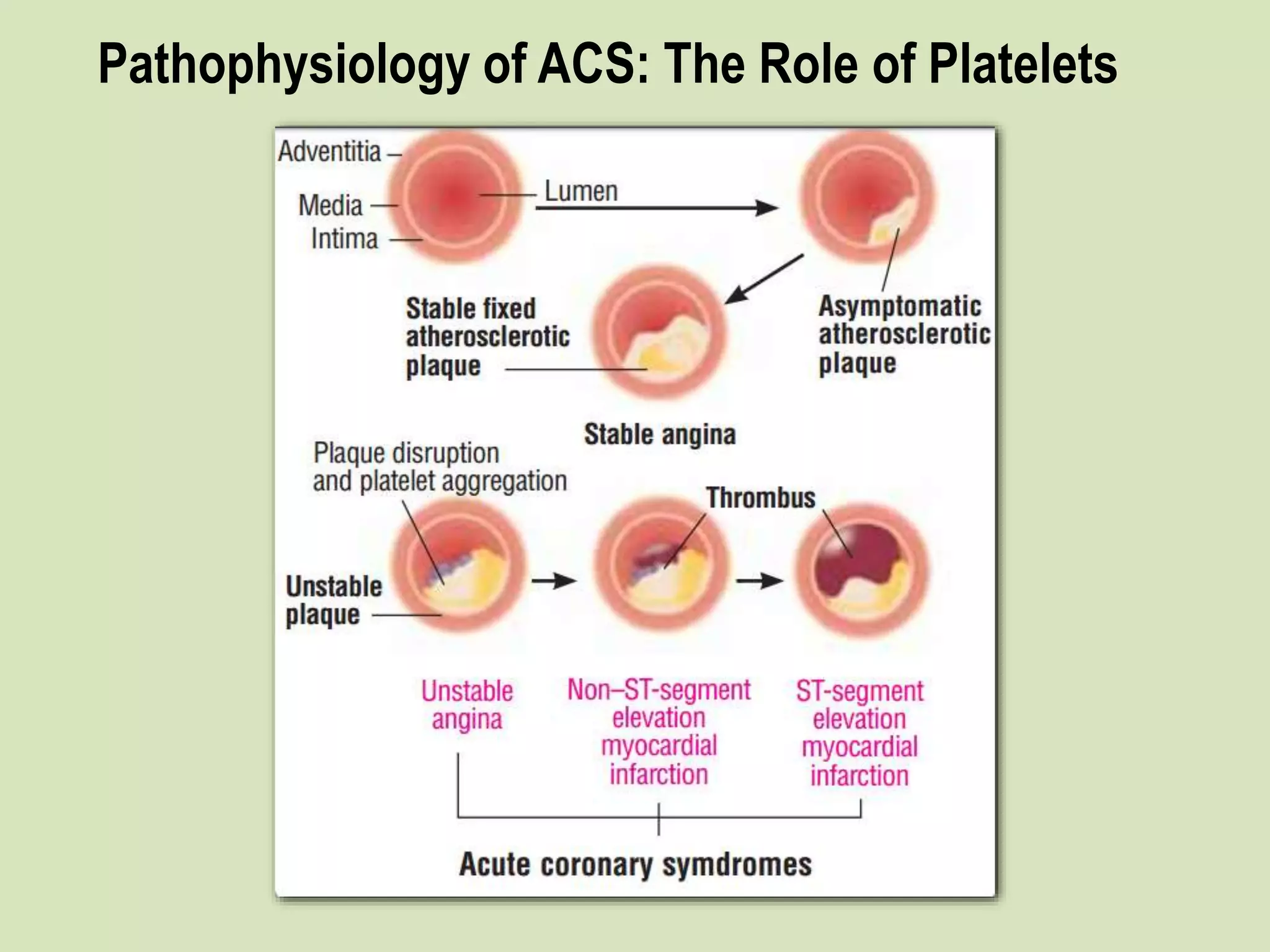
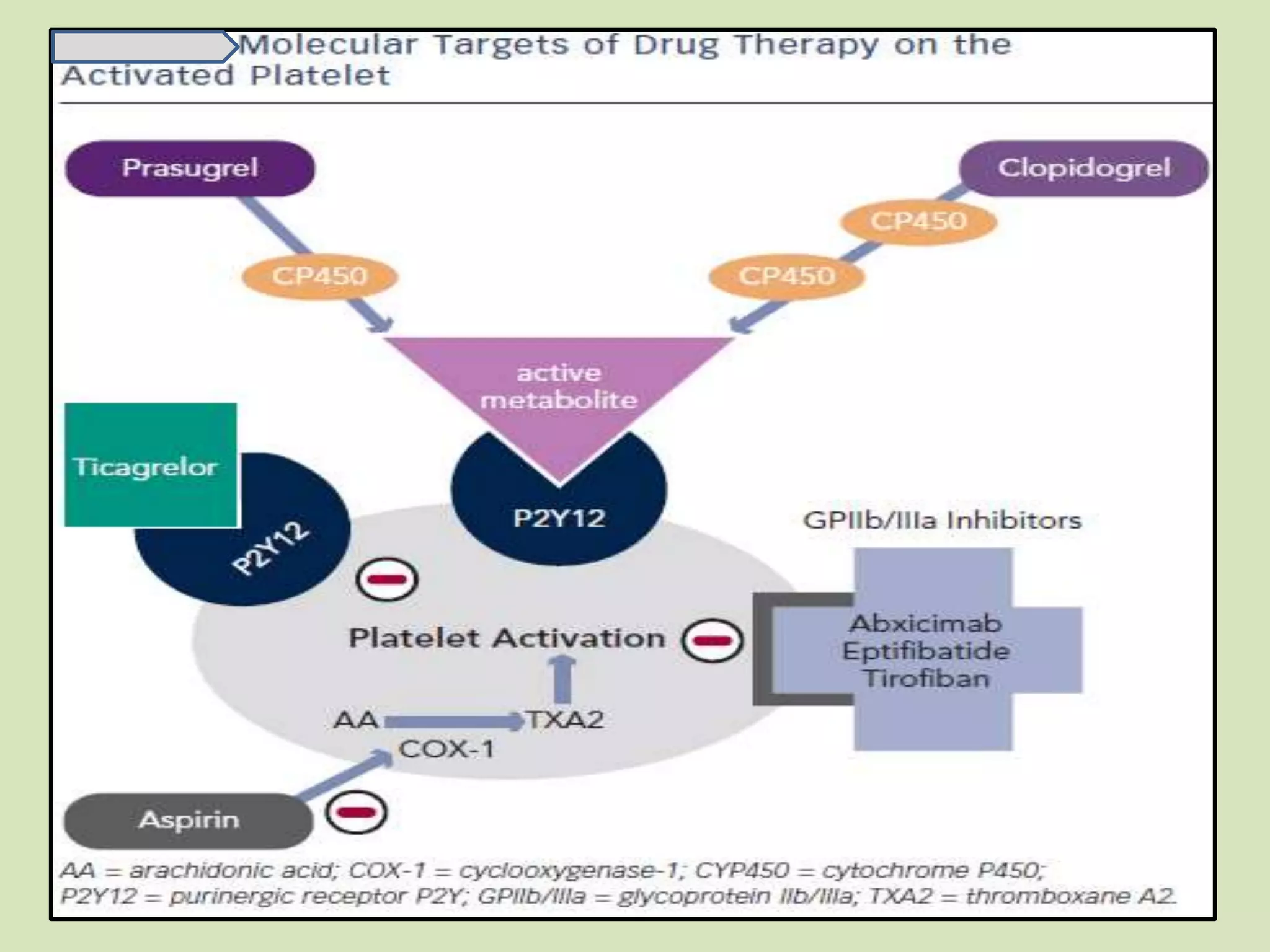
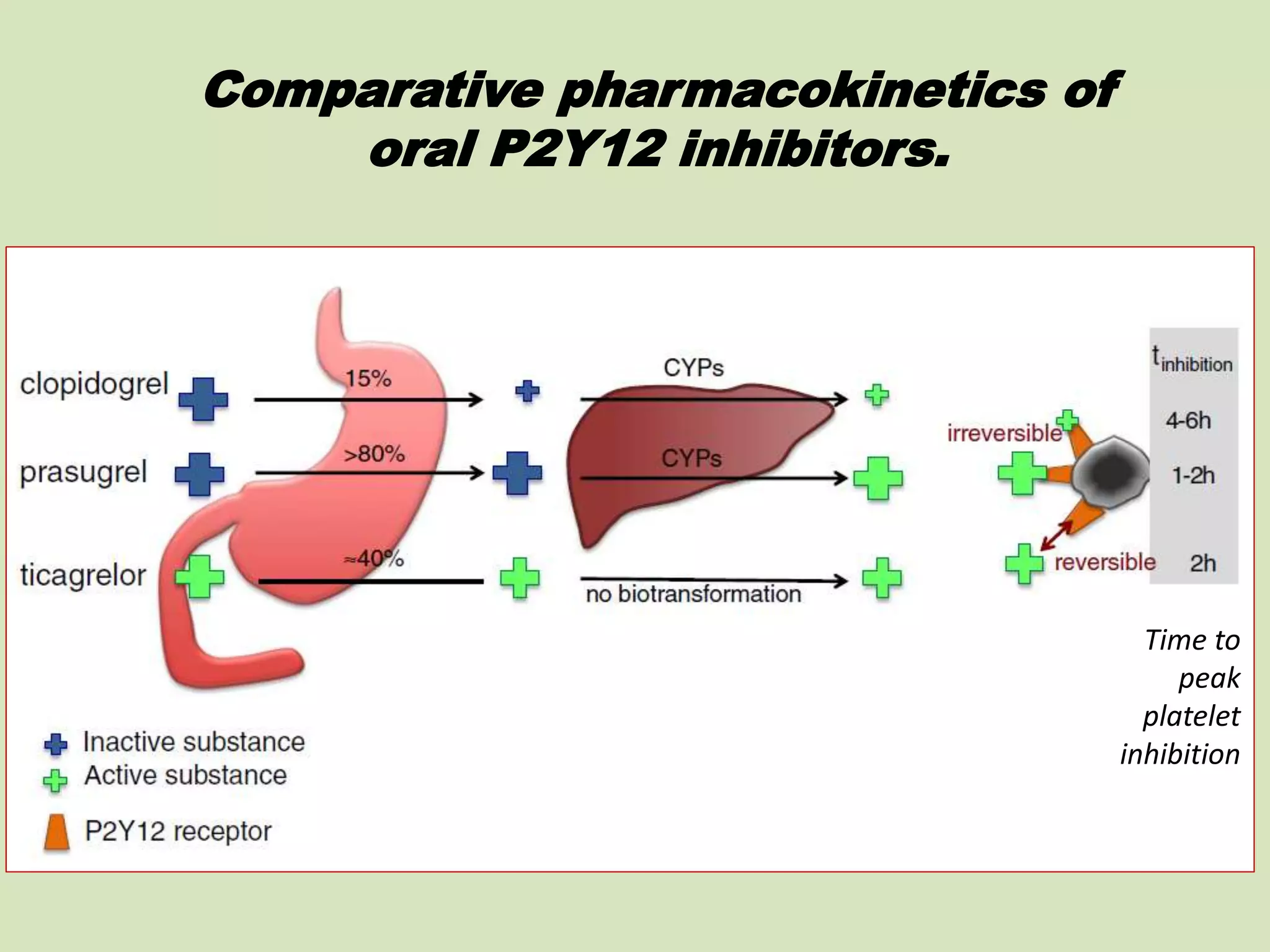
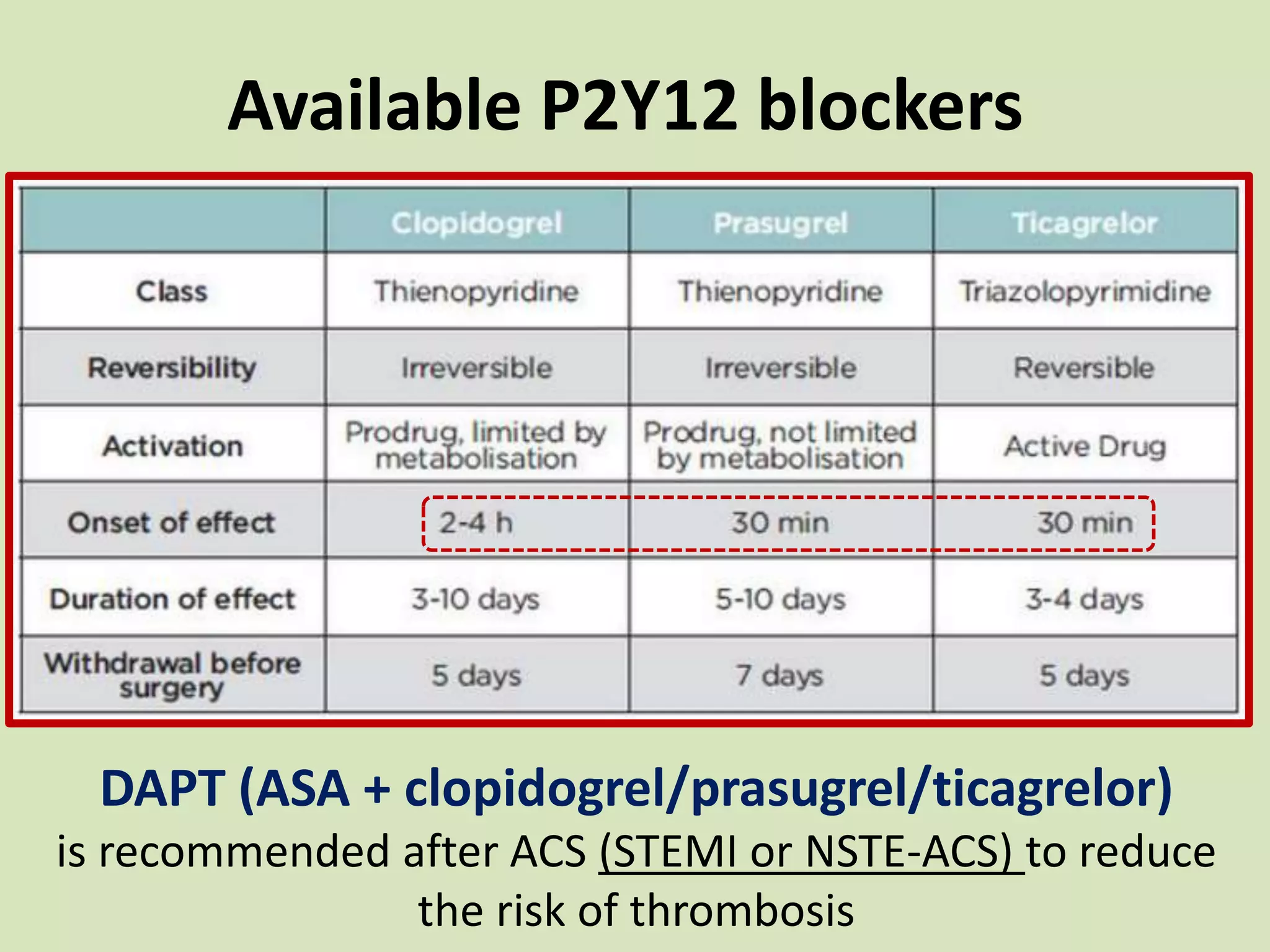
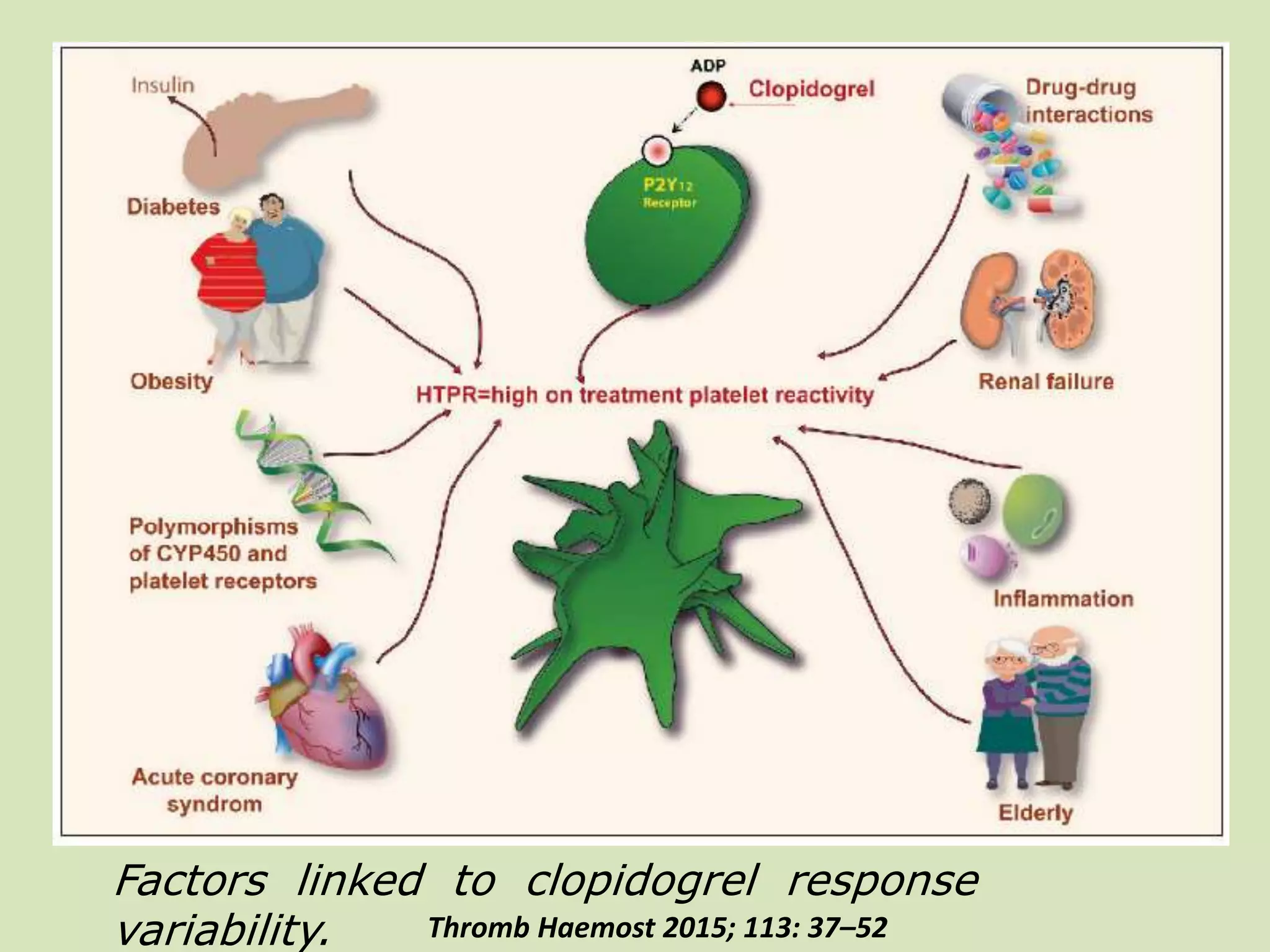
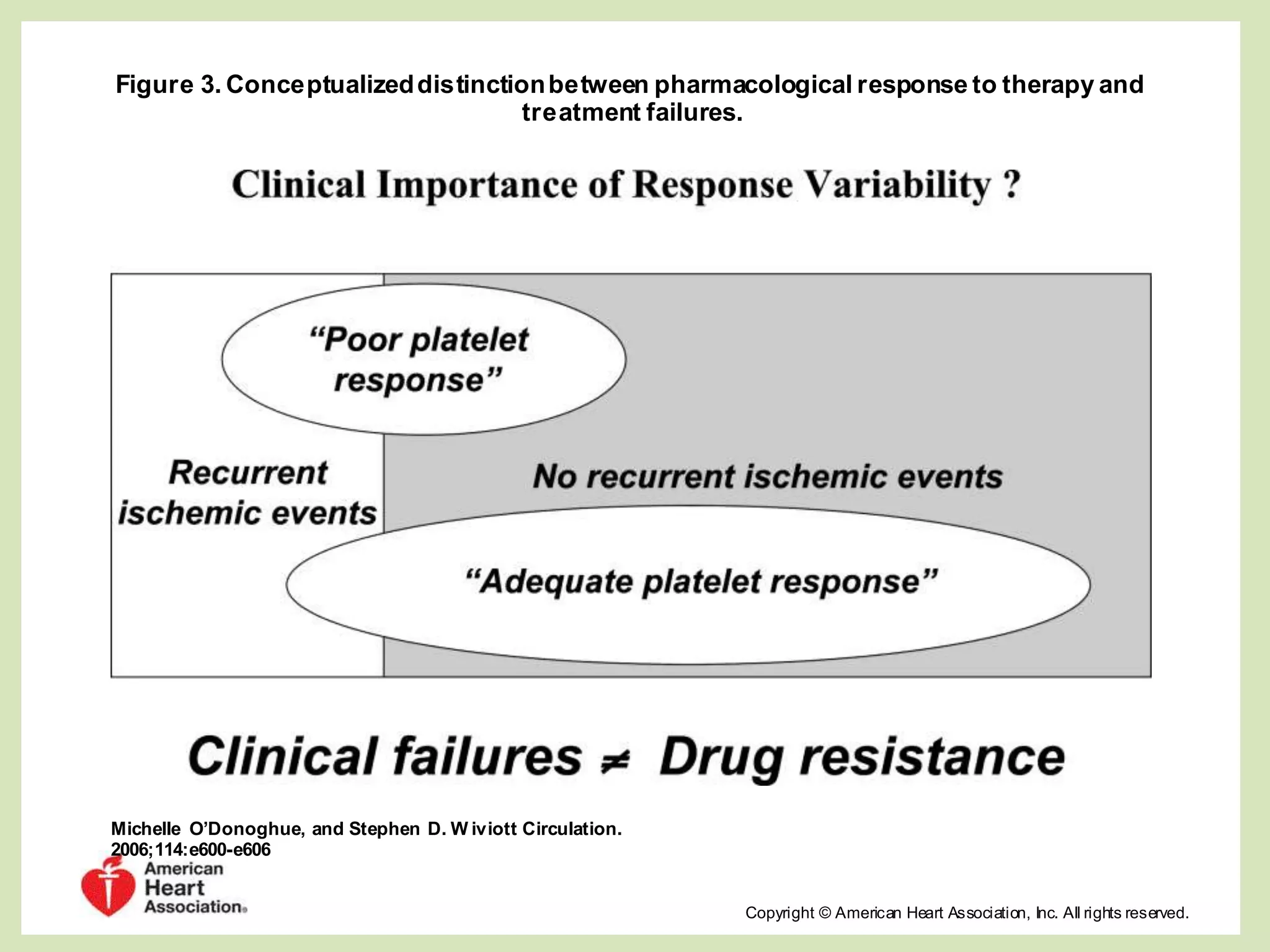
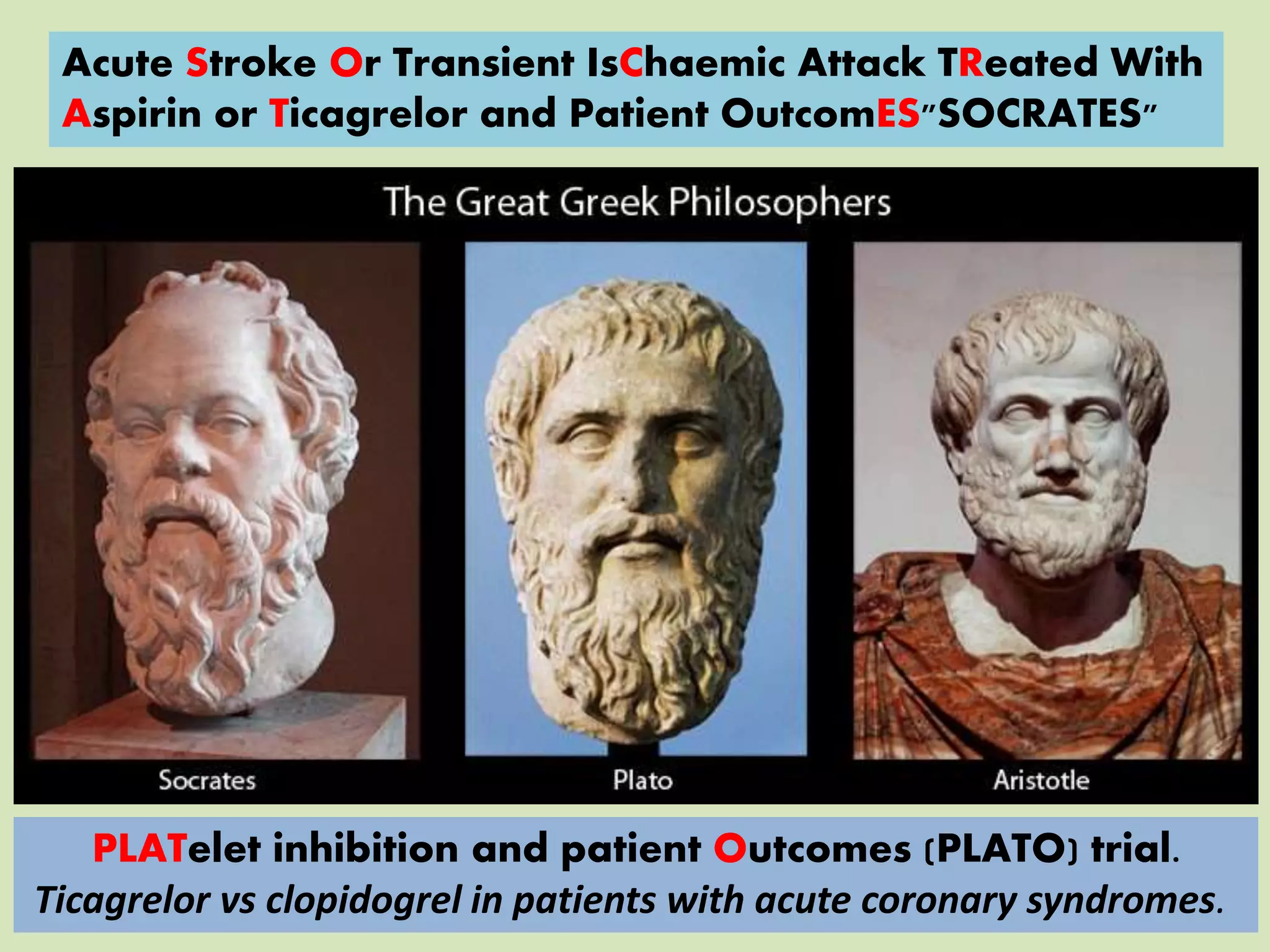
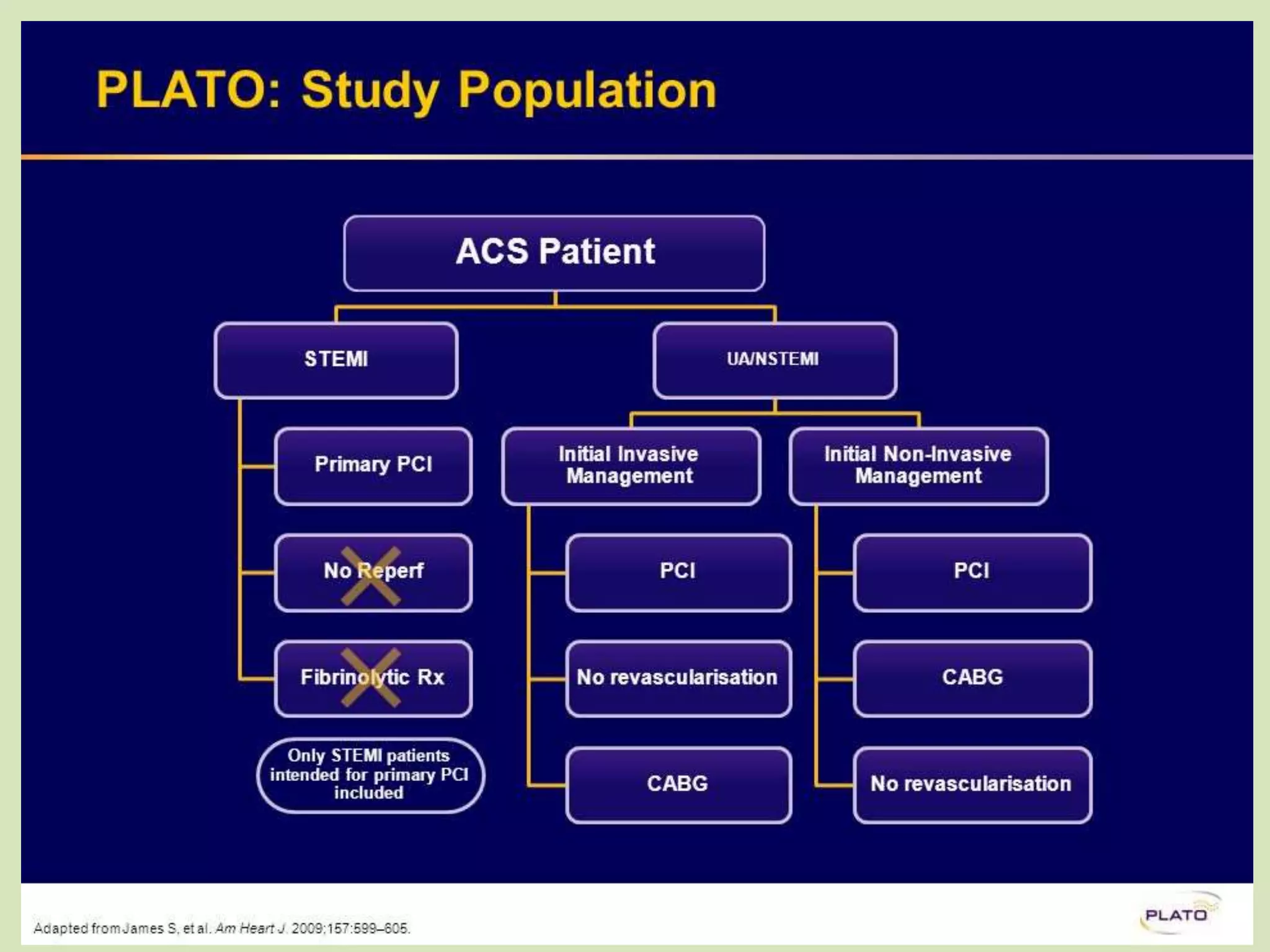
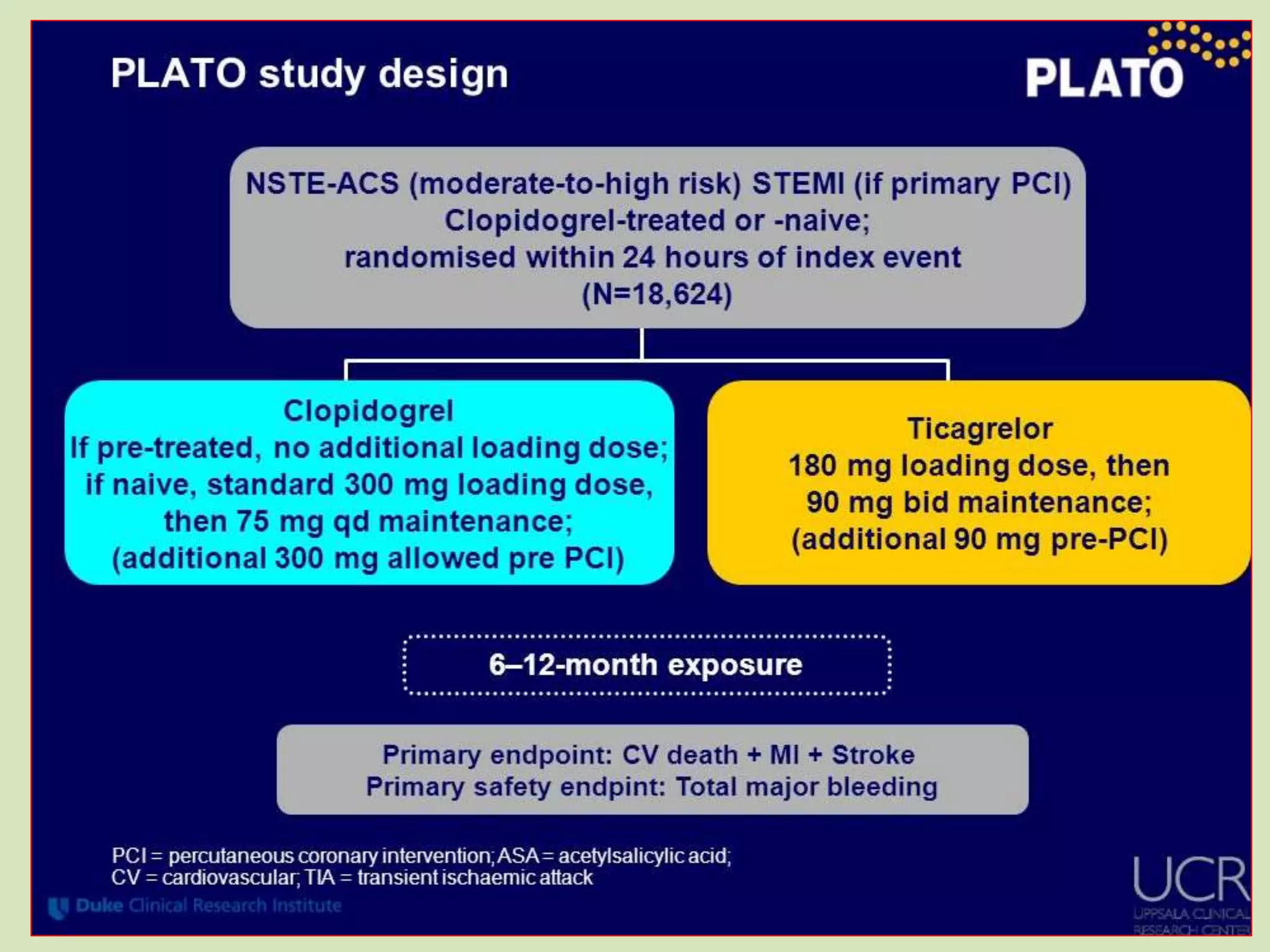
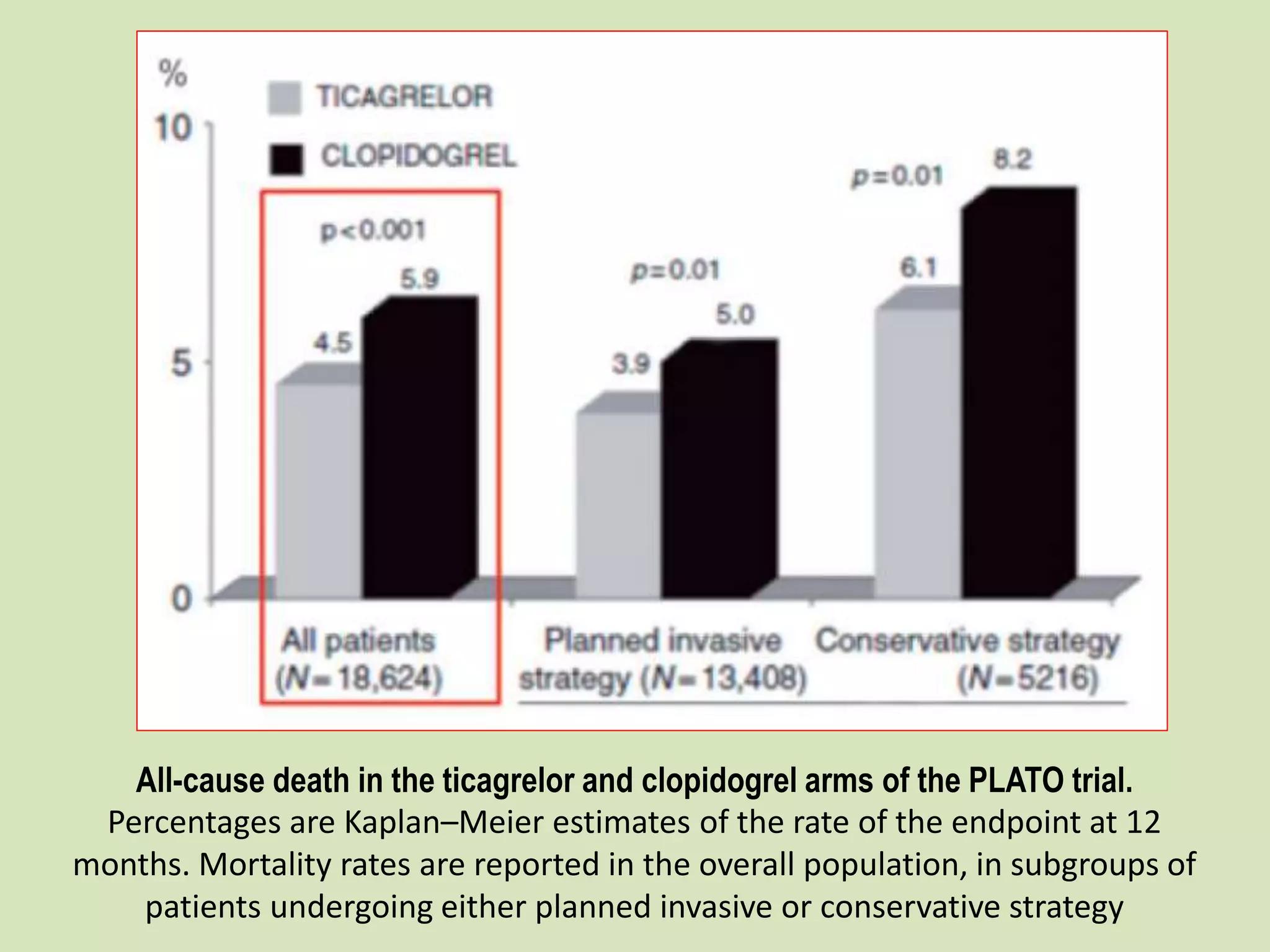
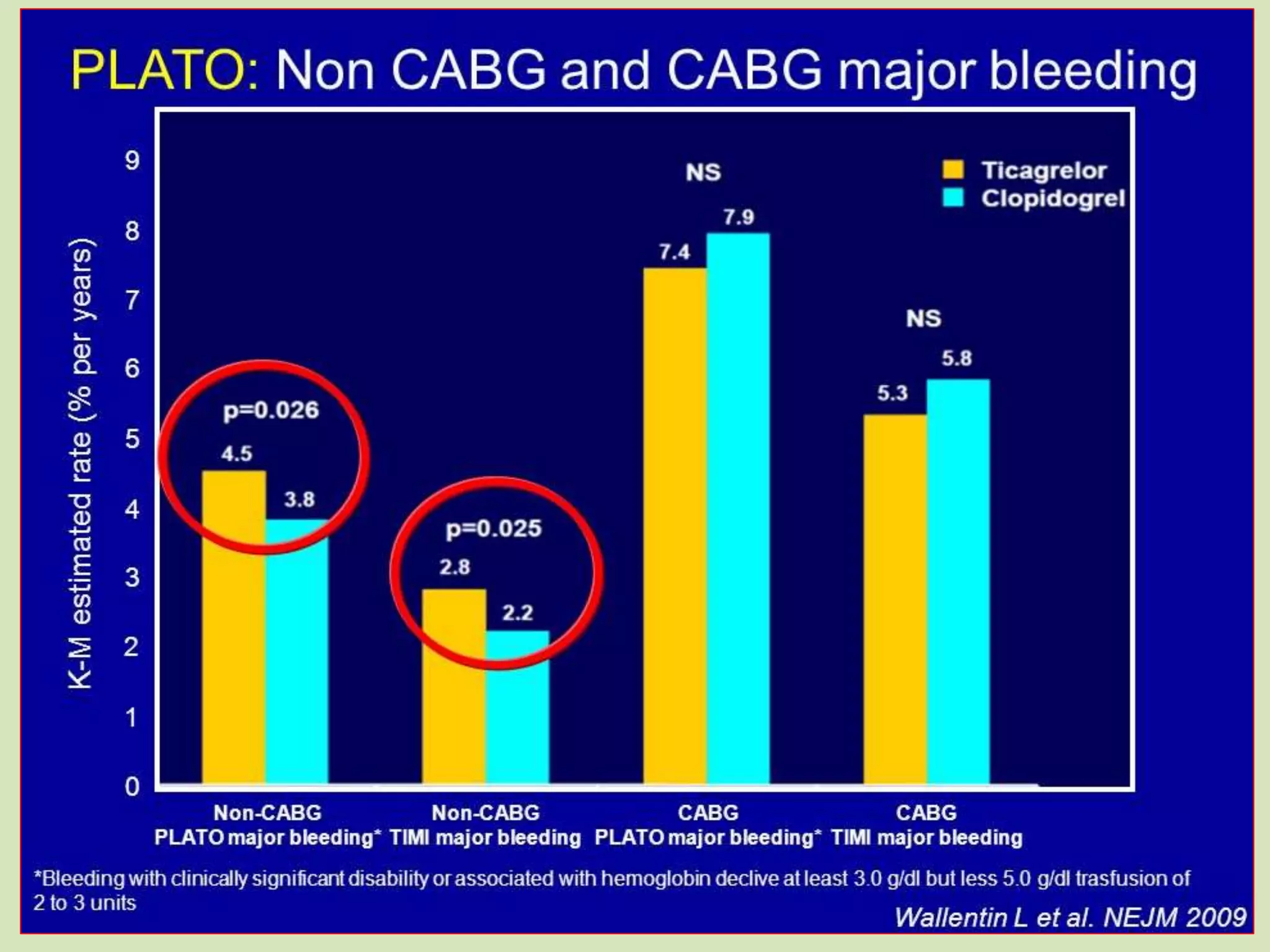
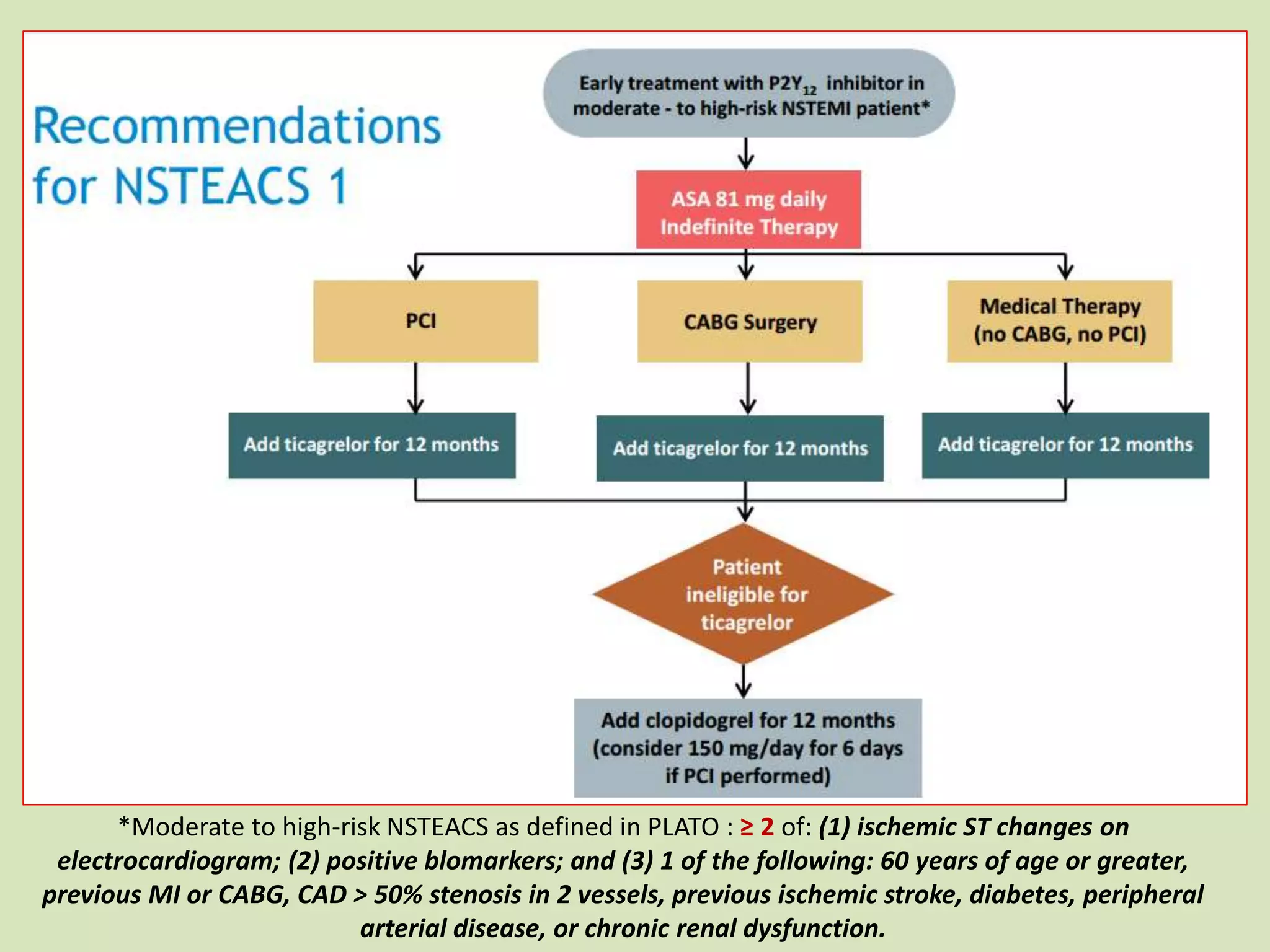
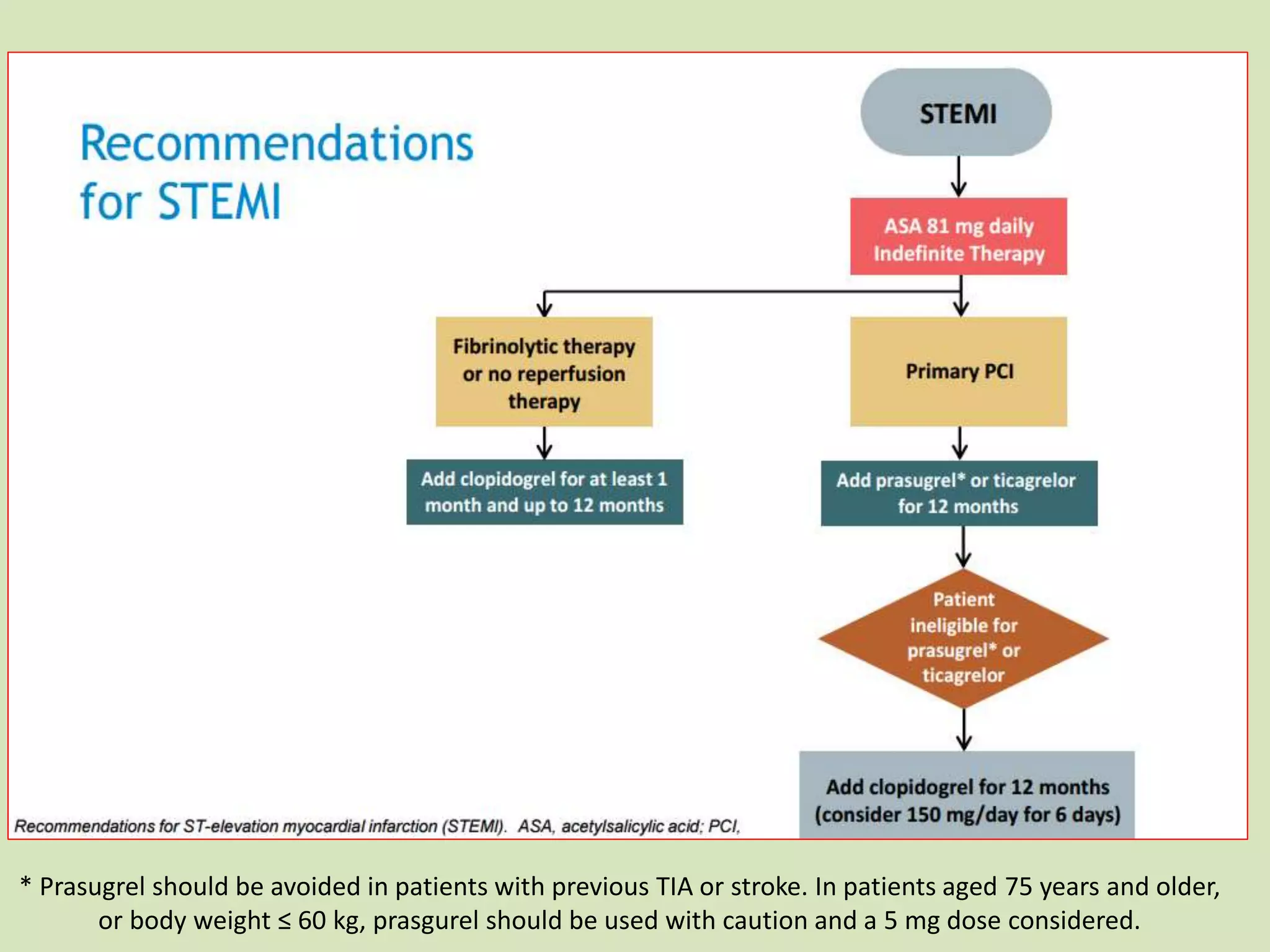
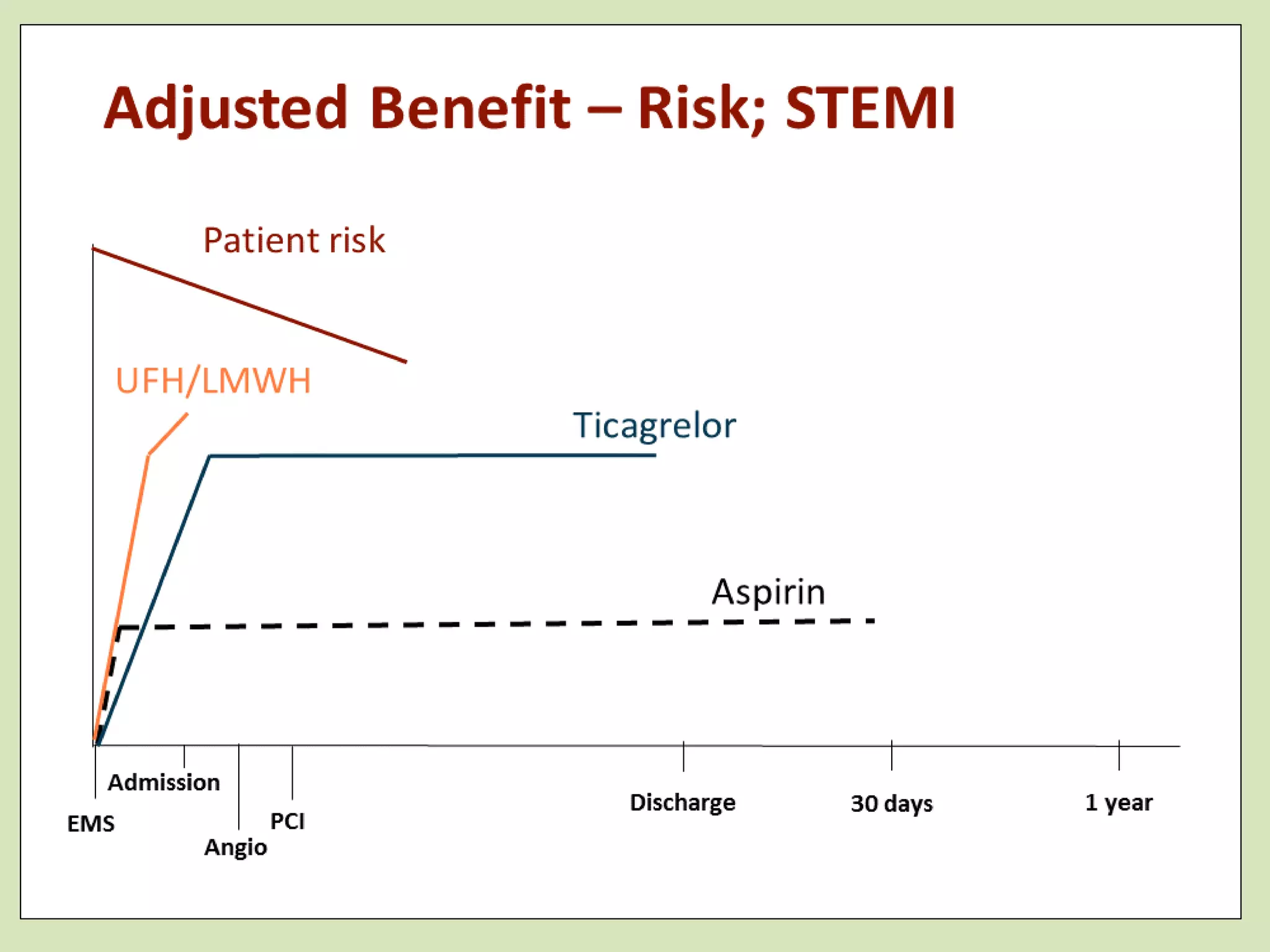
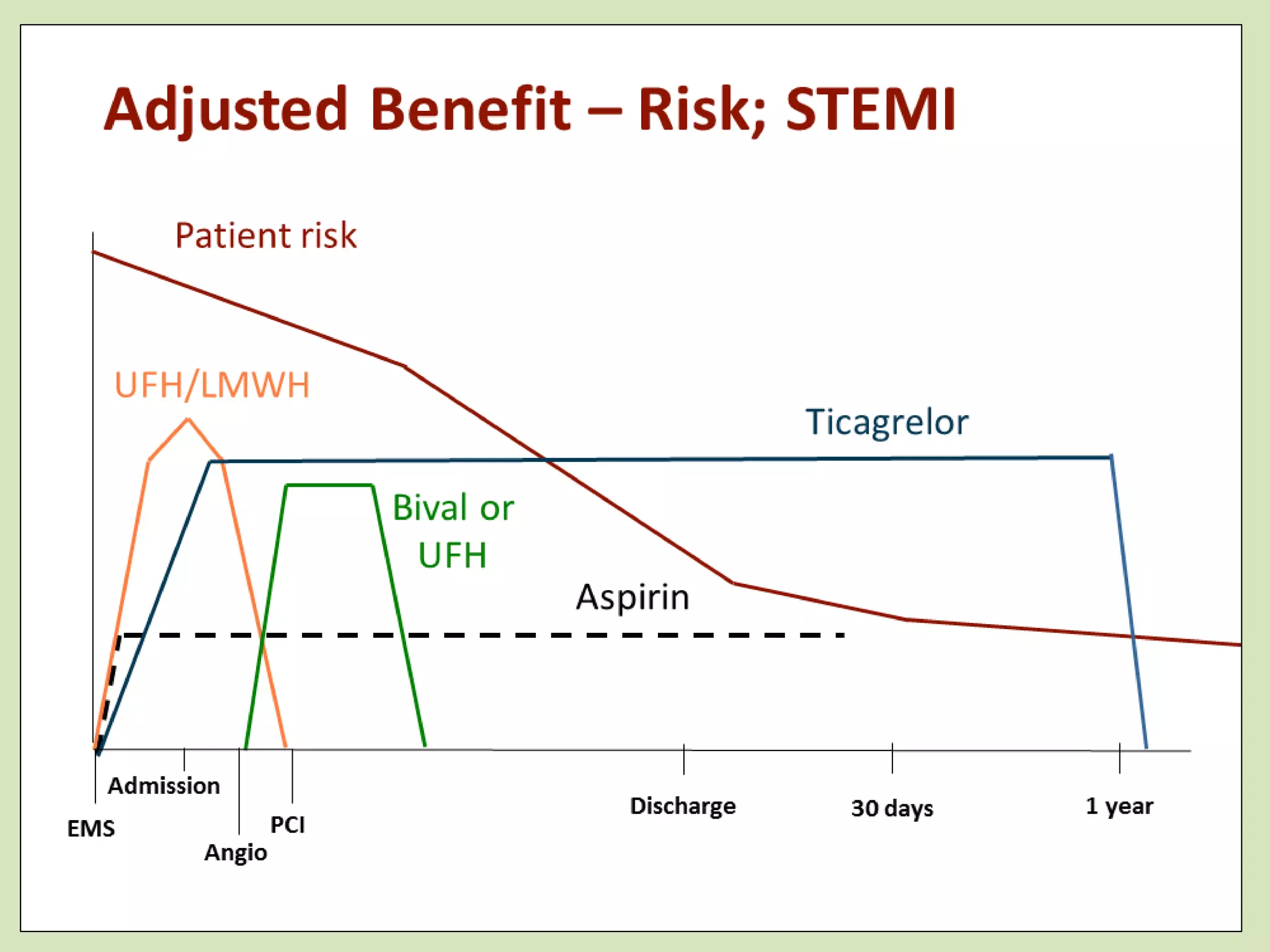
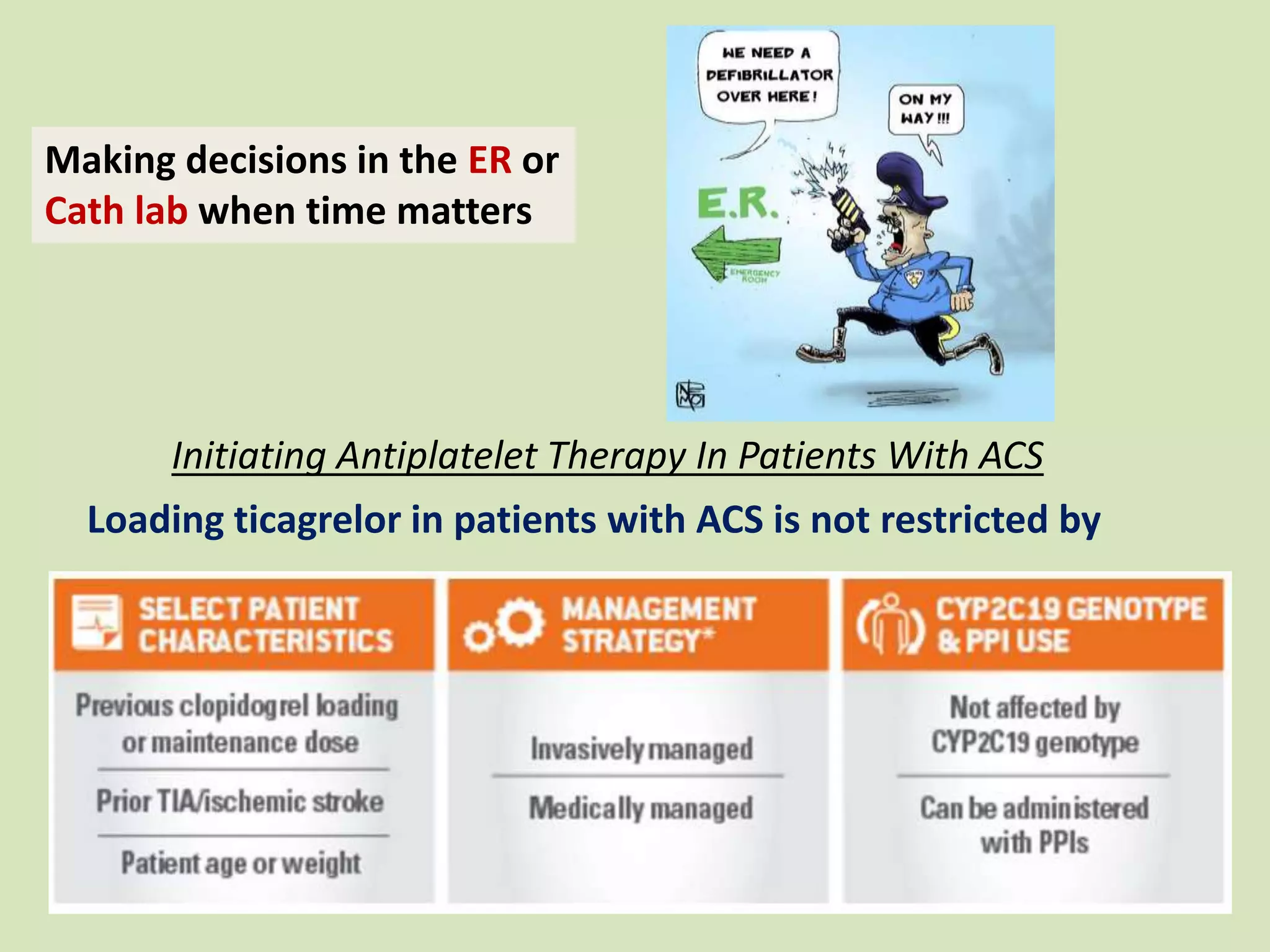
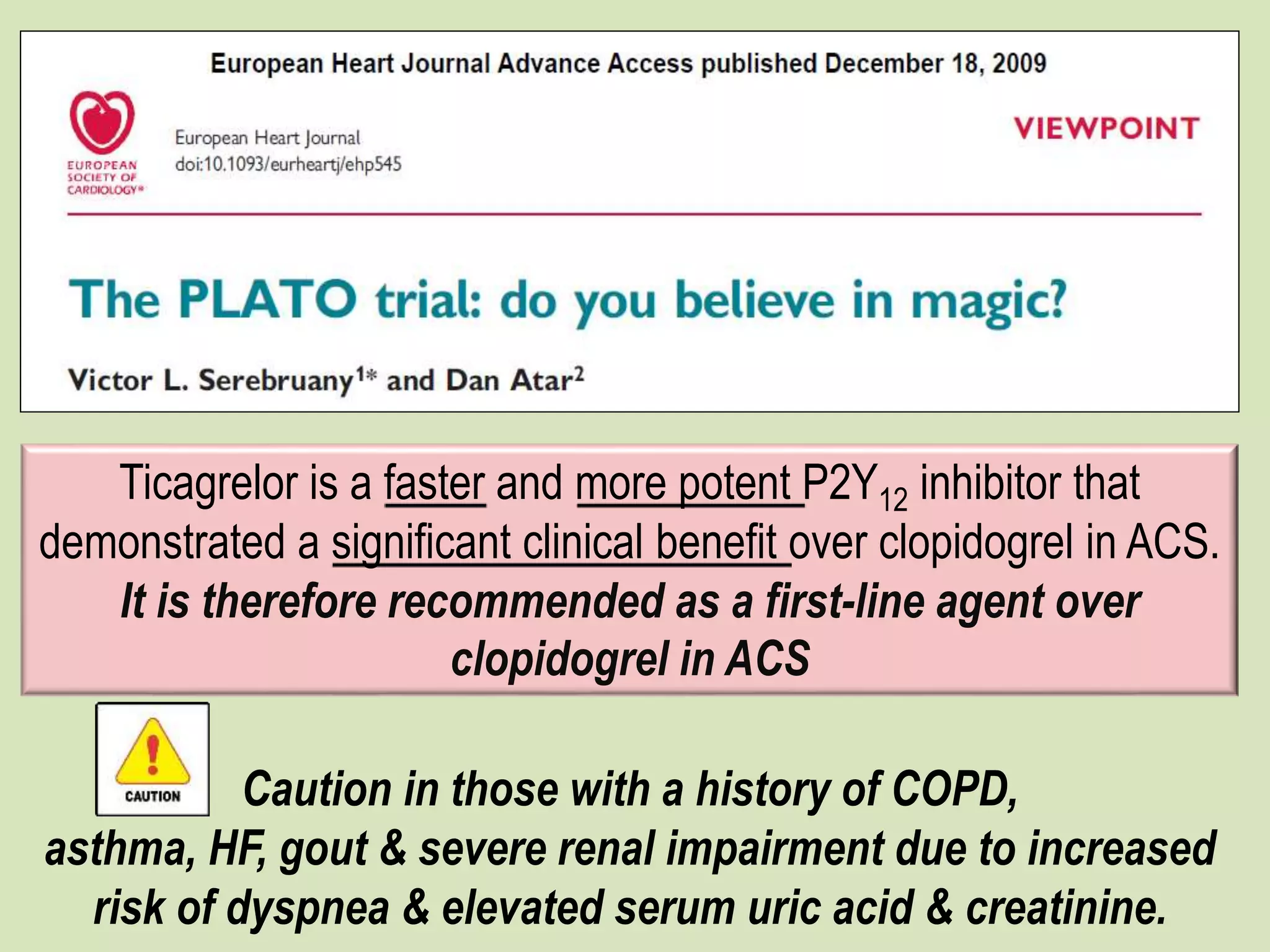
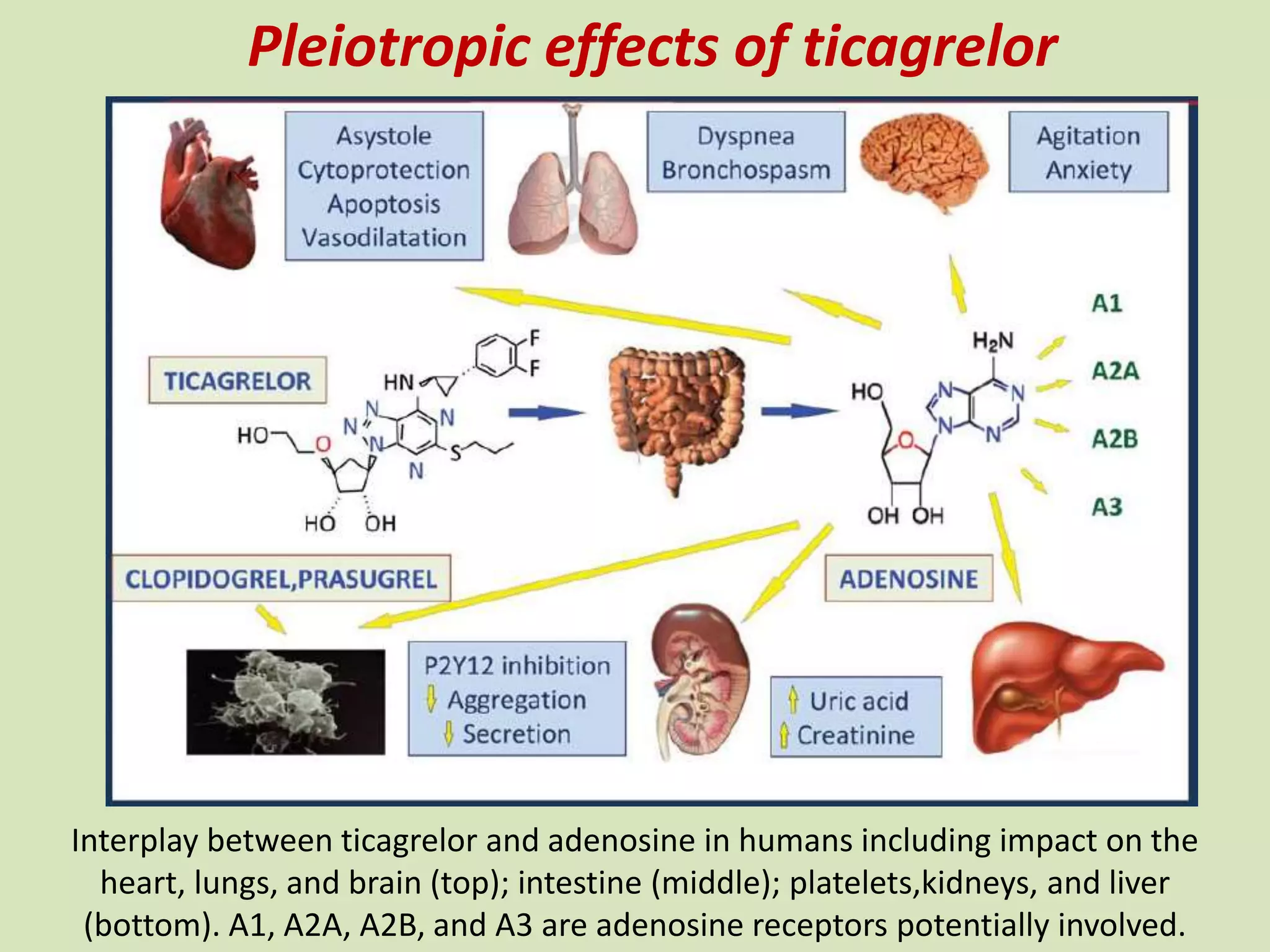
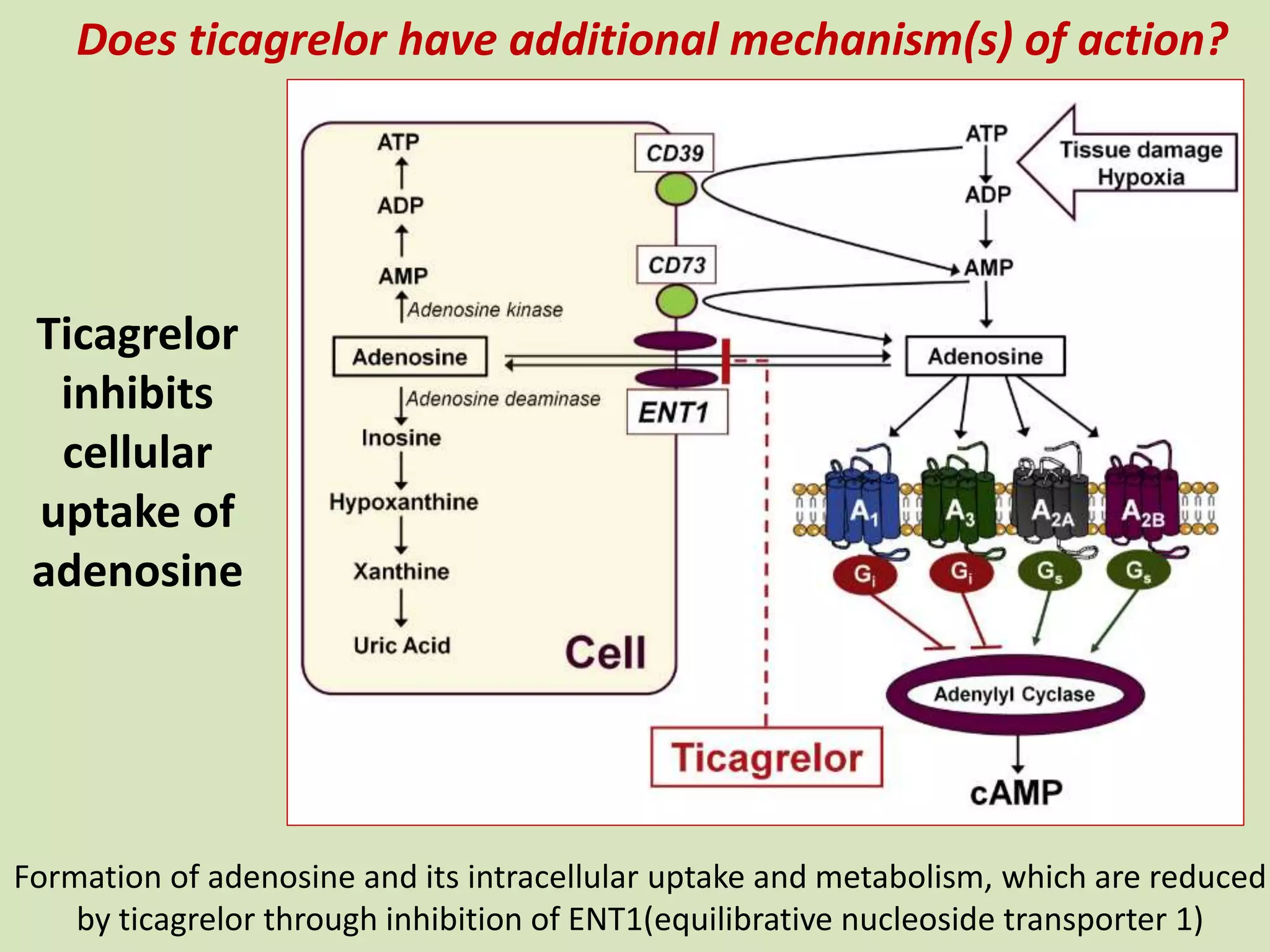
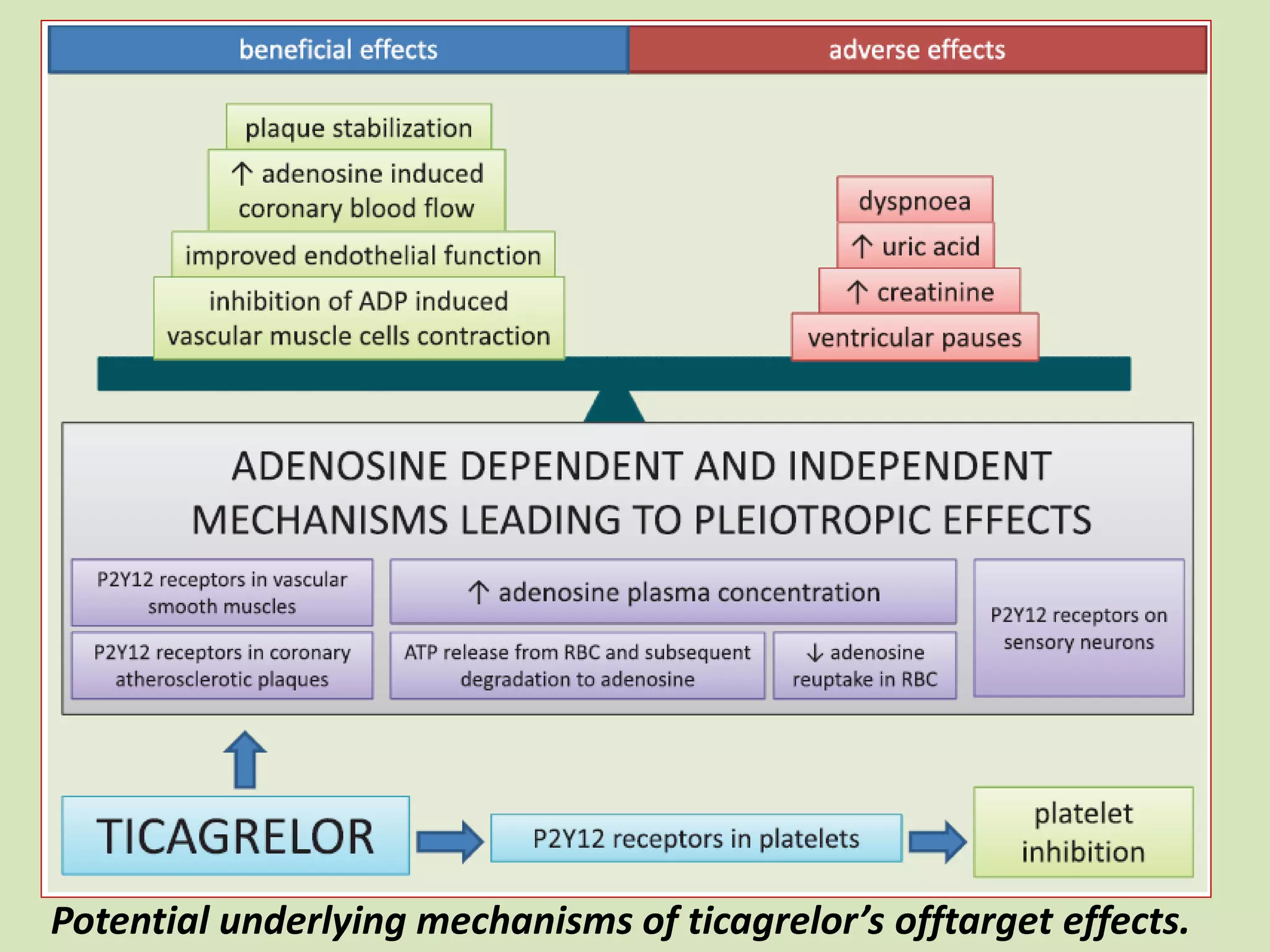
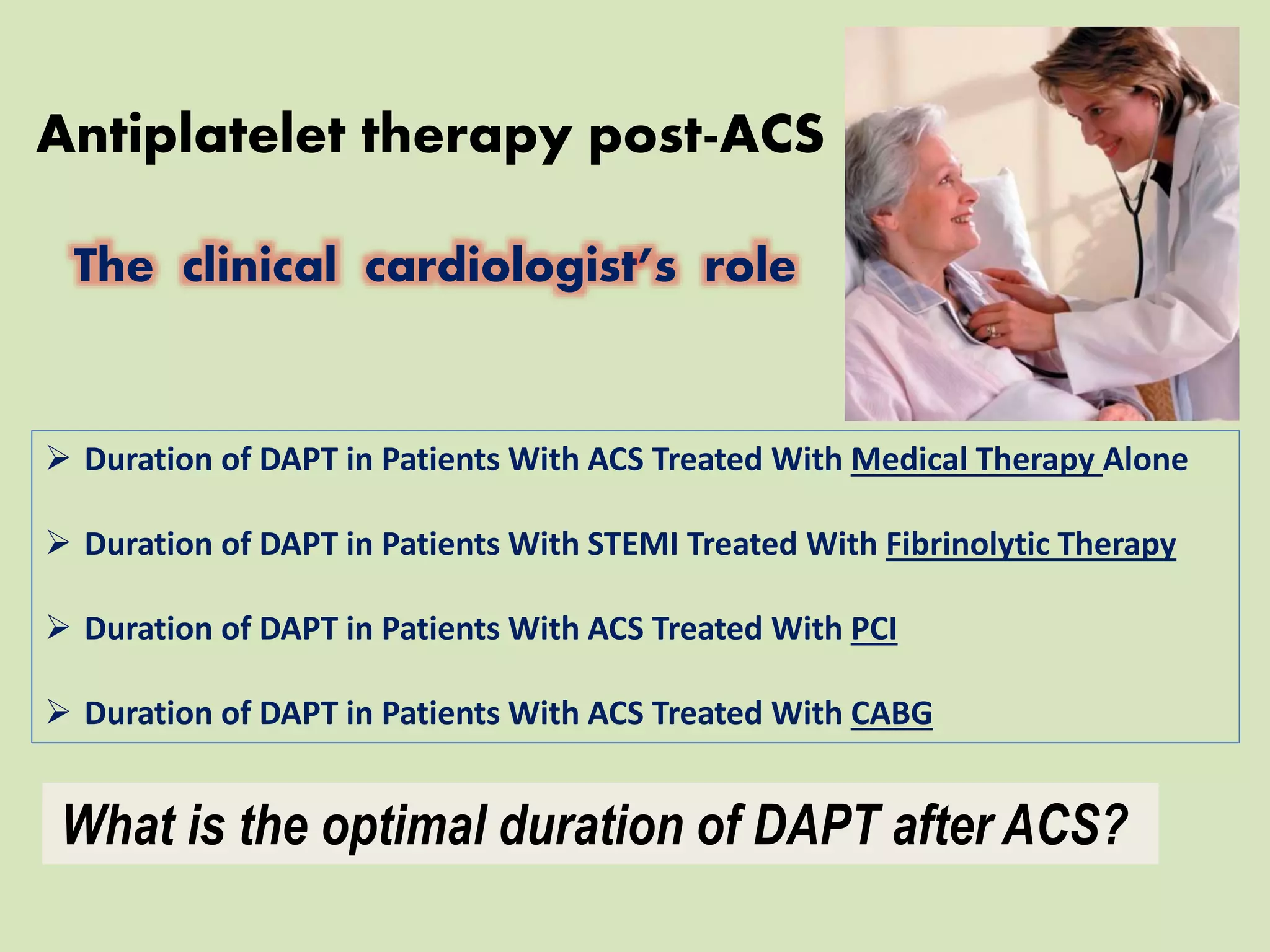
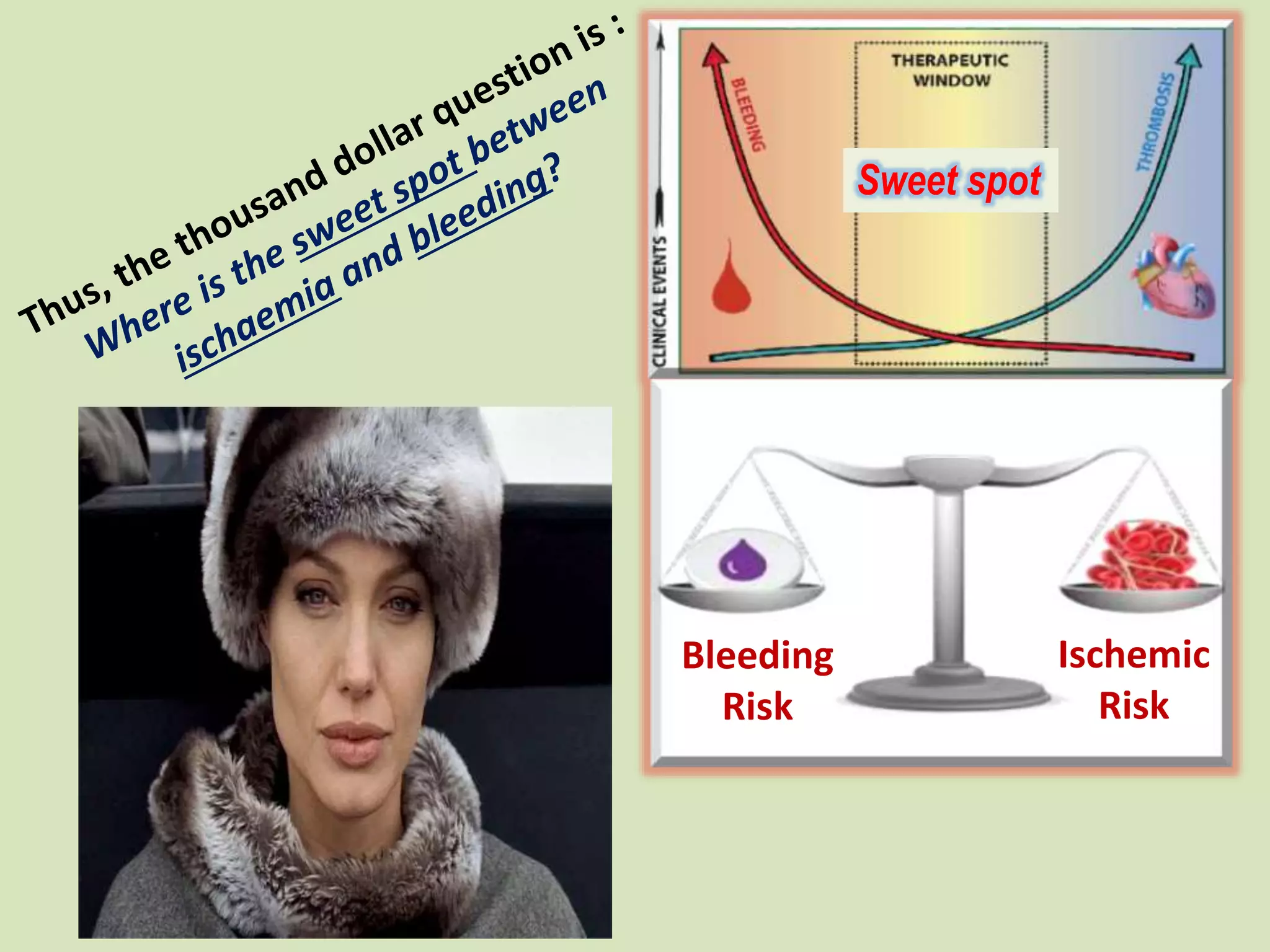
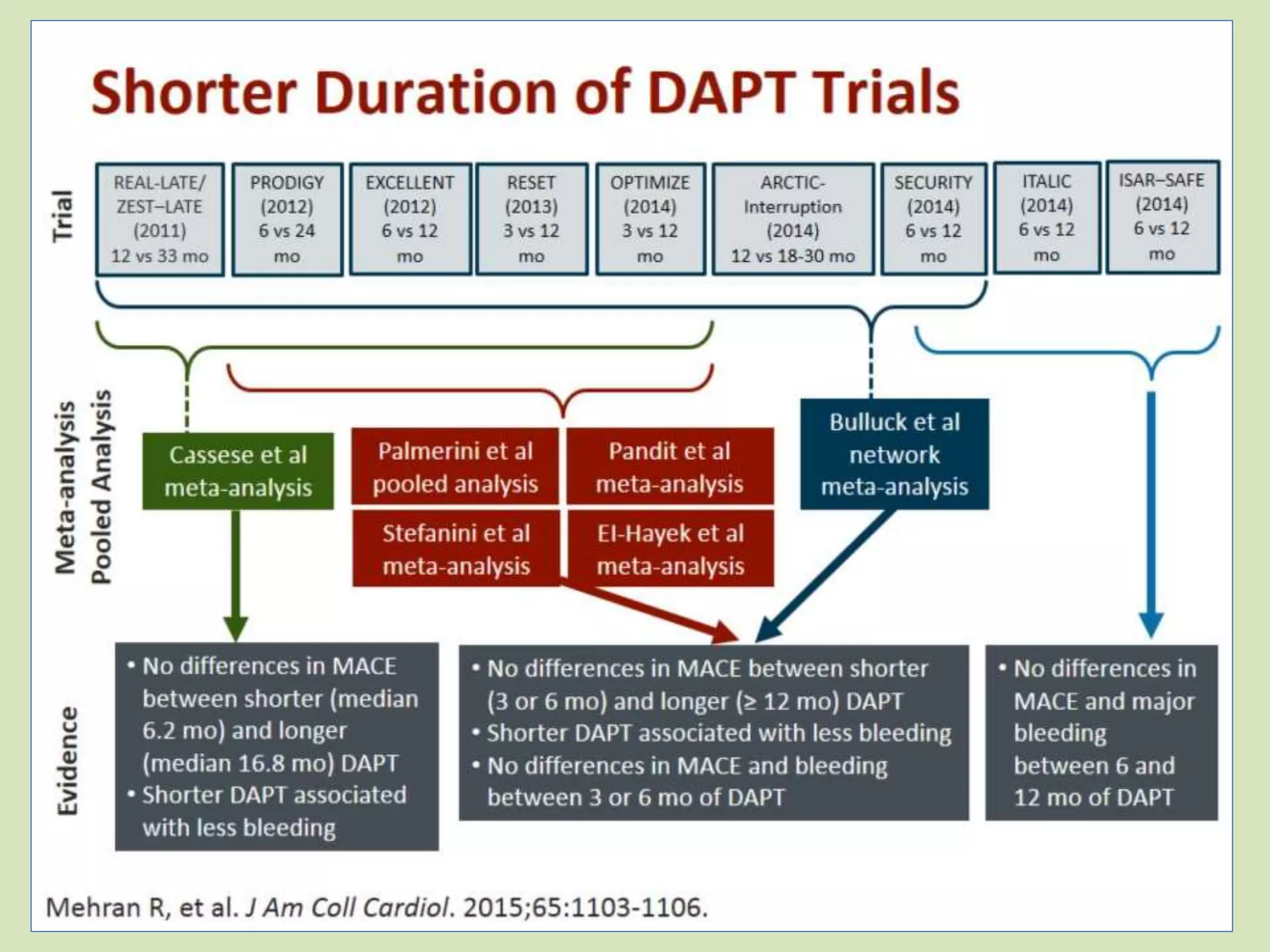
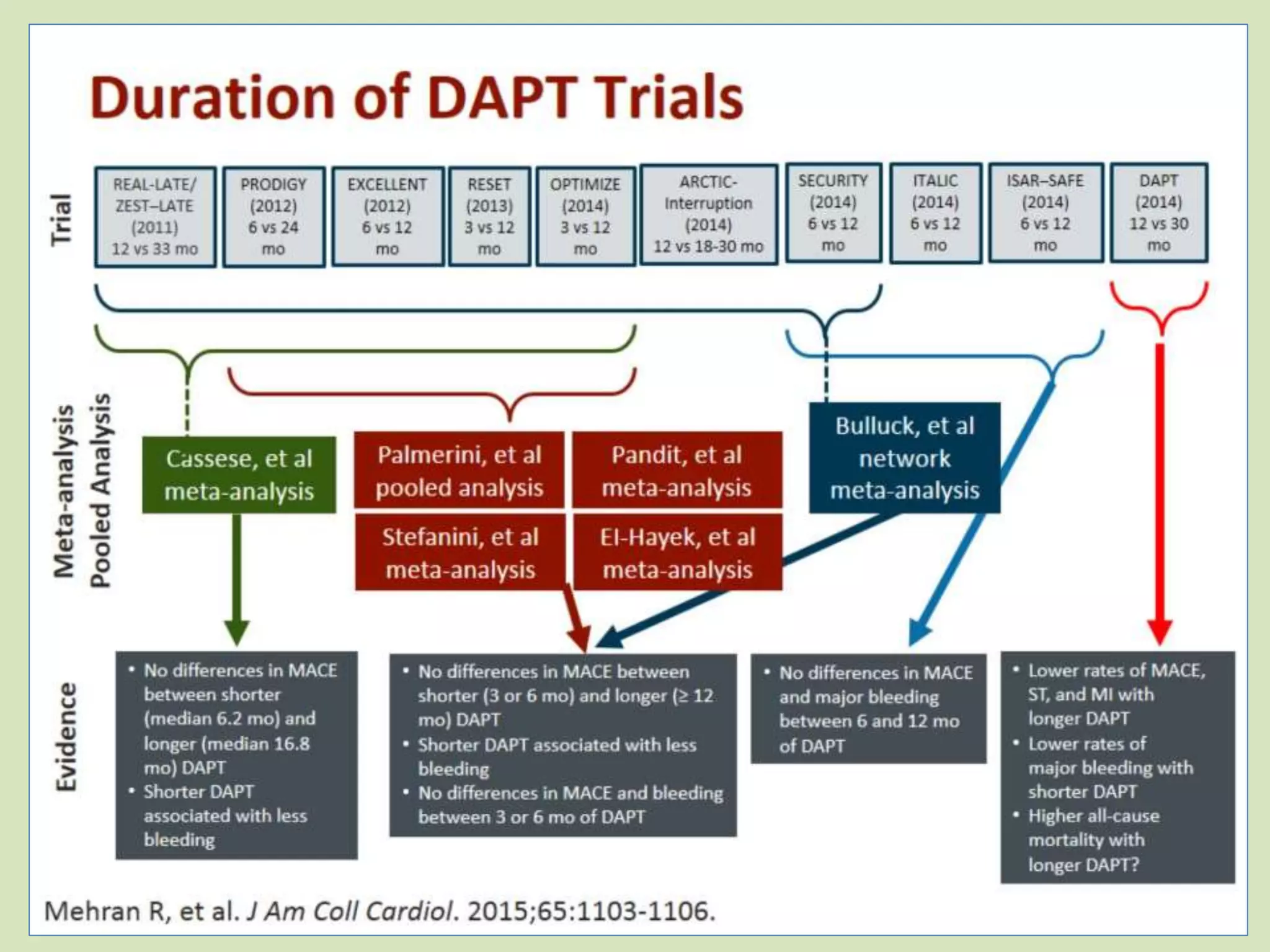
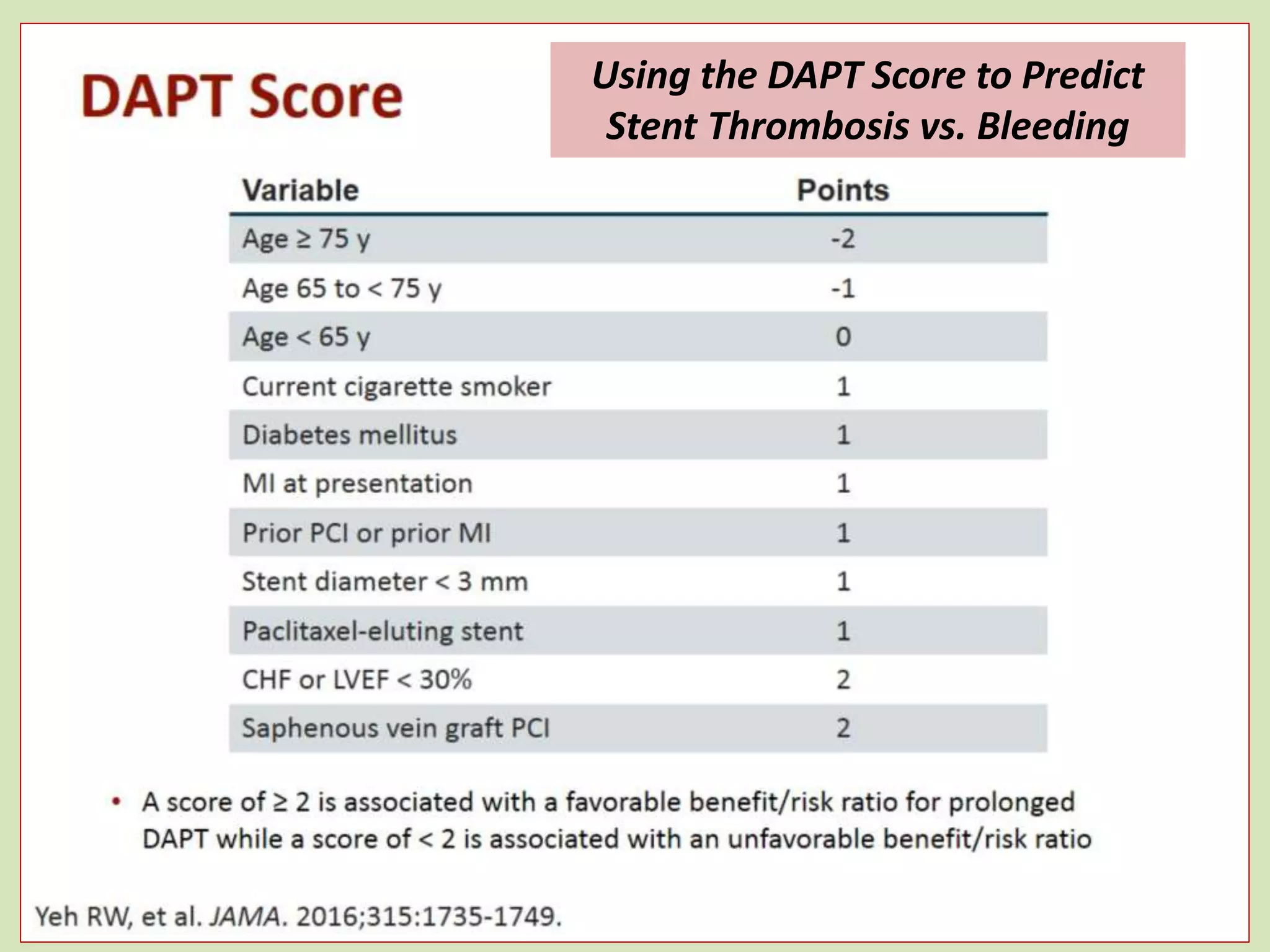
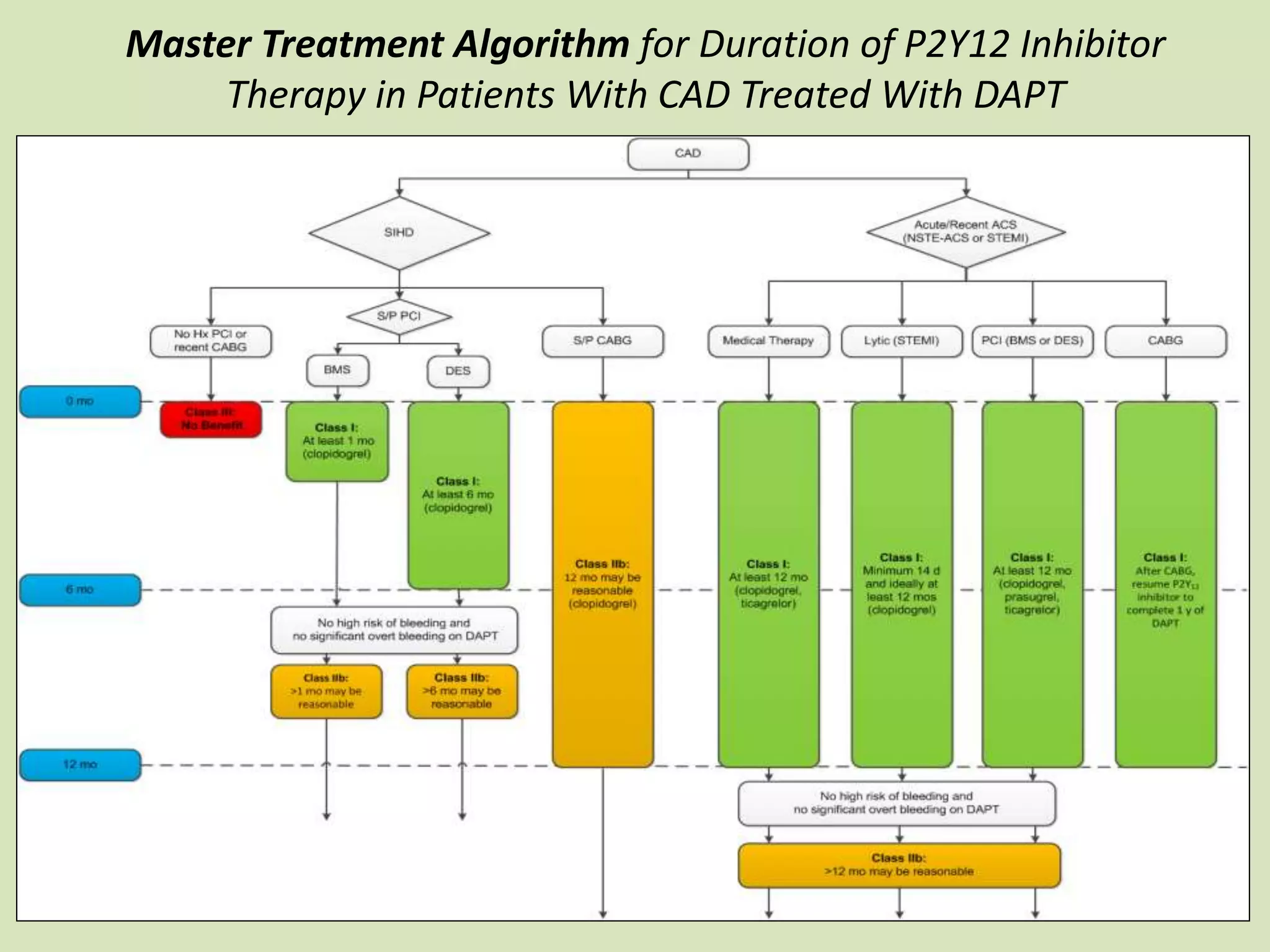
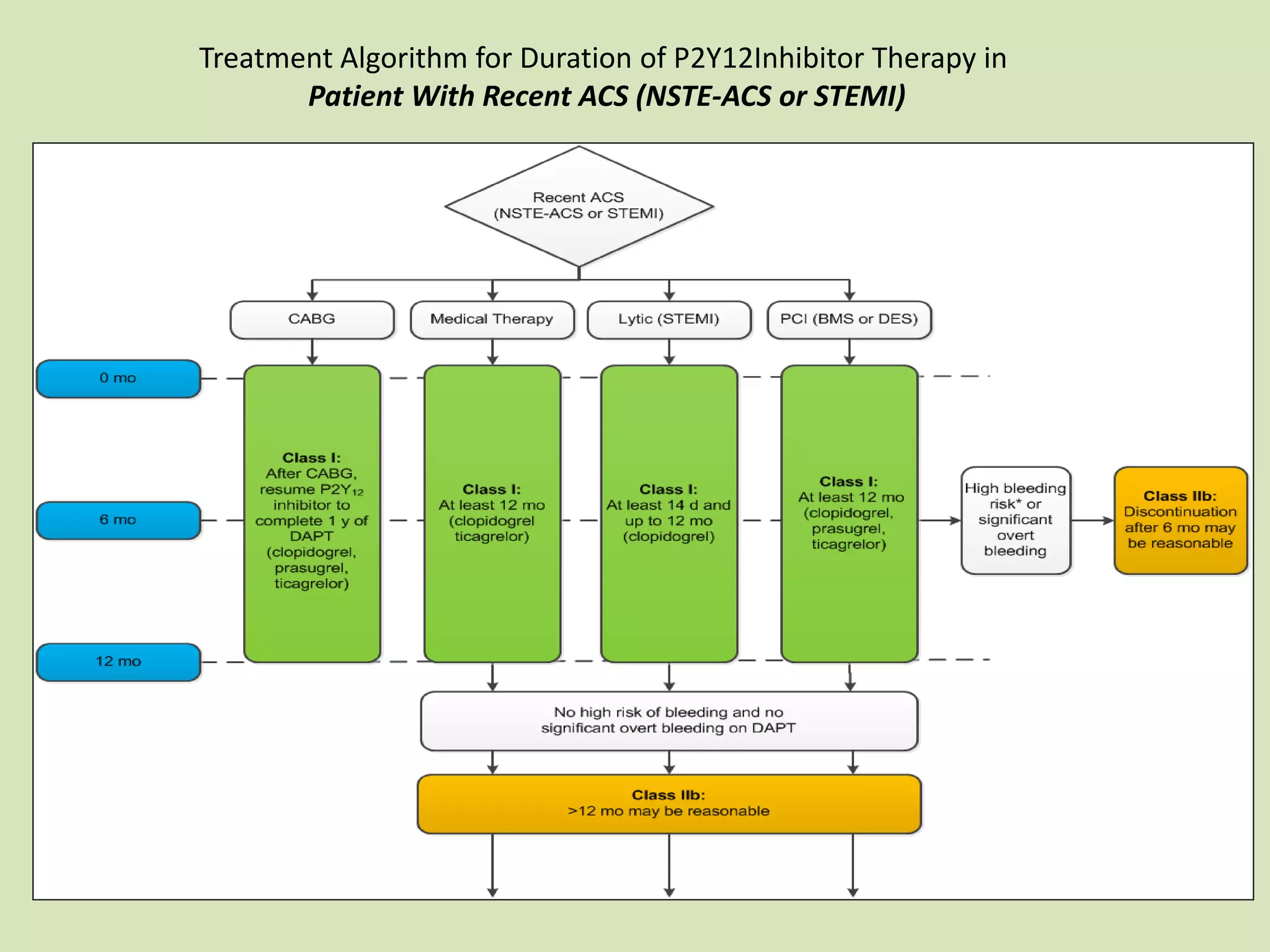
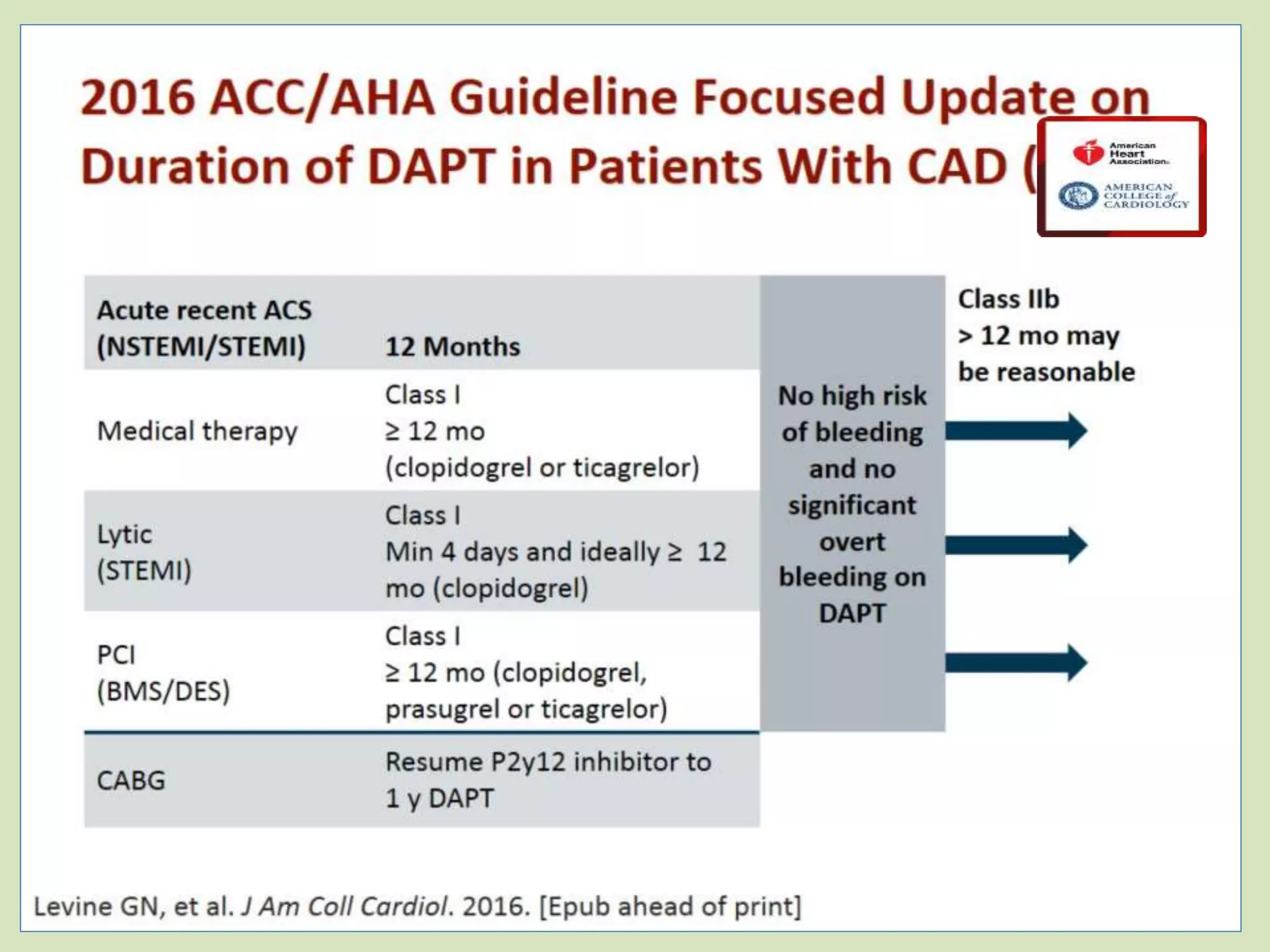
This document discusses antiplatelet therapy for acute coronary syndromes. It provides information on dual antiplatelet therapy using aspirin and P2Y12 inhibitors like clopidogrel, prasugrel, and ticagrelor. It summarizes trials comparing these drugs and outlines treatment strategies and duration of dual antiplatelet therapy based on a patient's risk level. Factors influencing response to clopidogrel and the potential additional mechanisms of action of ticagrelor are also reviewed.