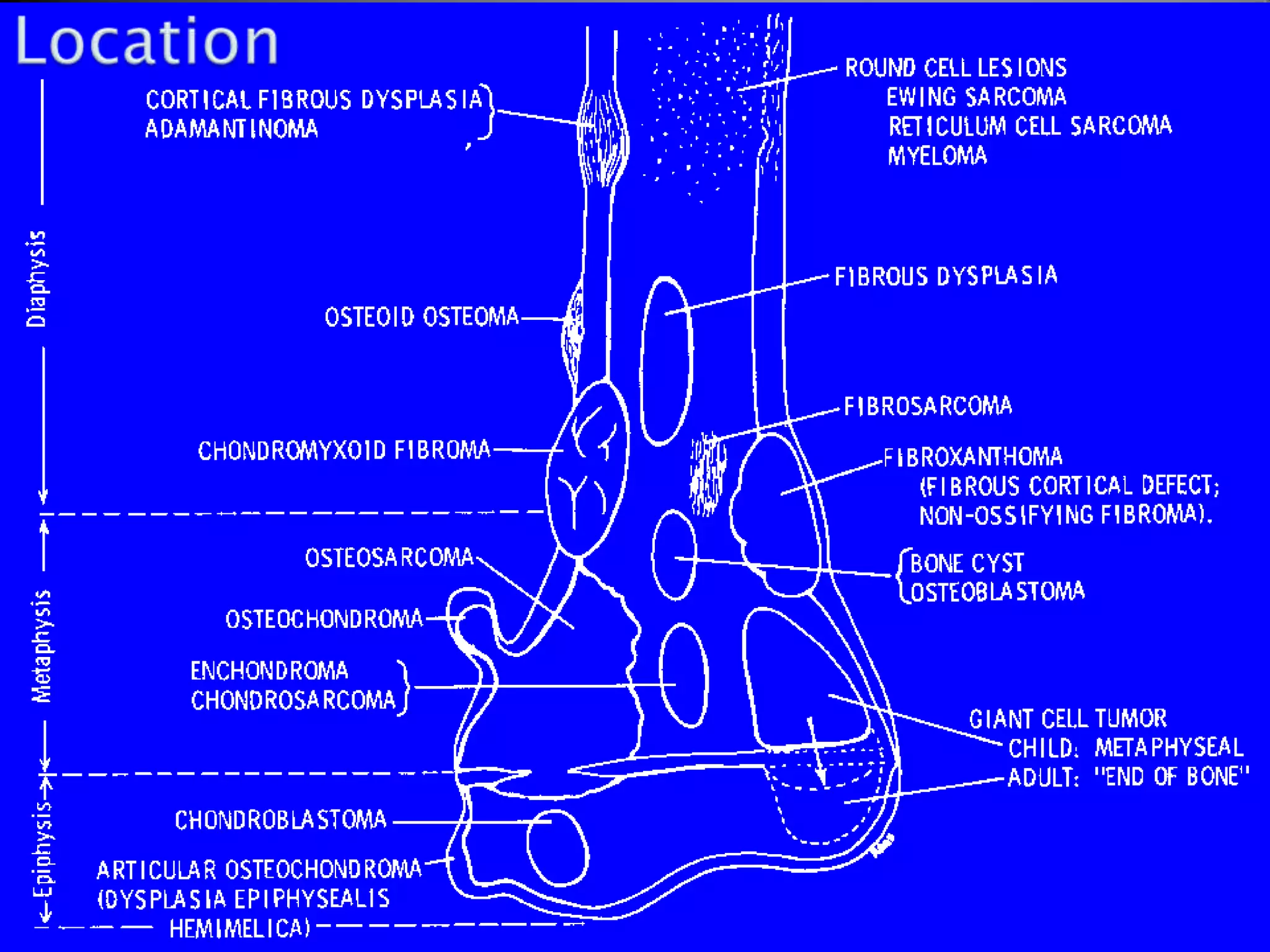
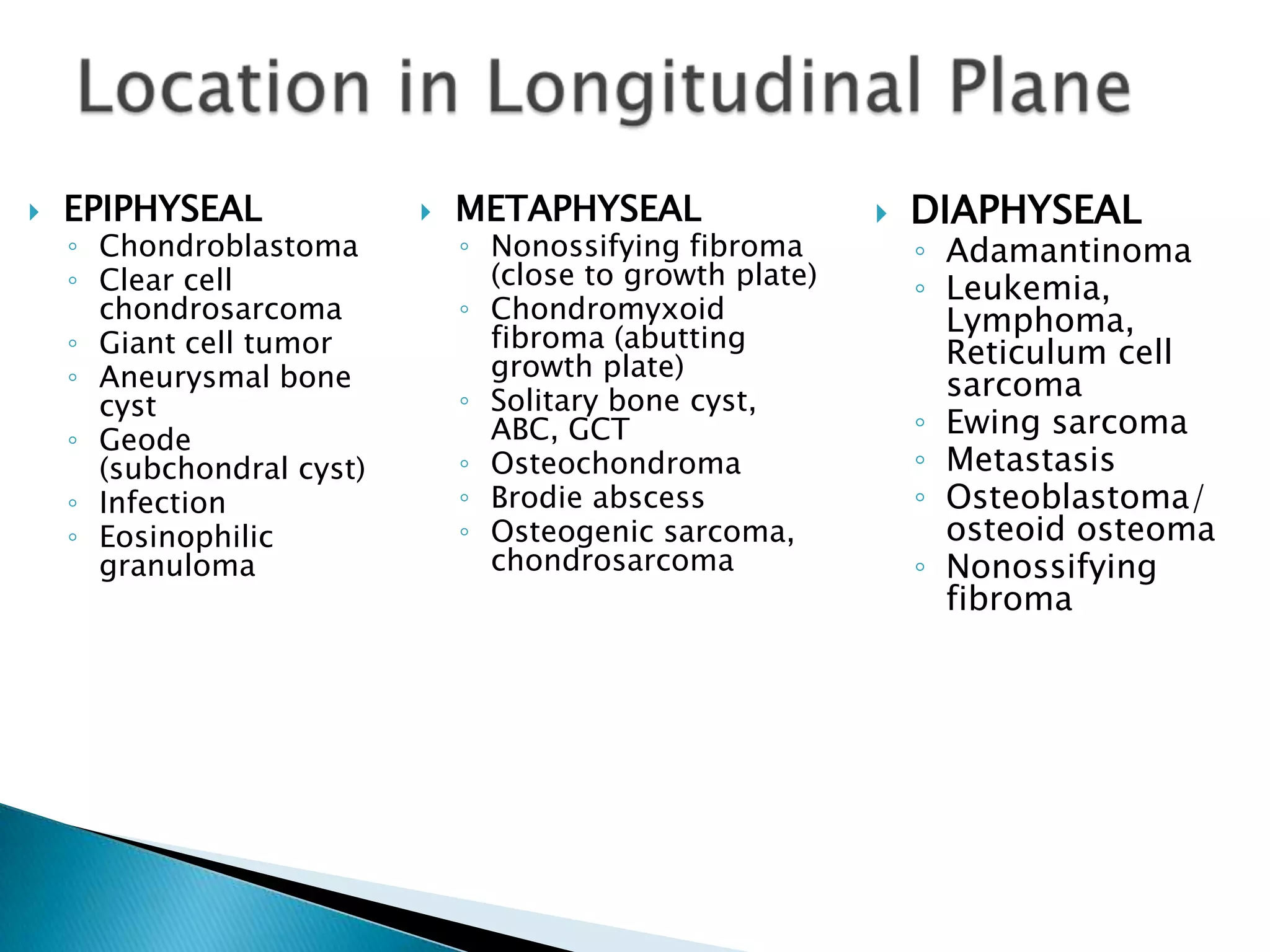
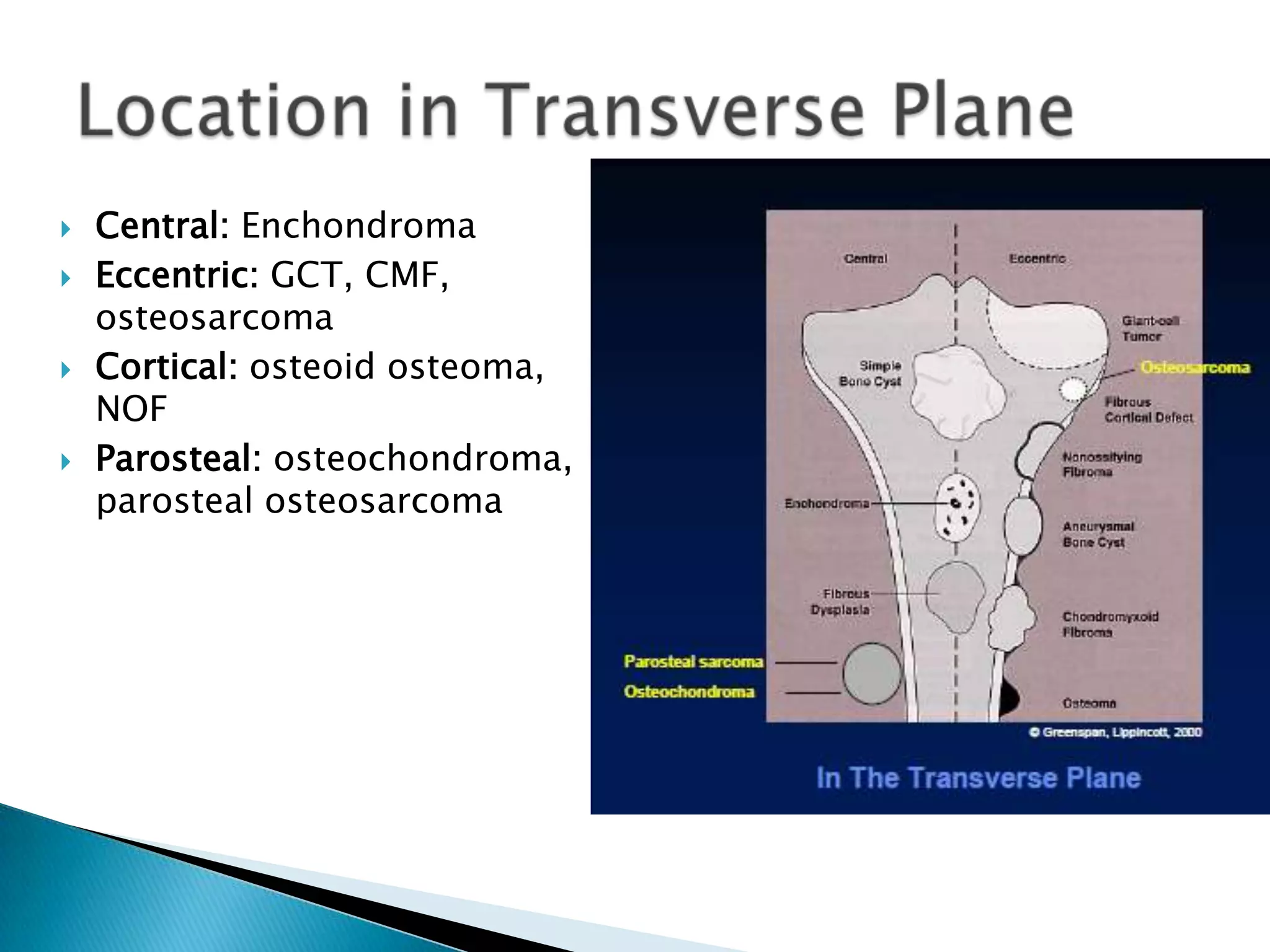
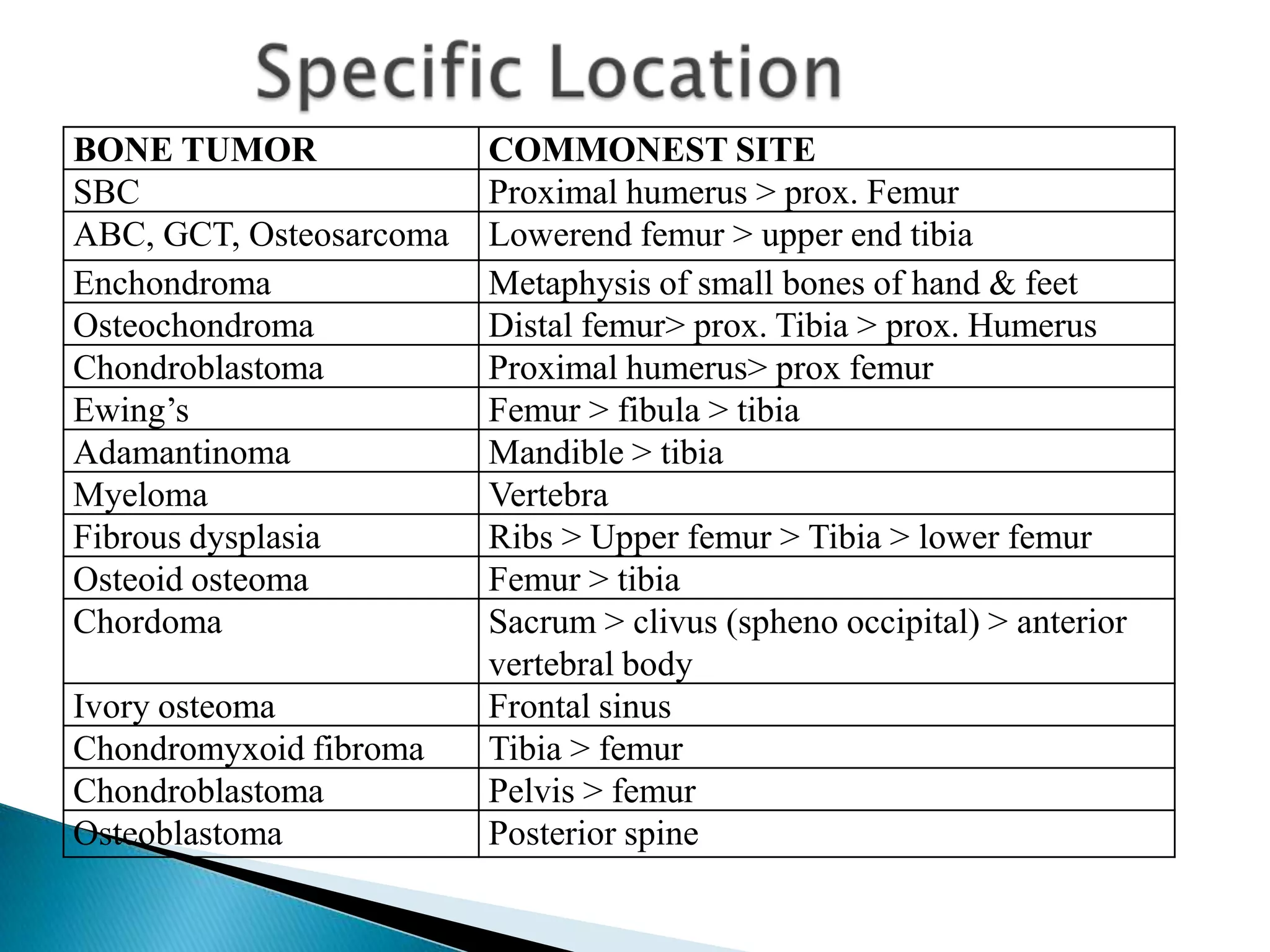
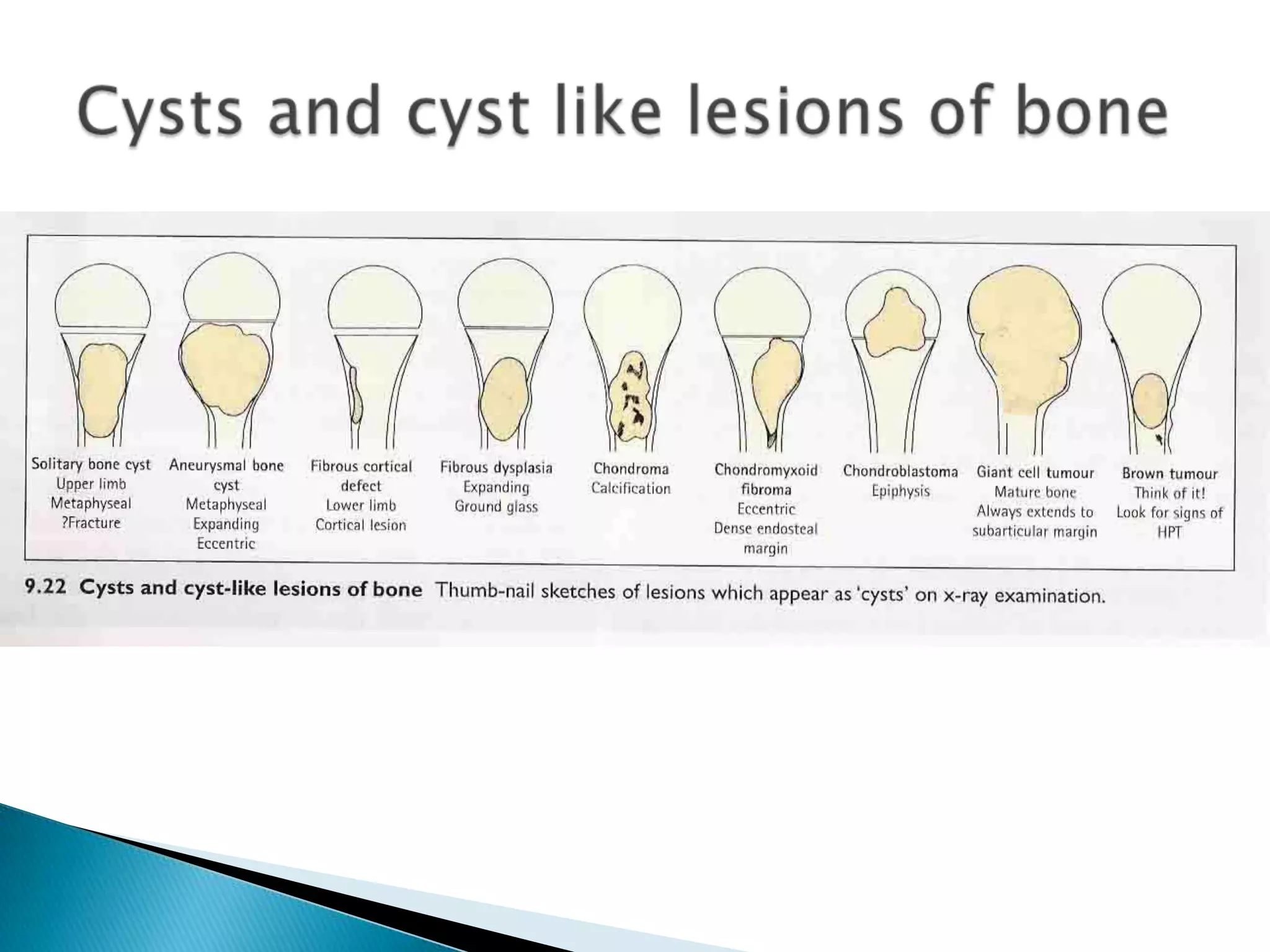
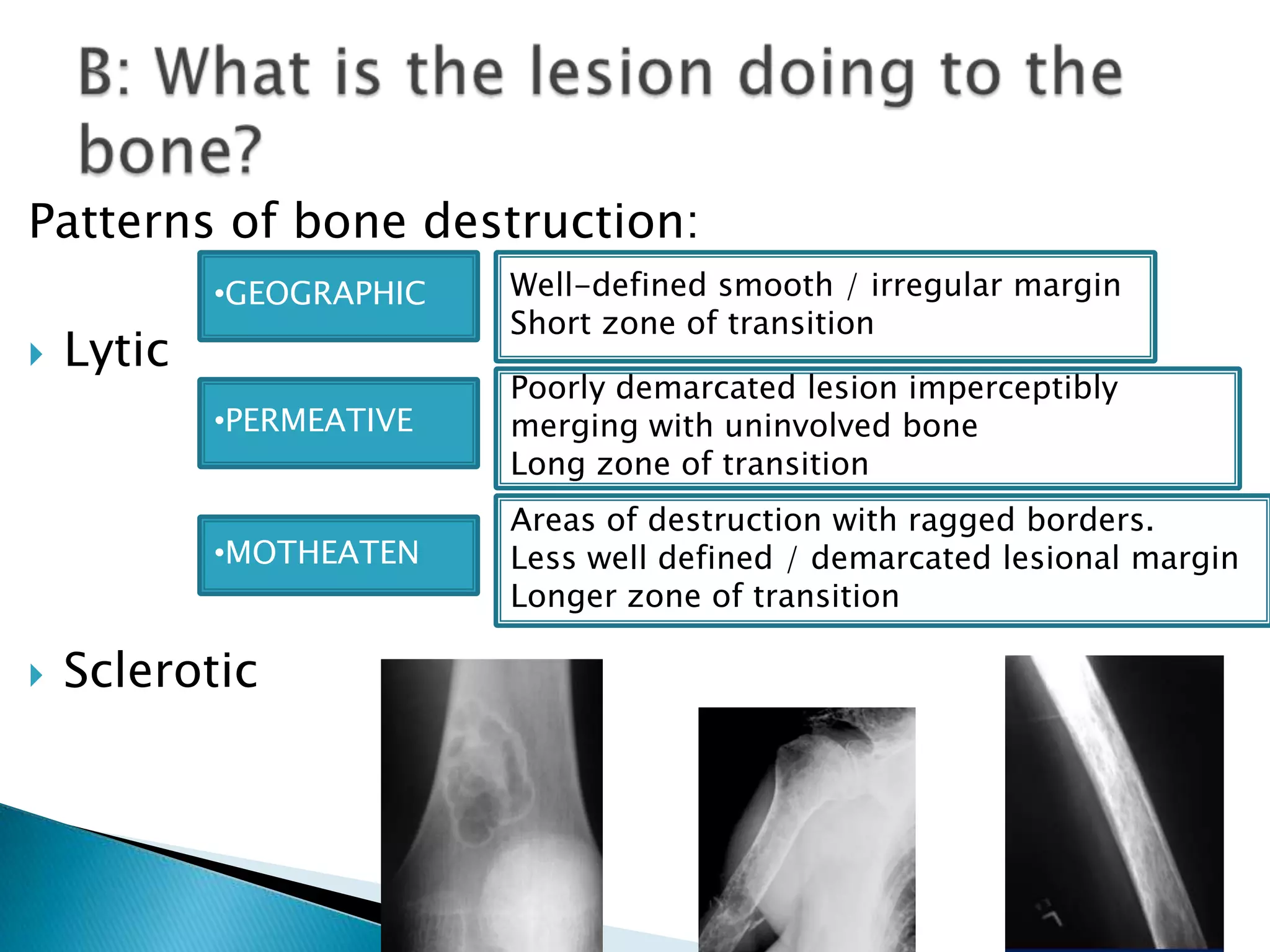
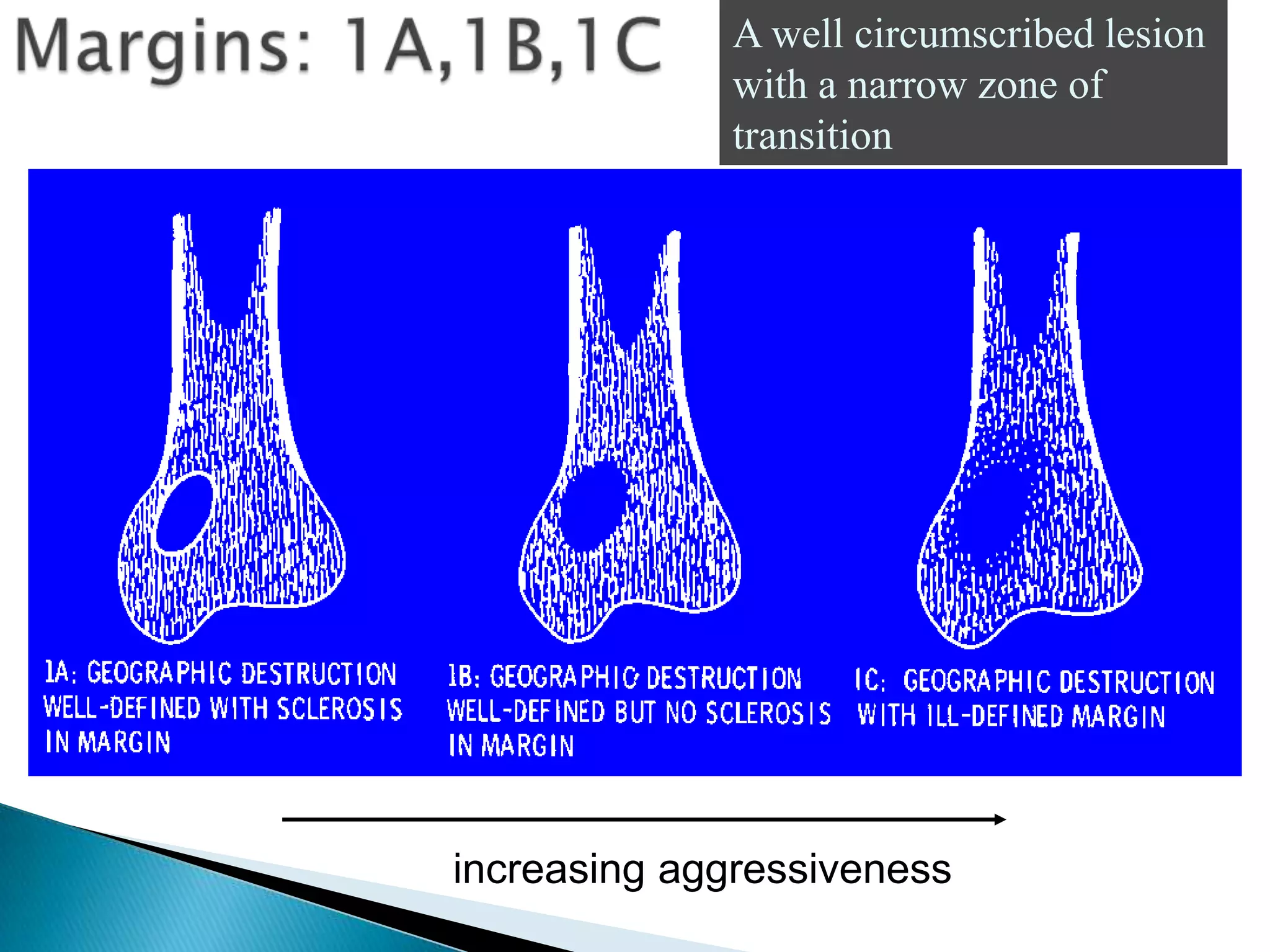
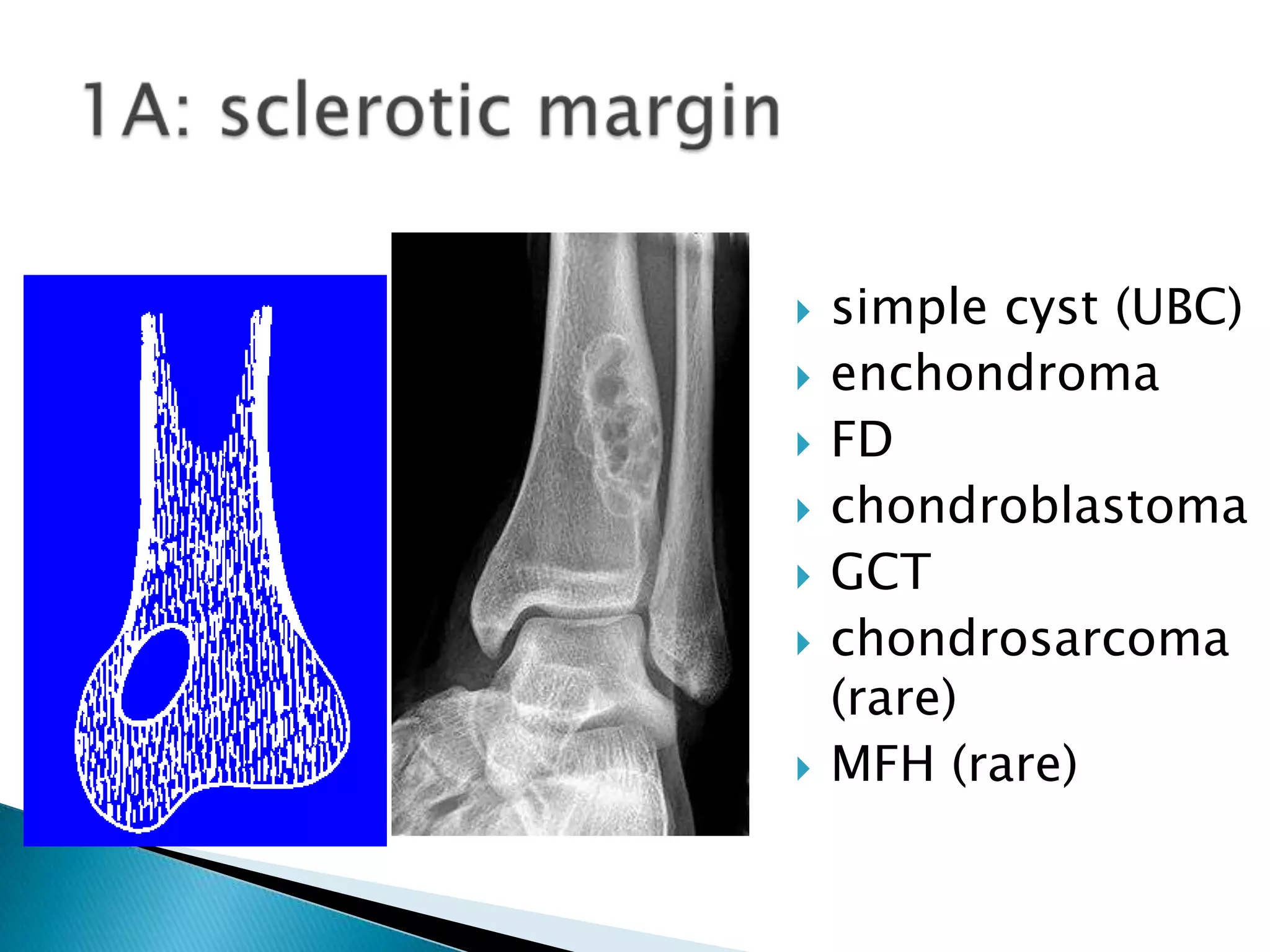
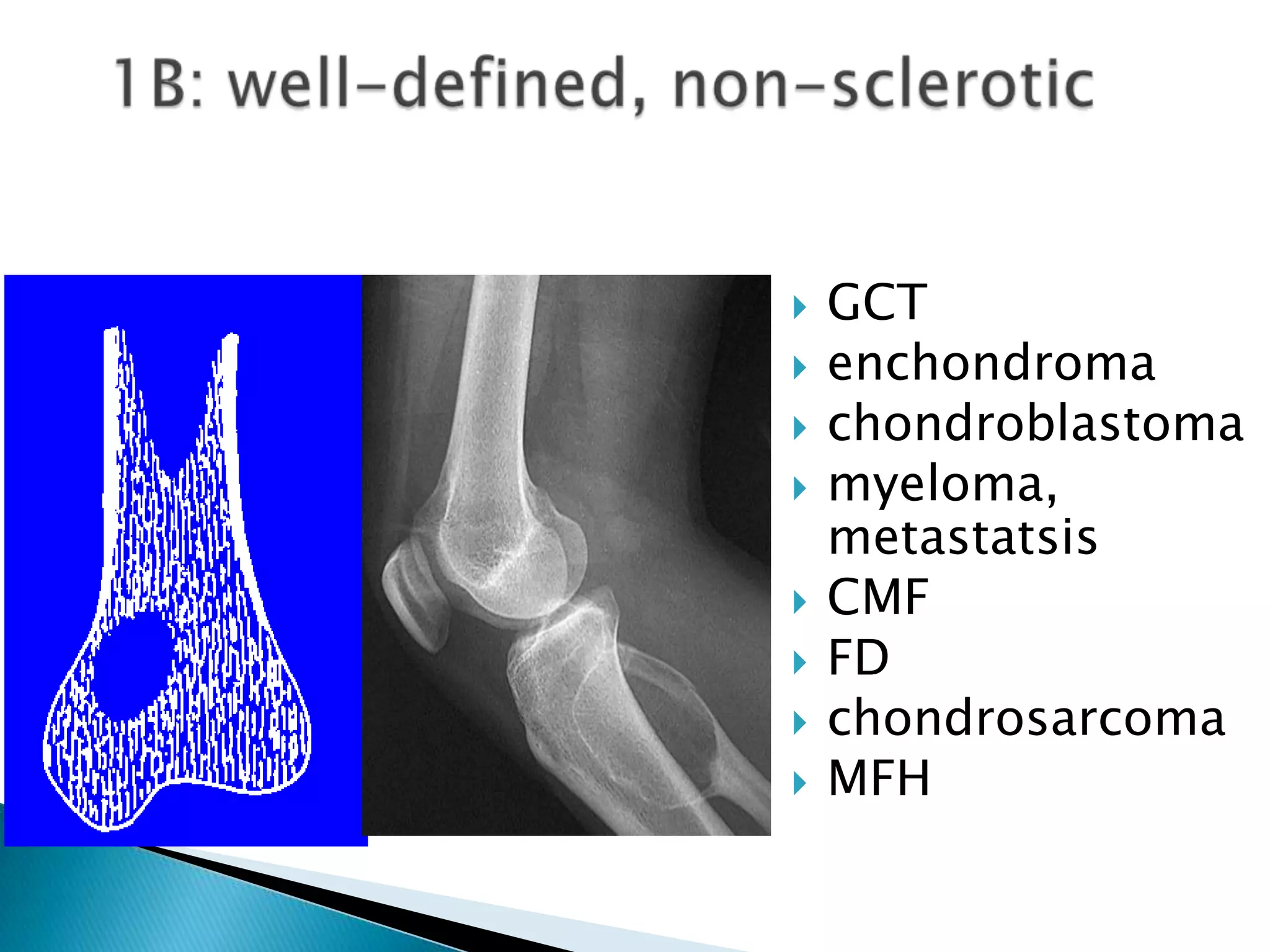
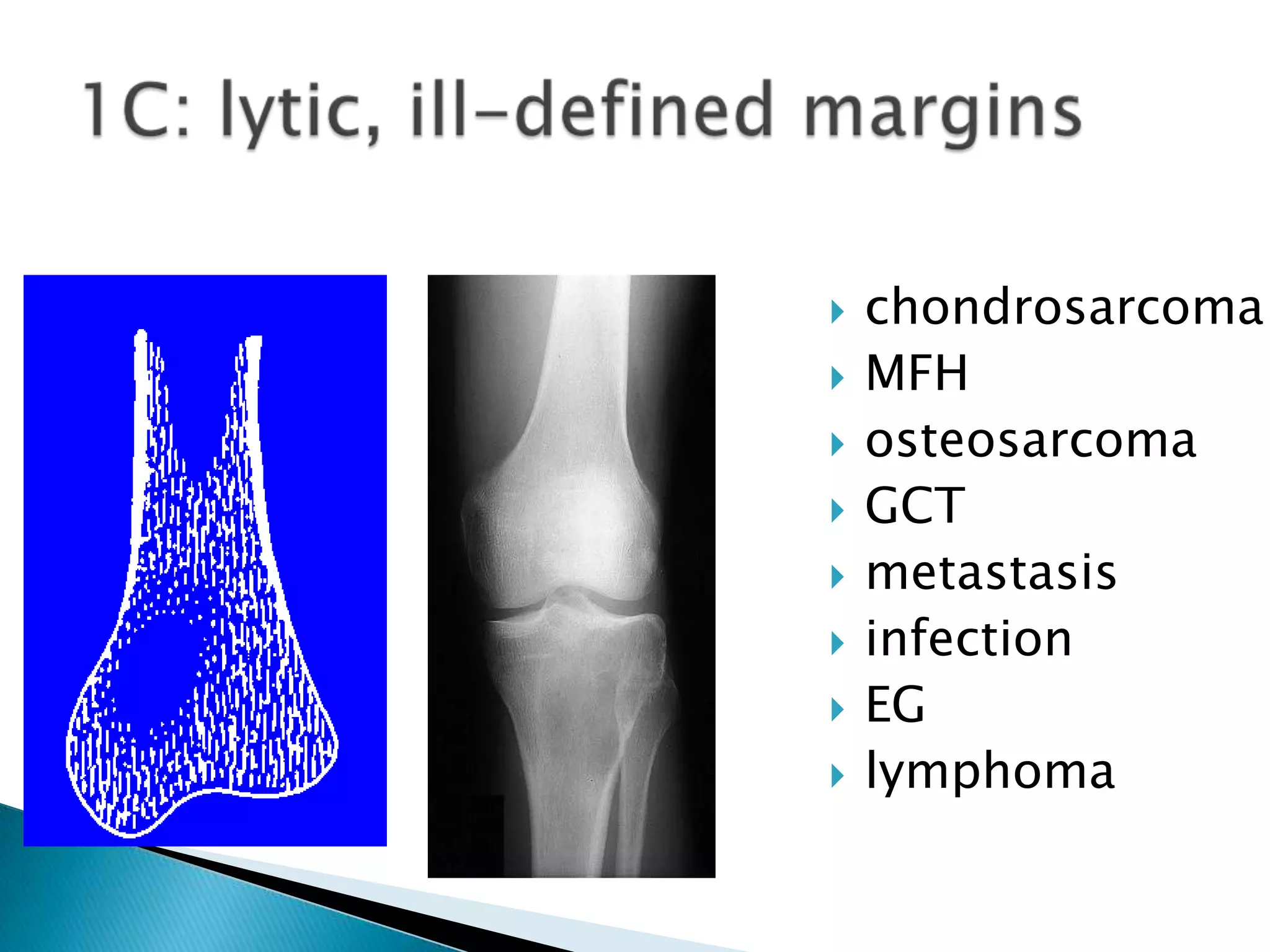
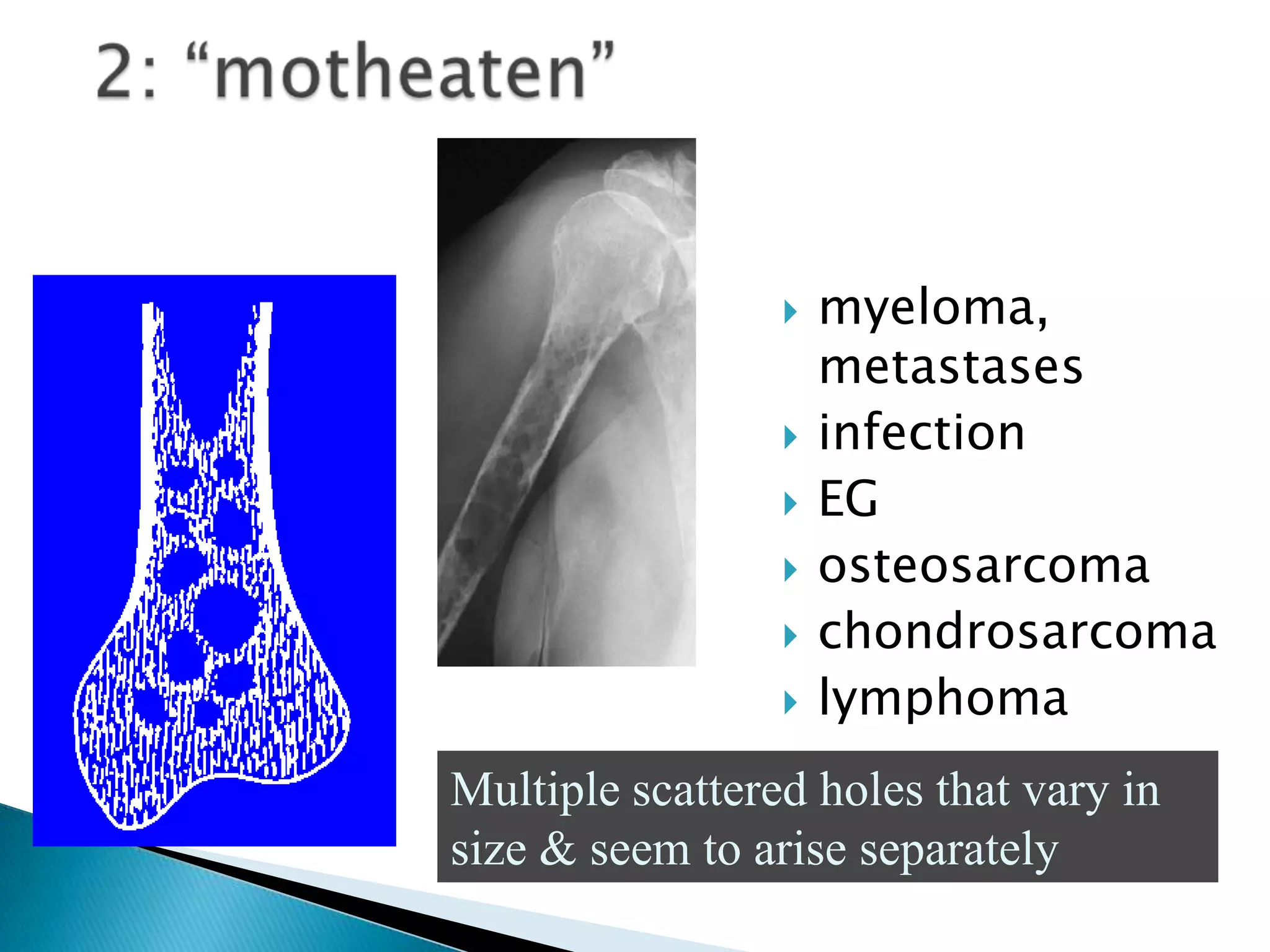
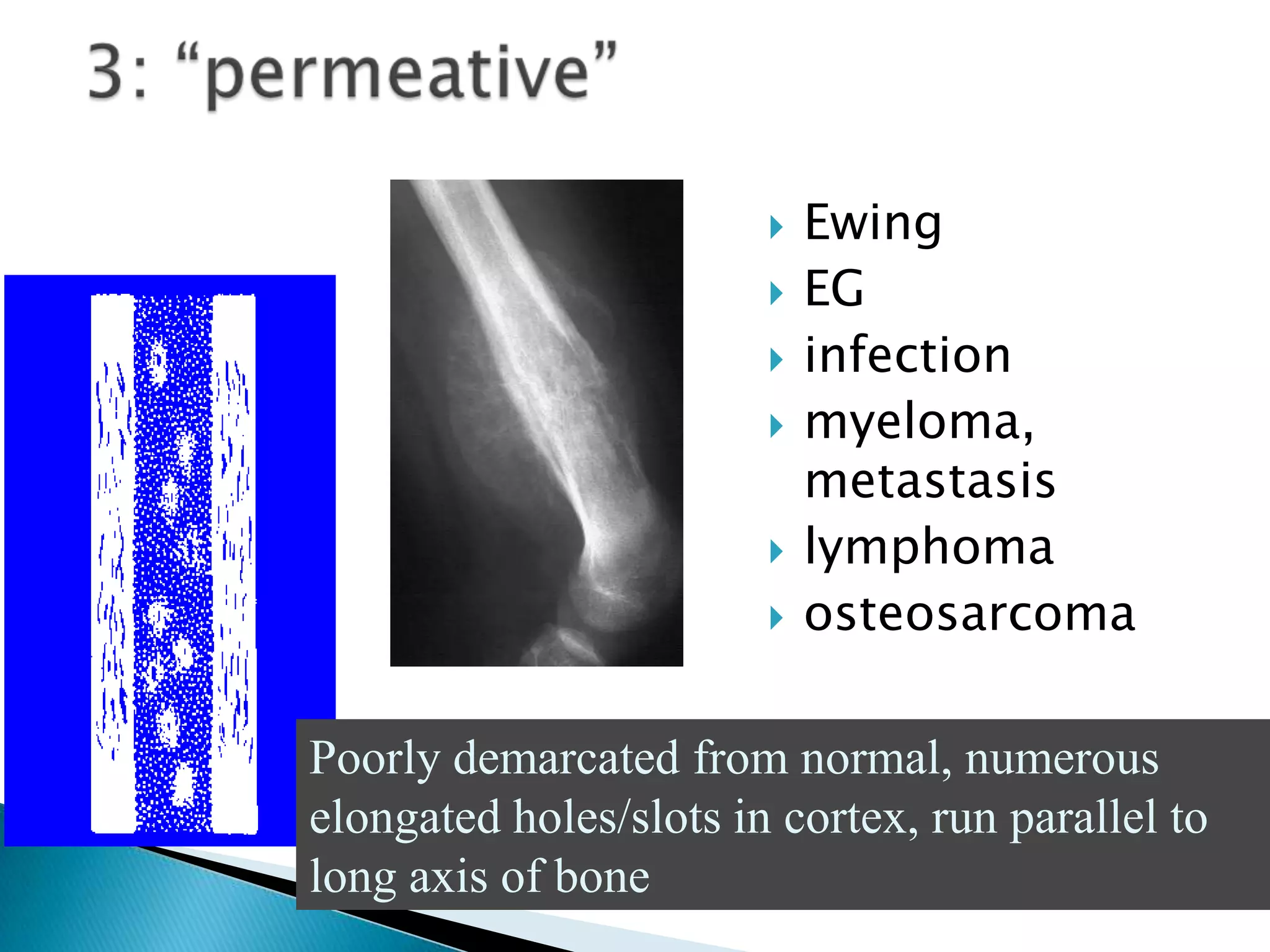
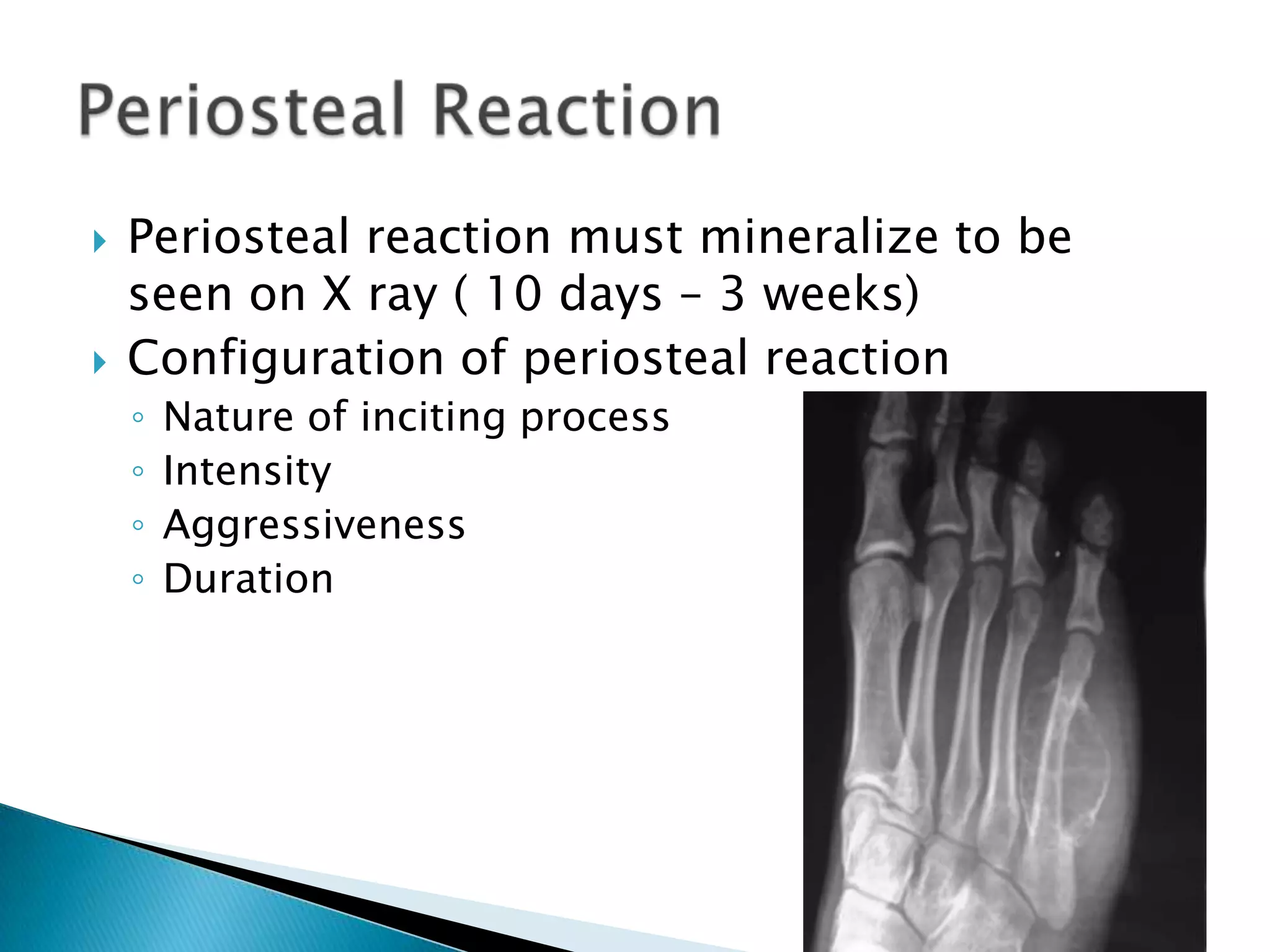
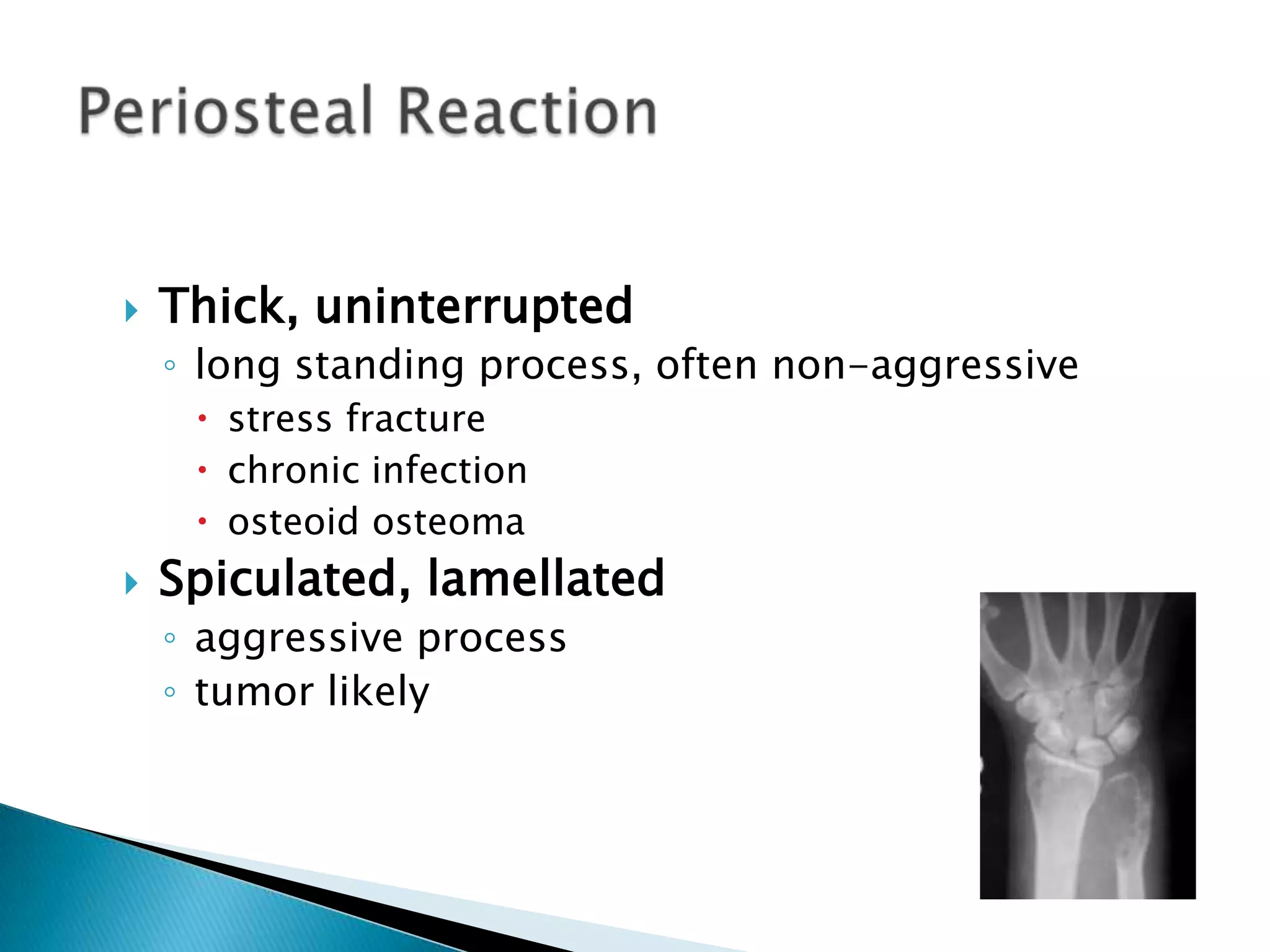
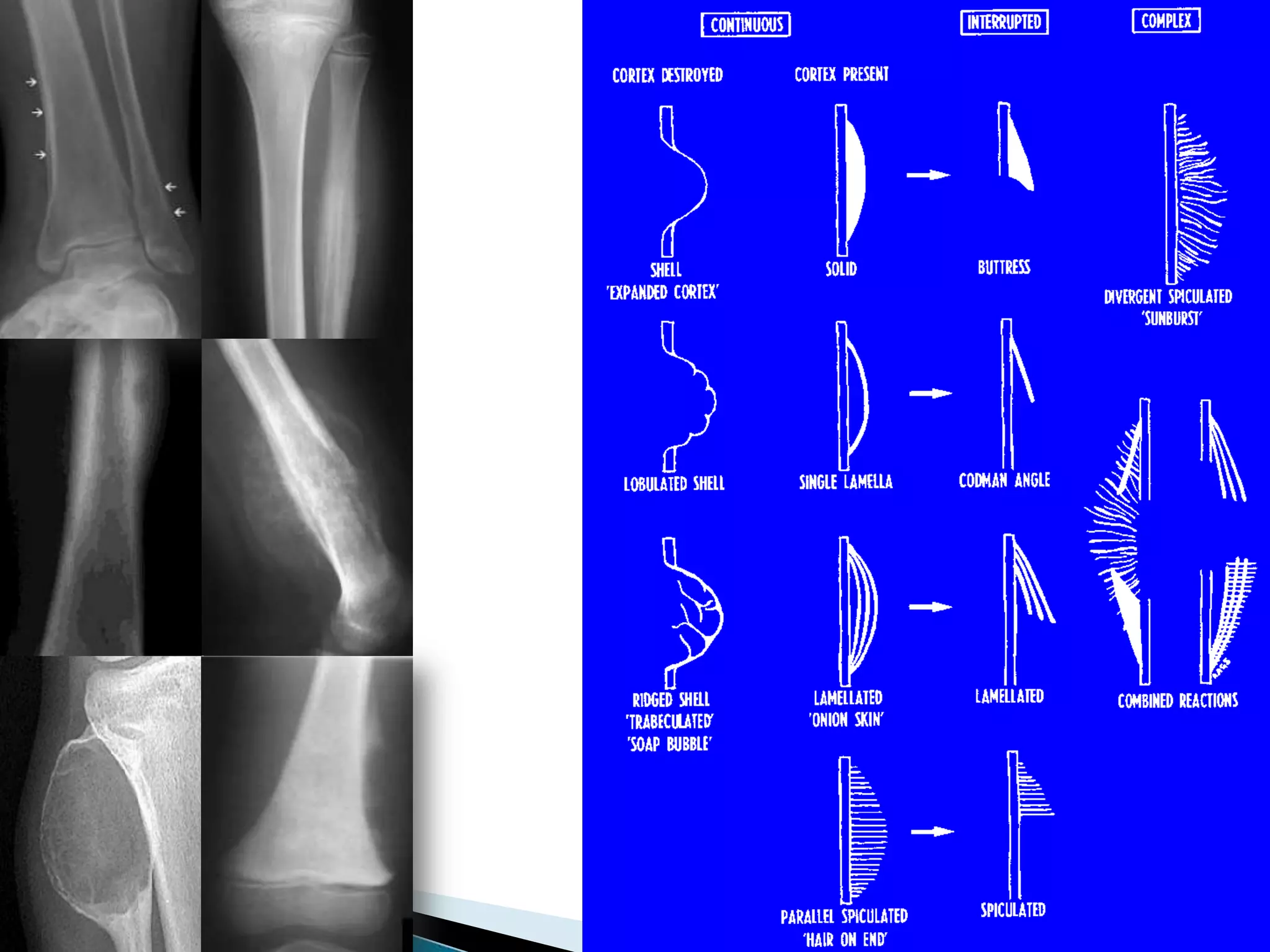
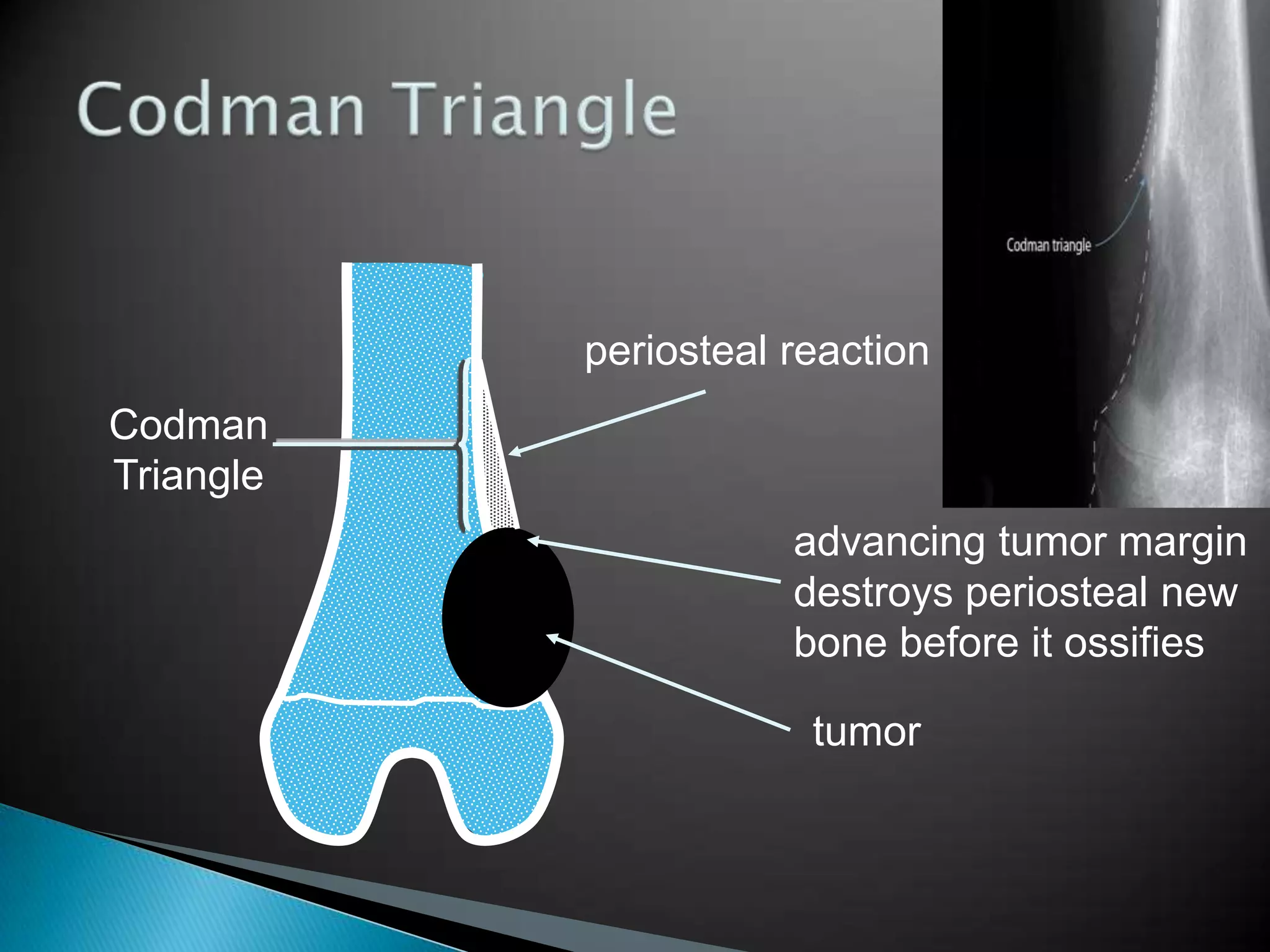
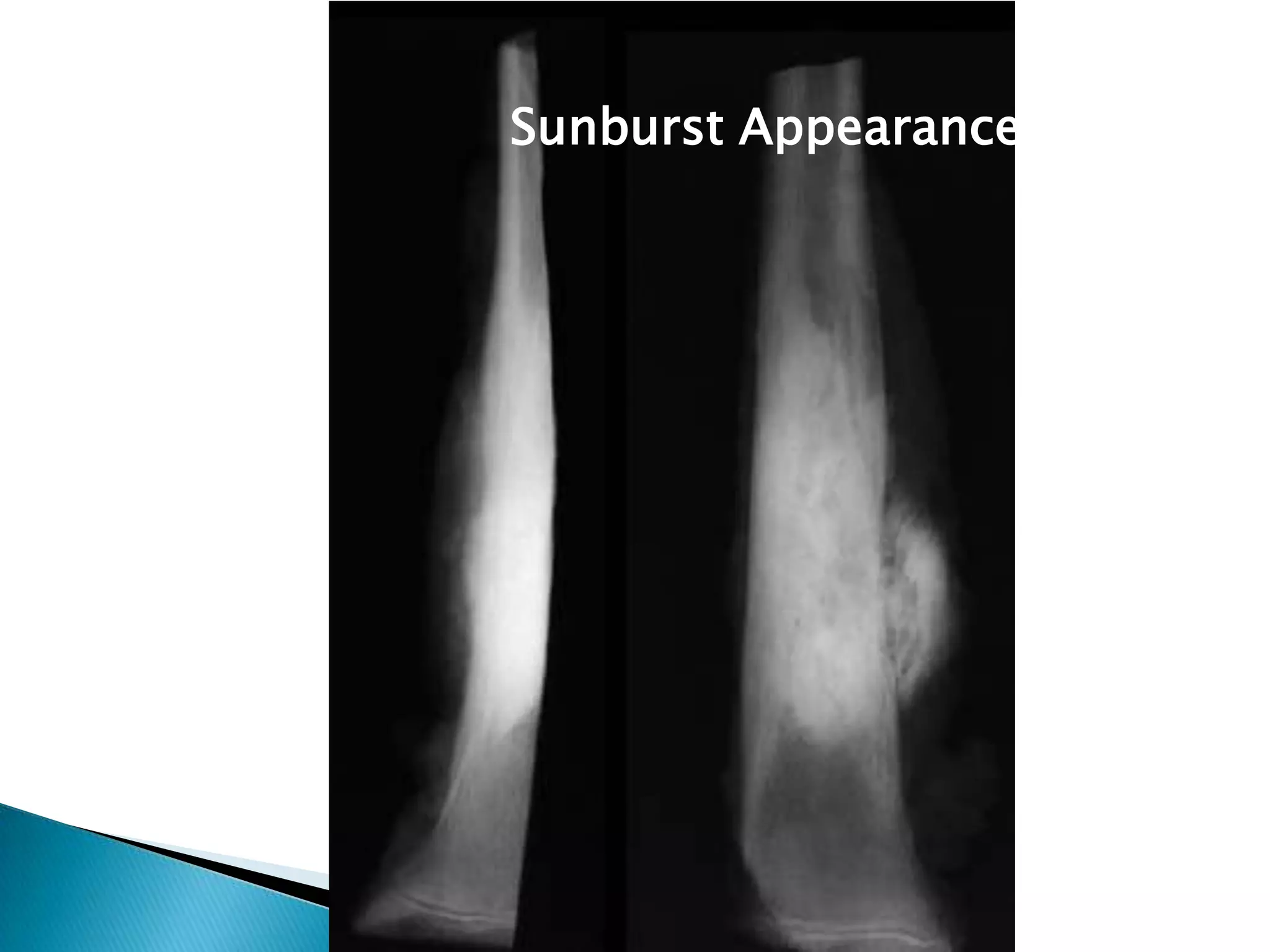
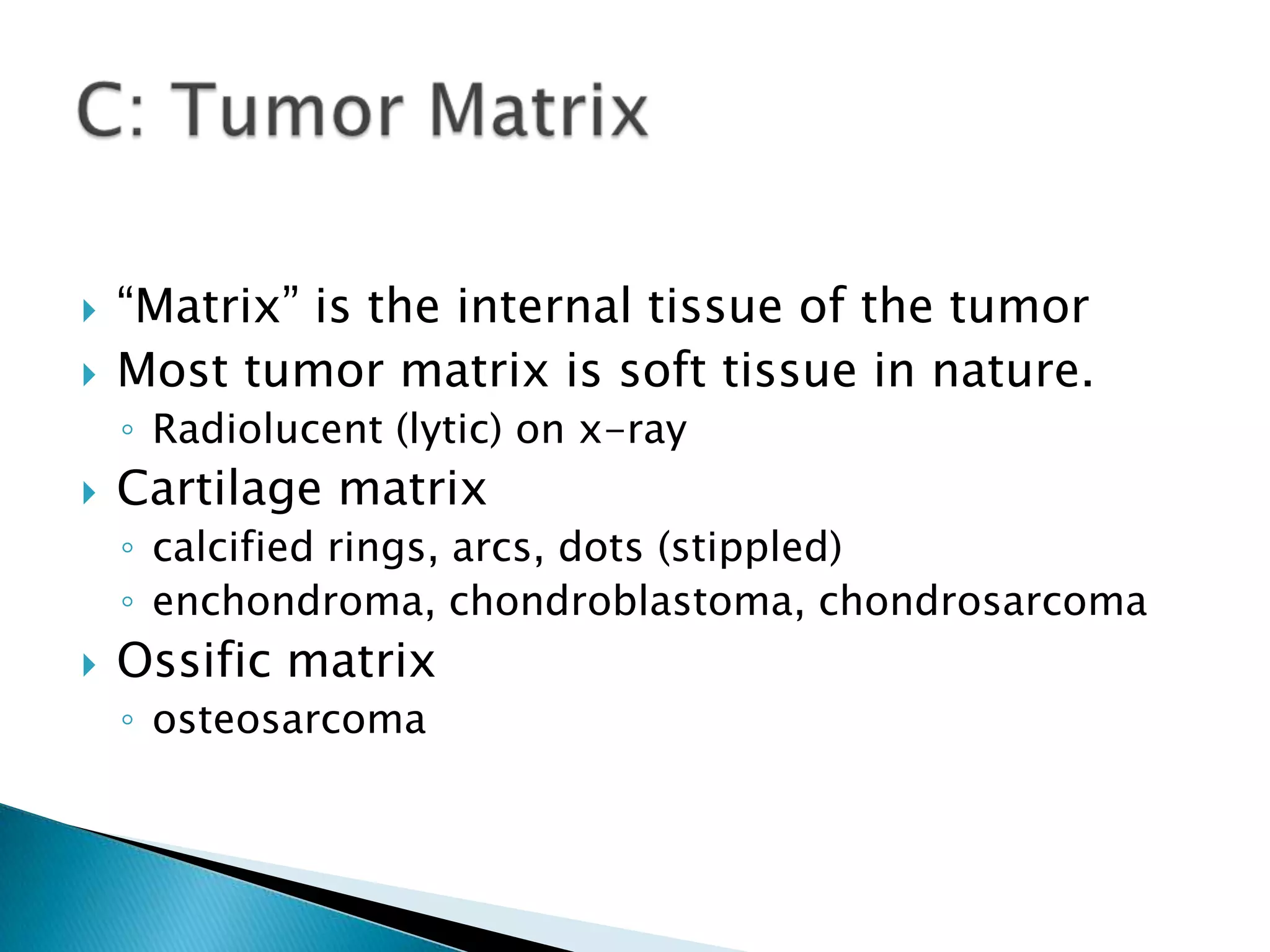
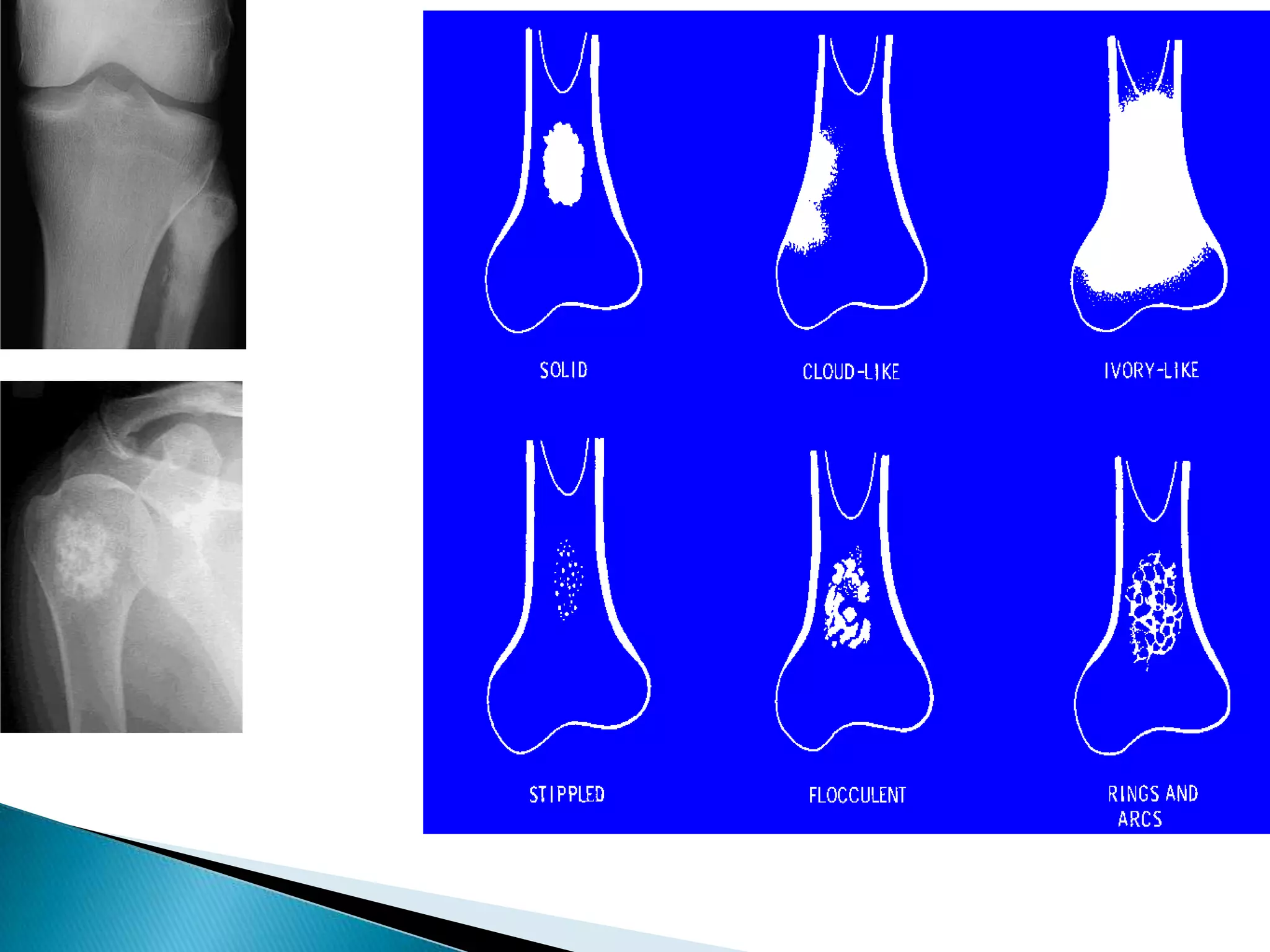
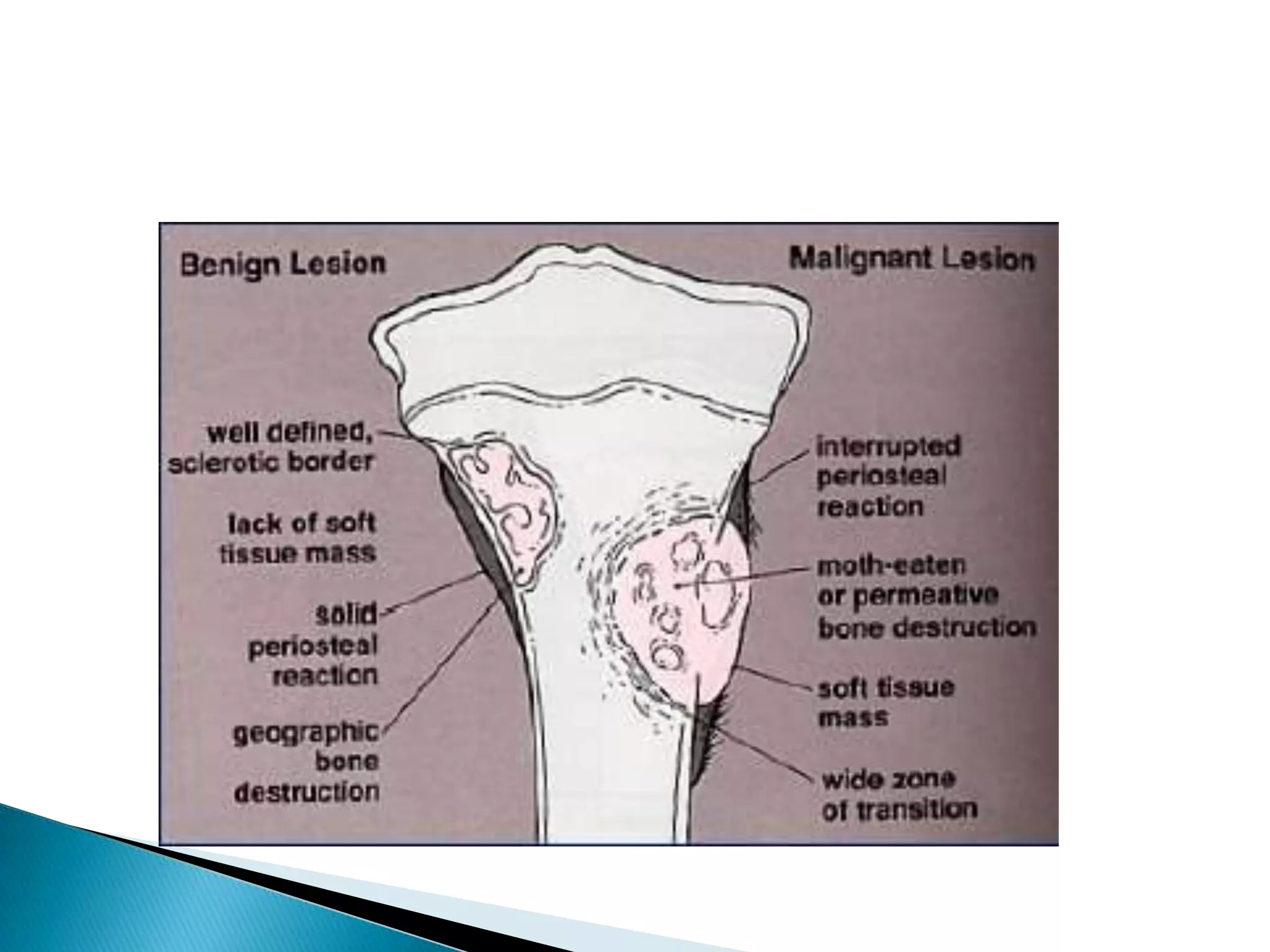
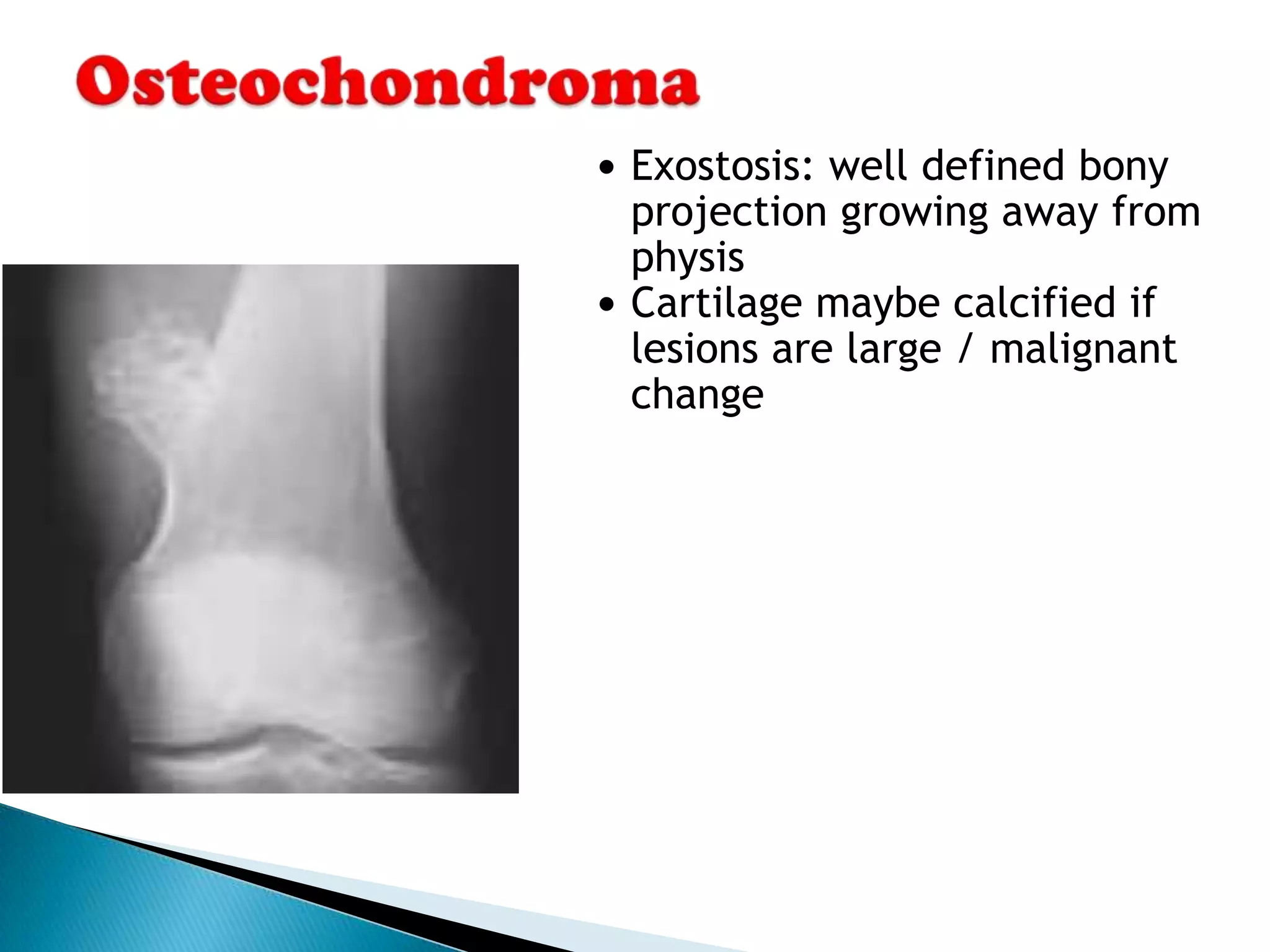
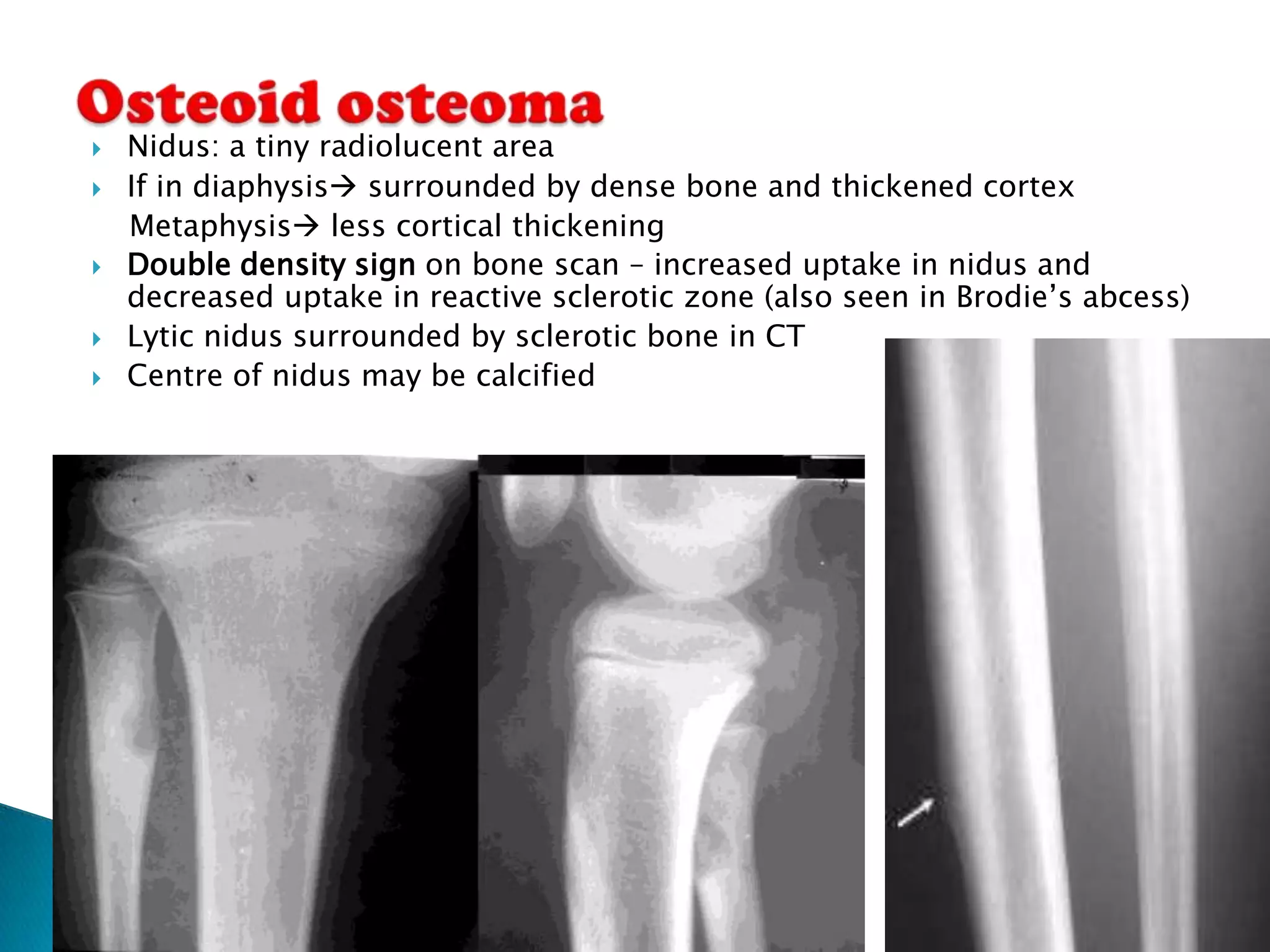
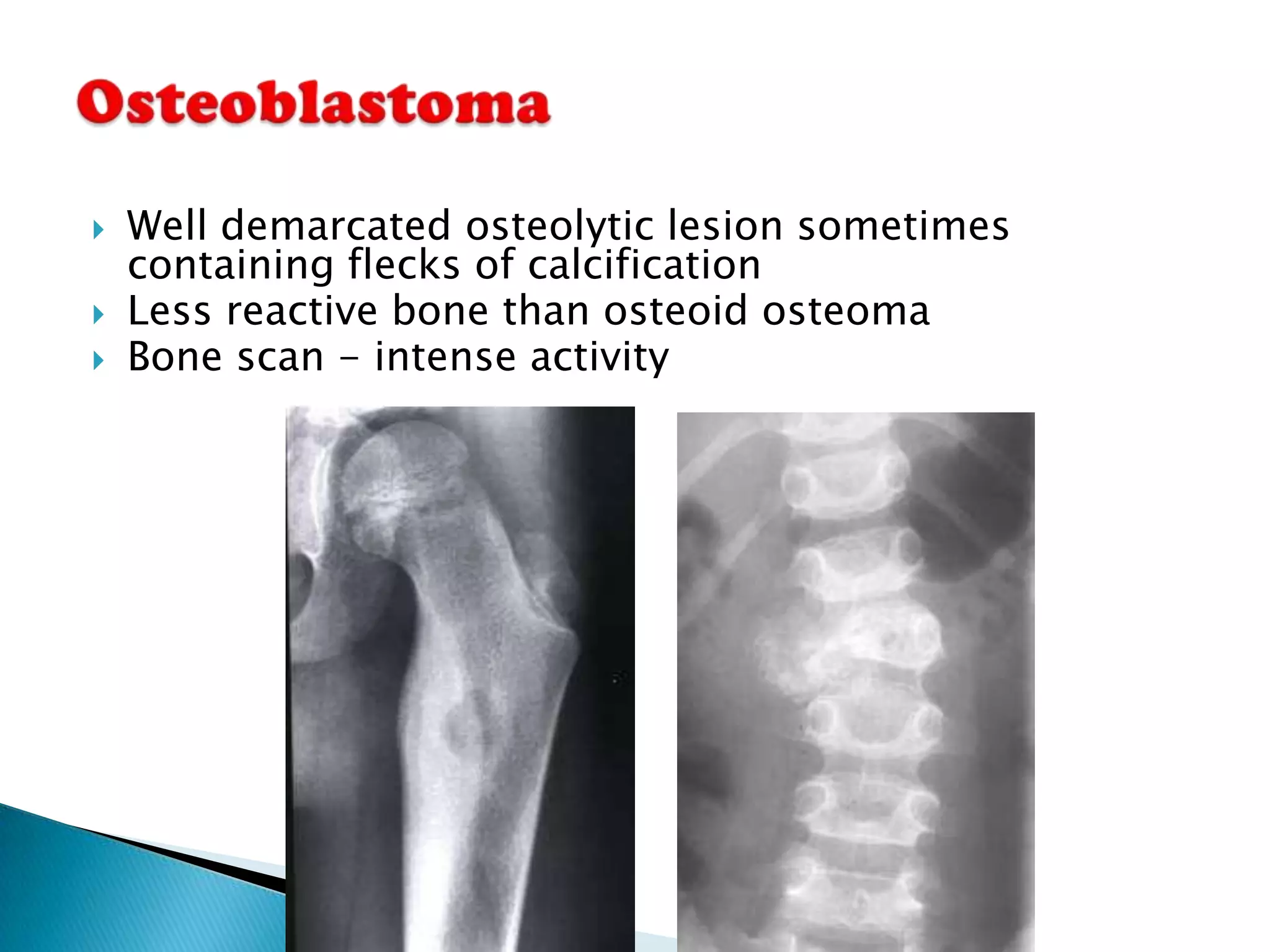
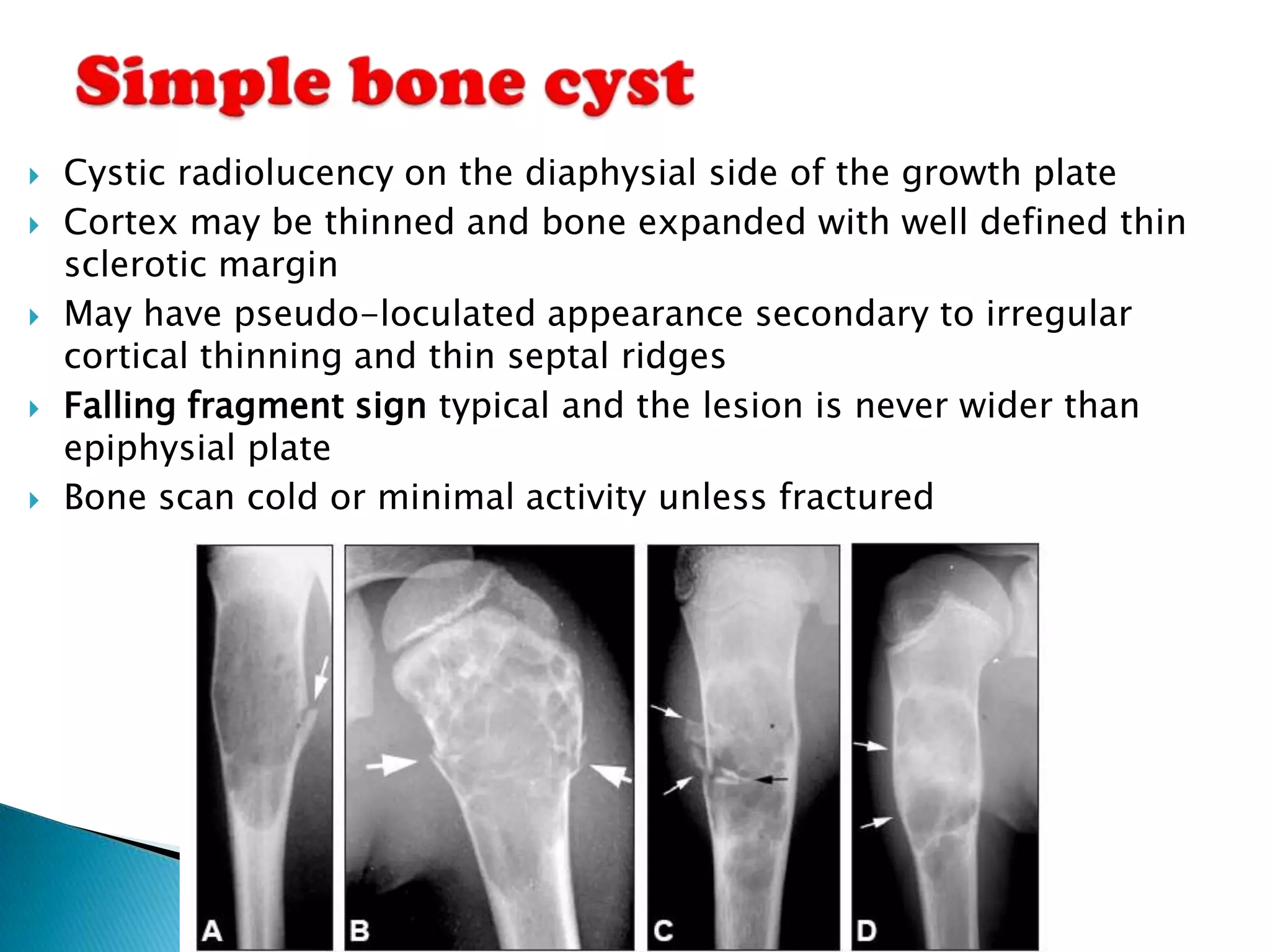
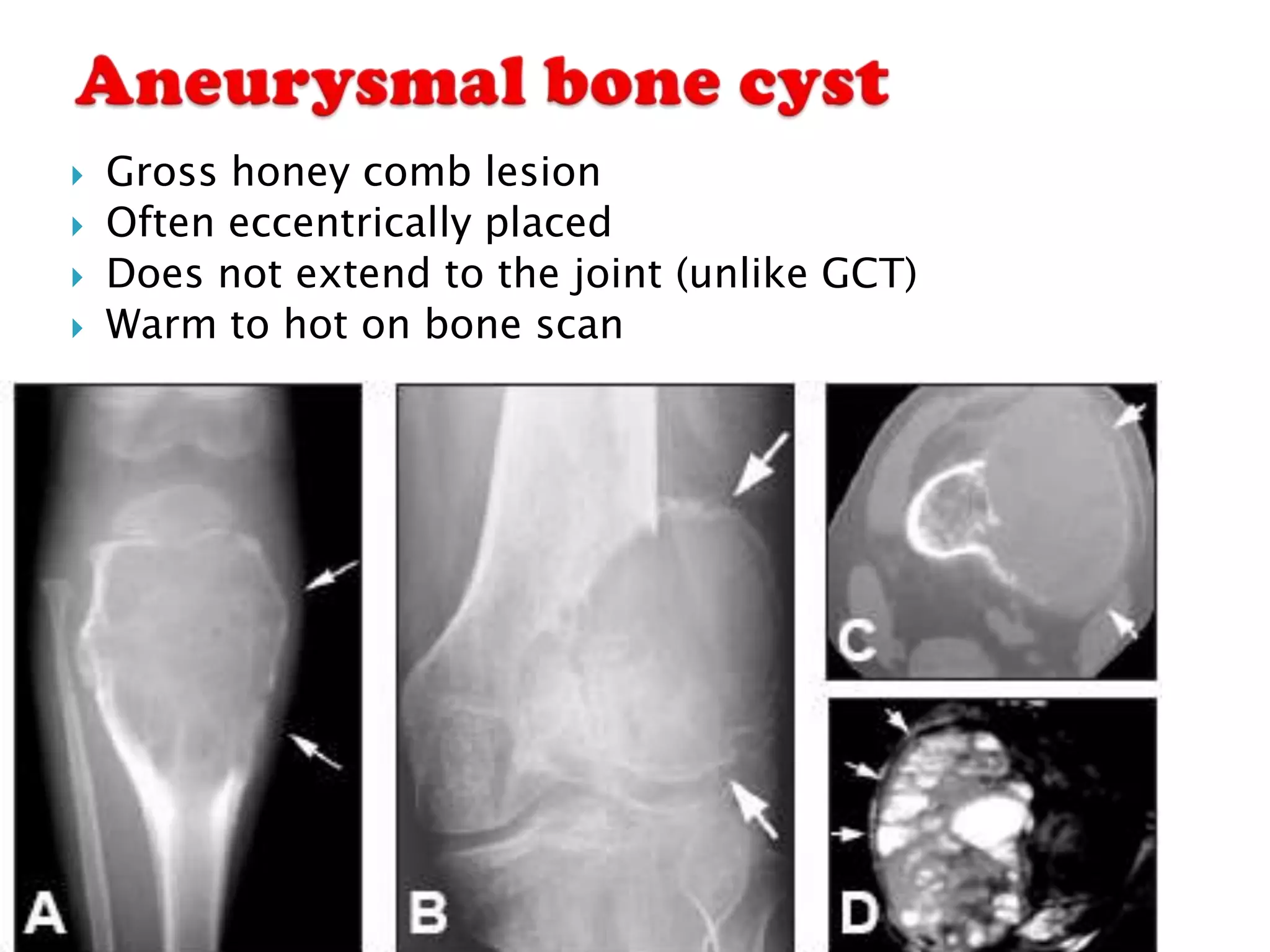
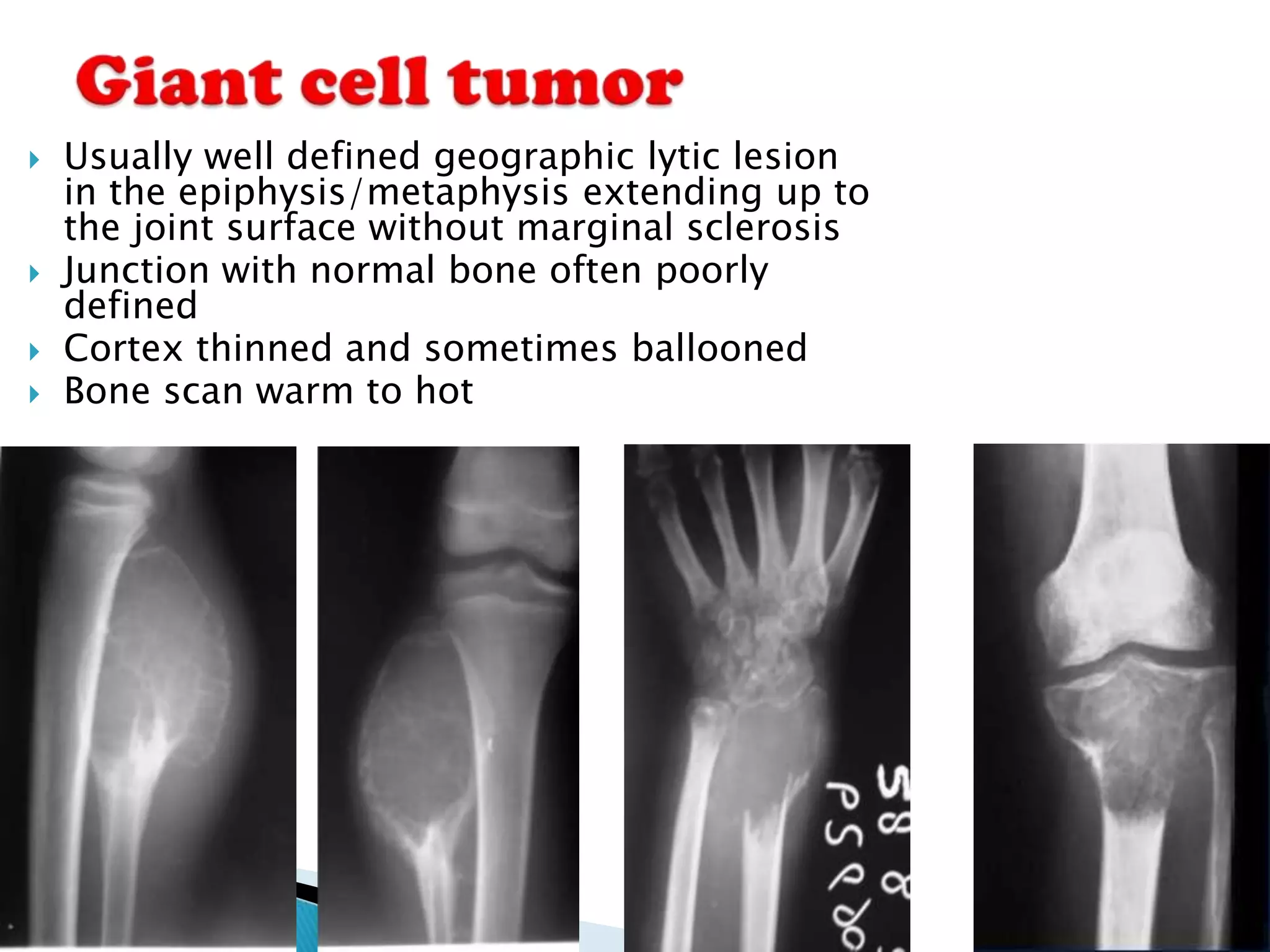
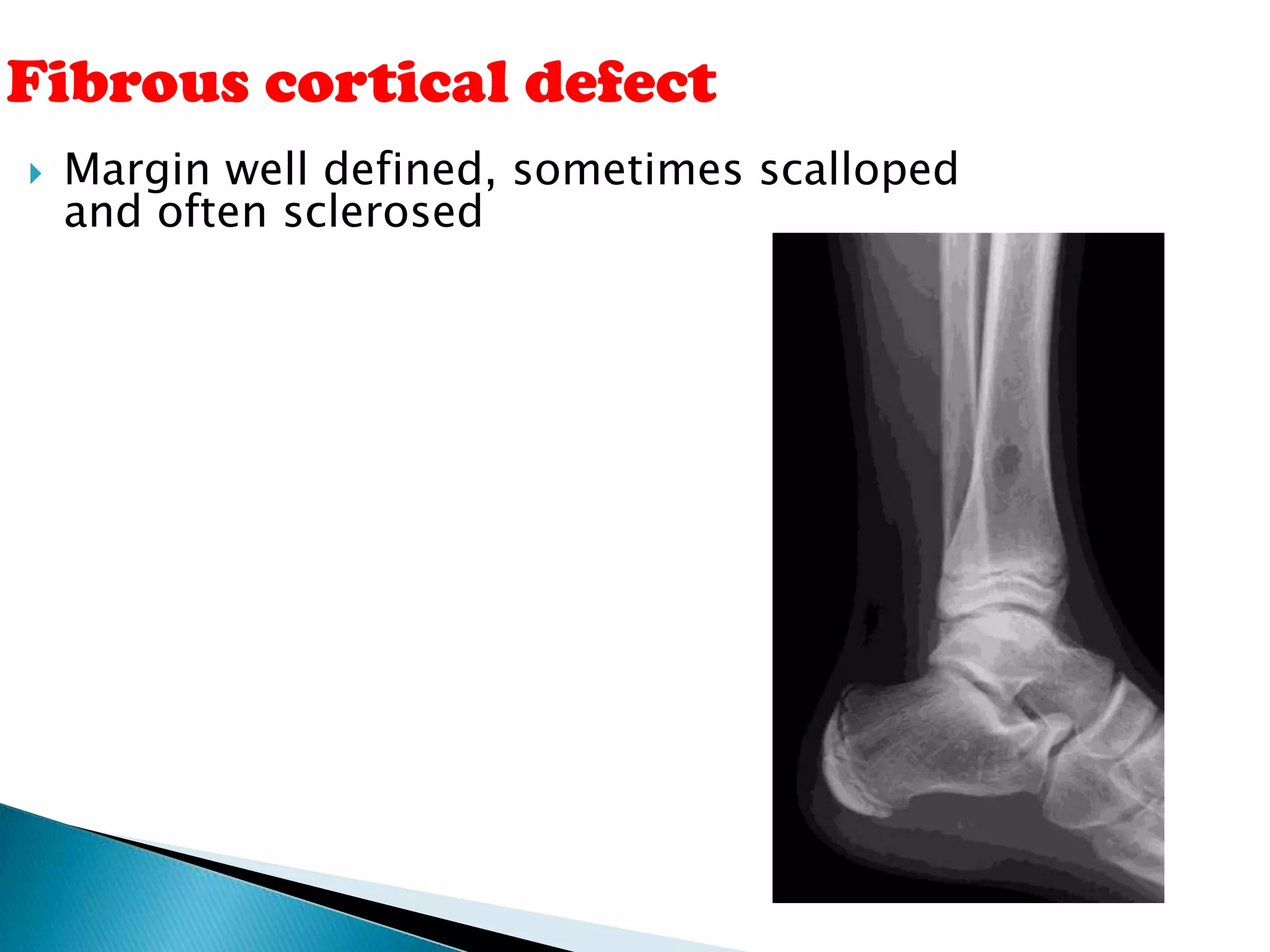
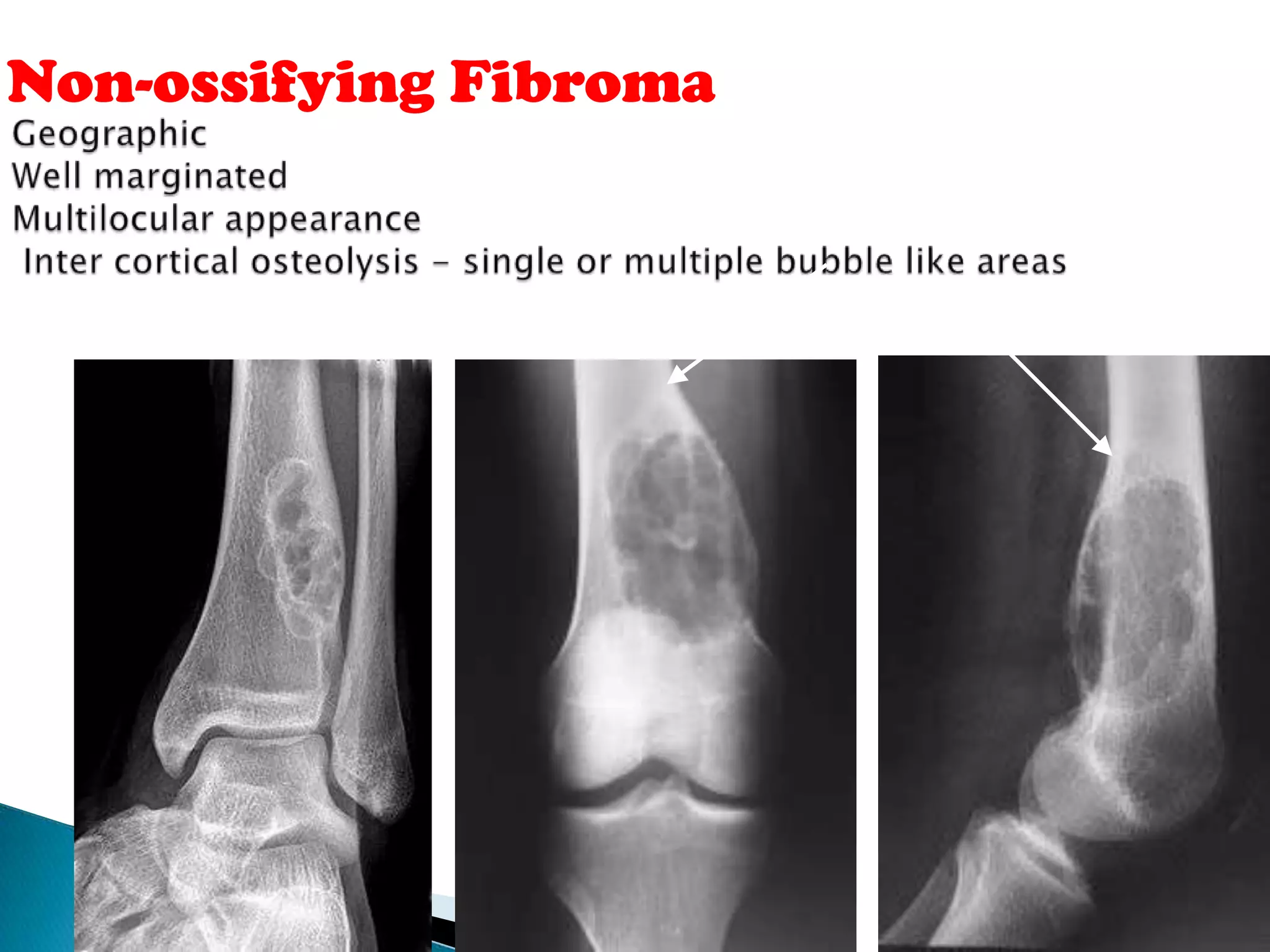
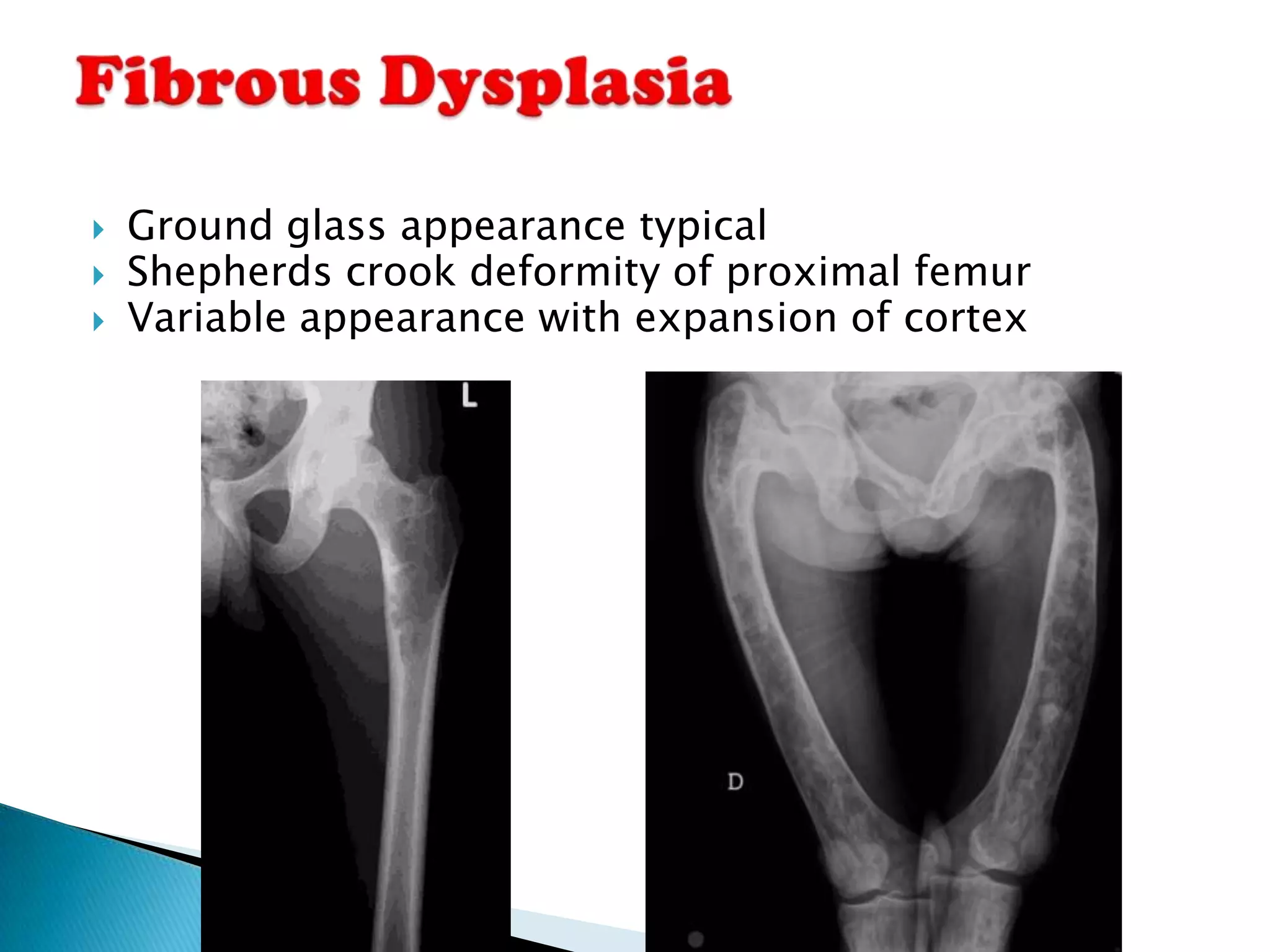
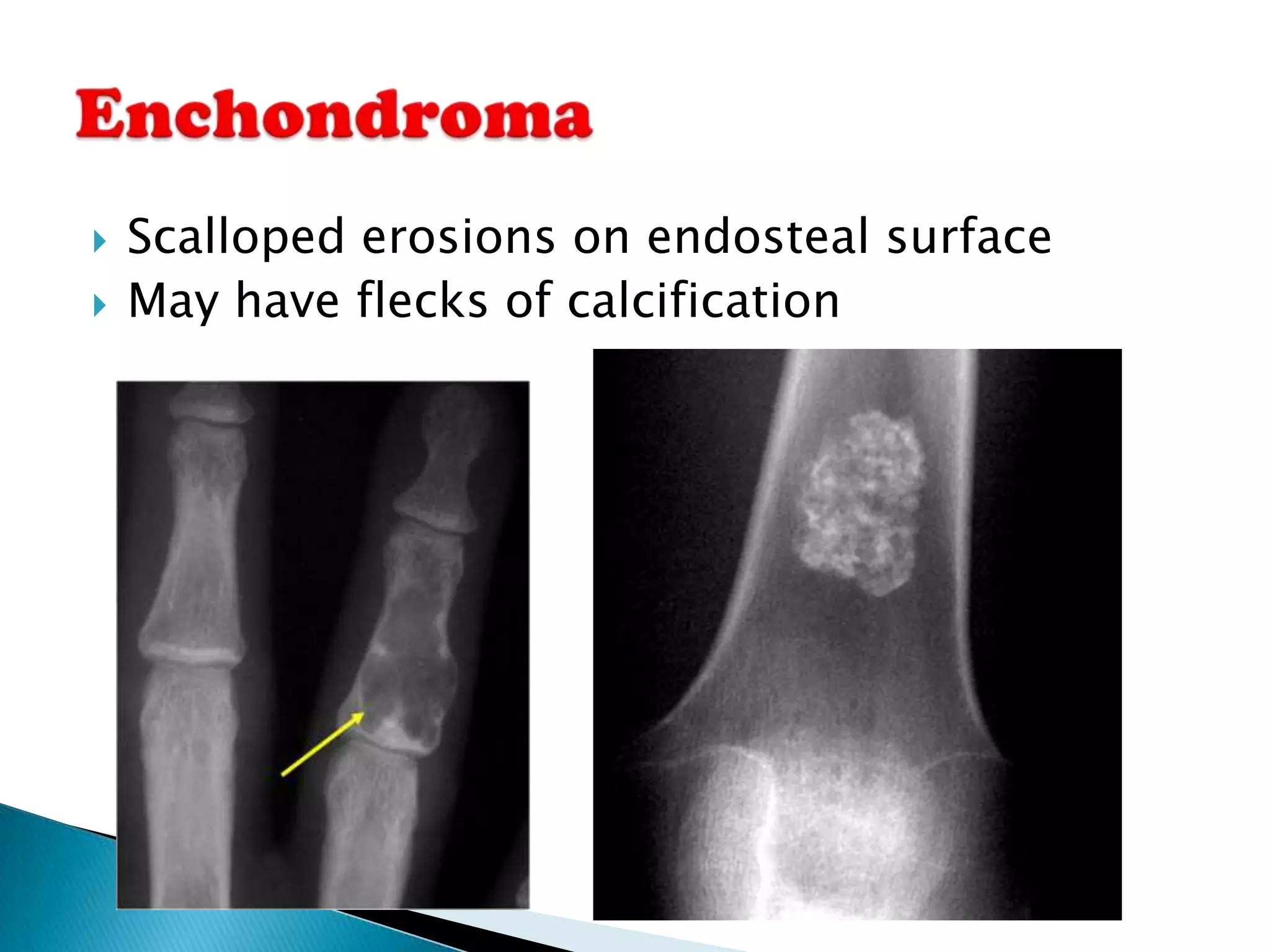
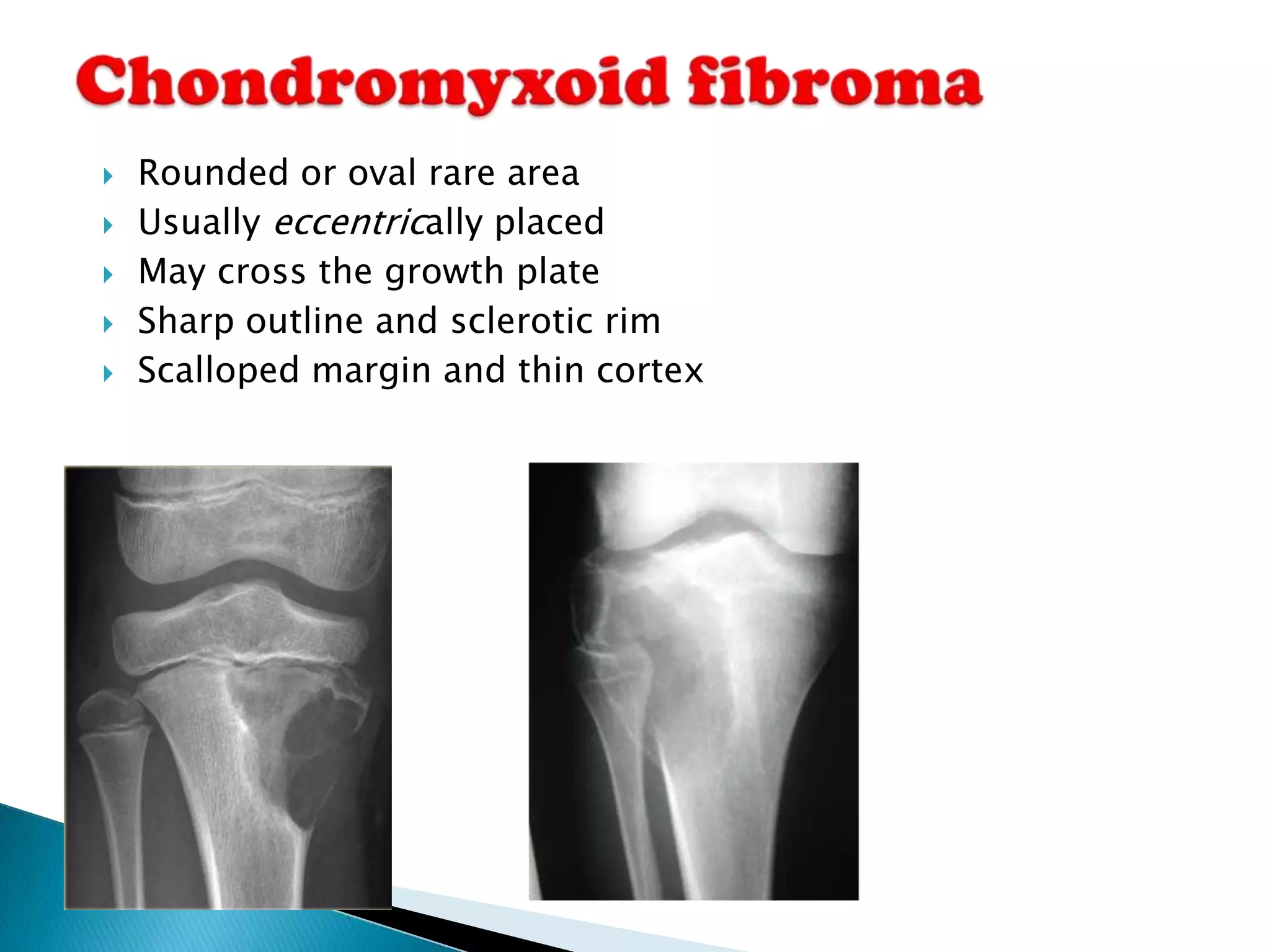
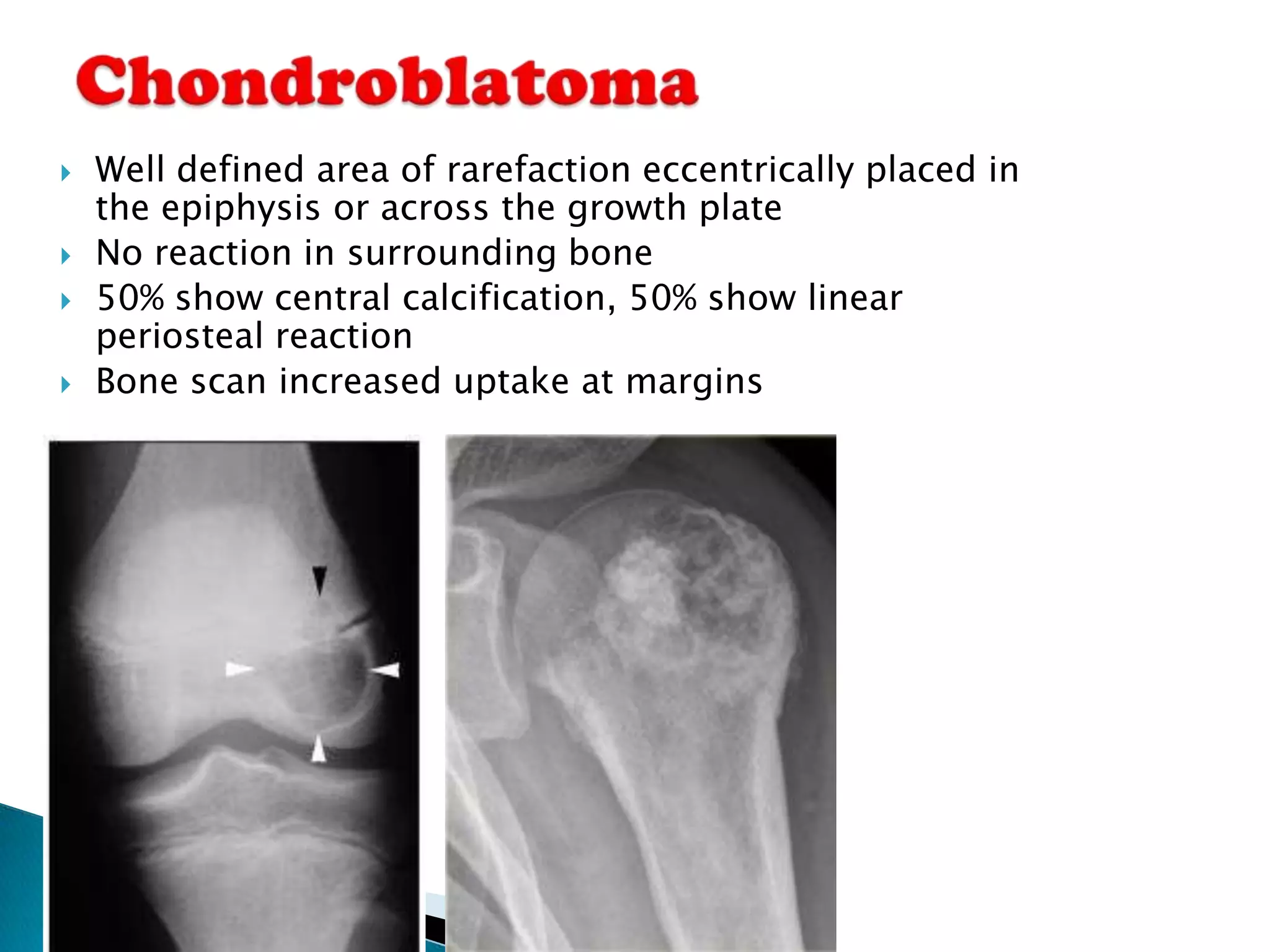
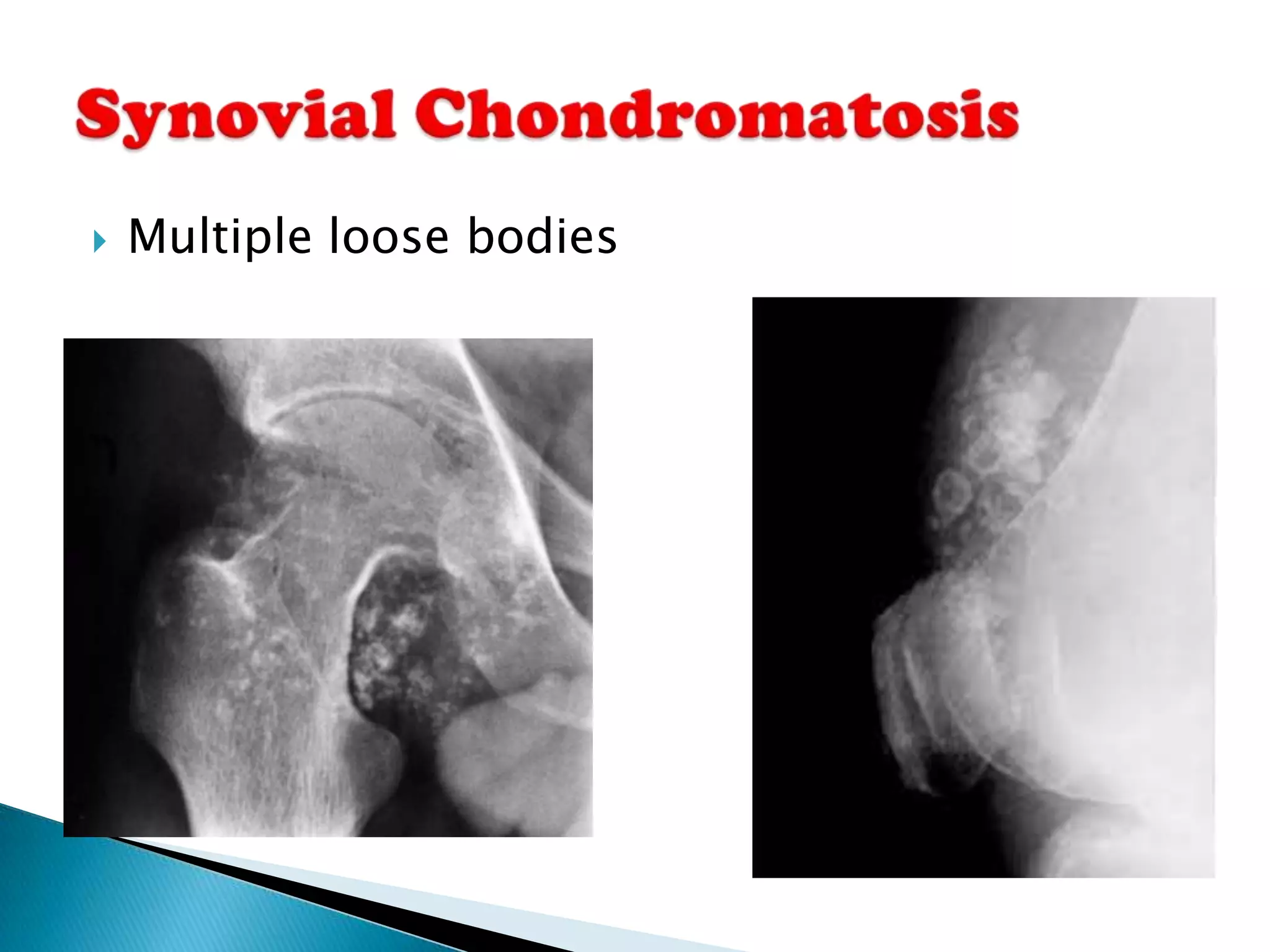
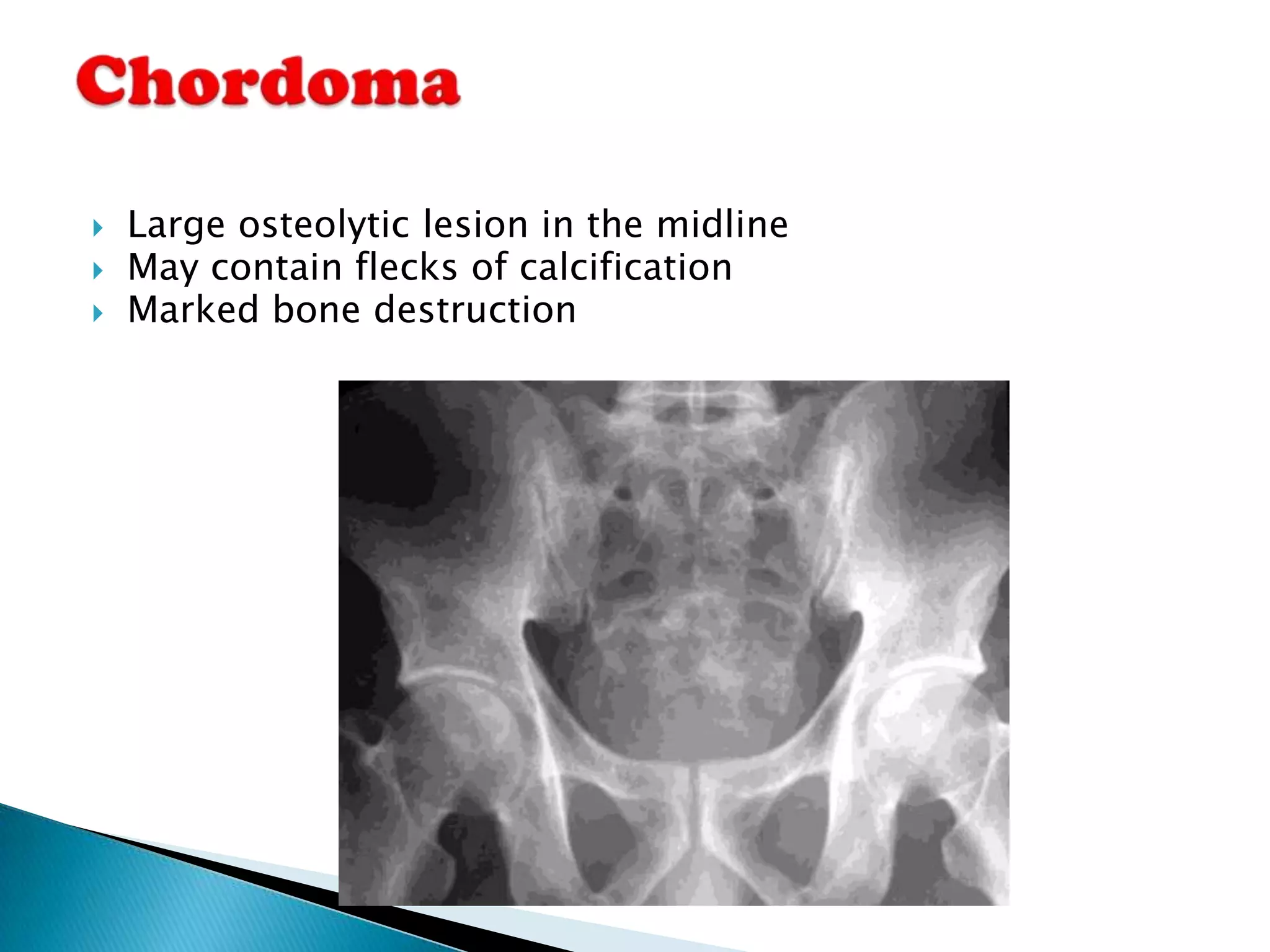
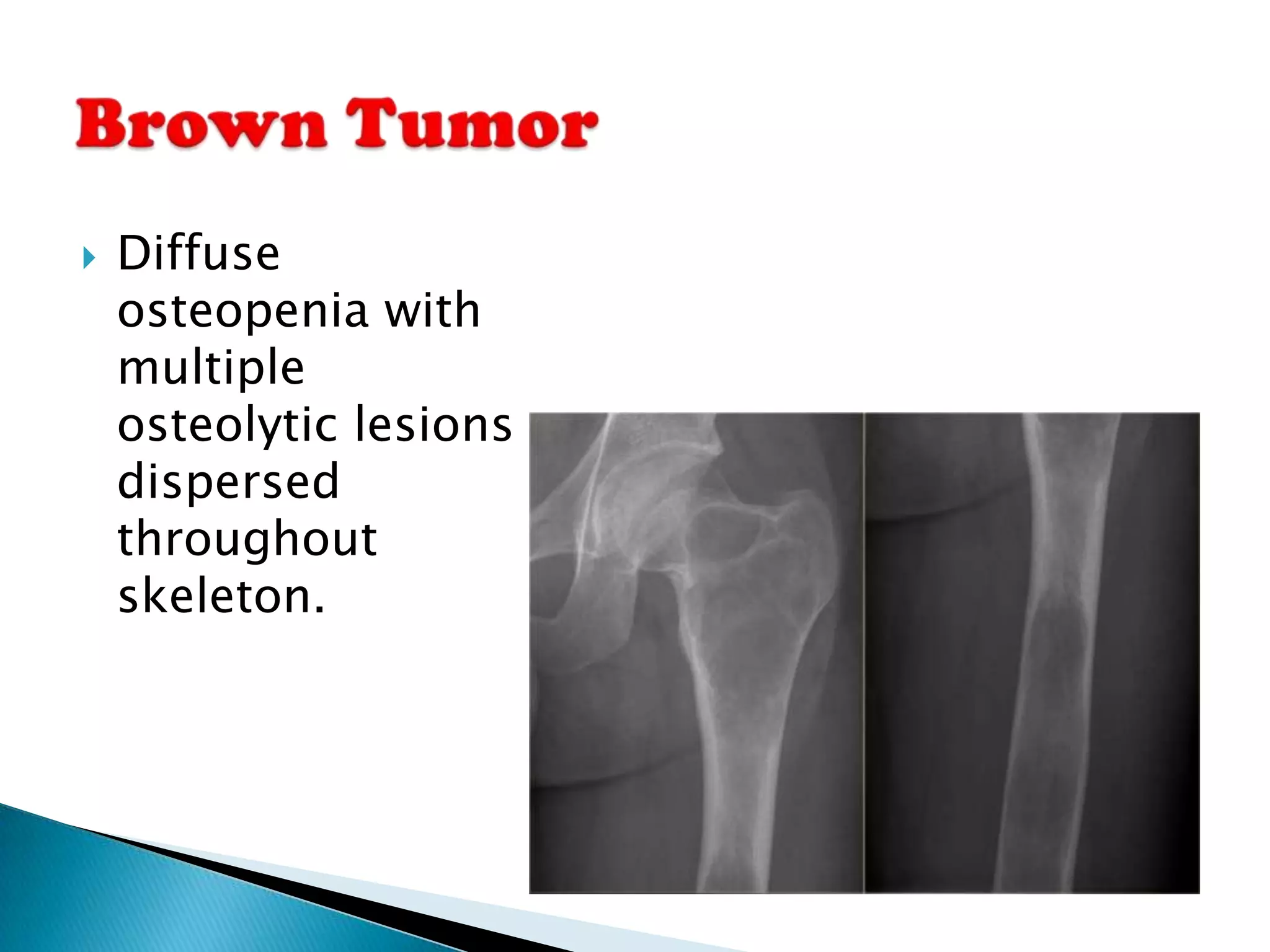
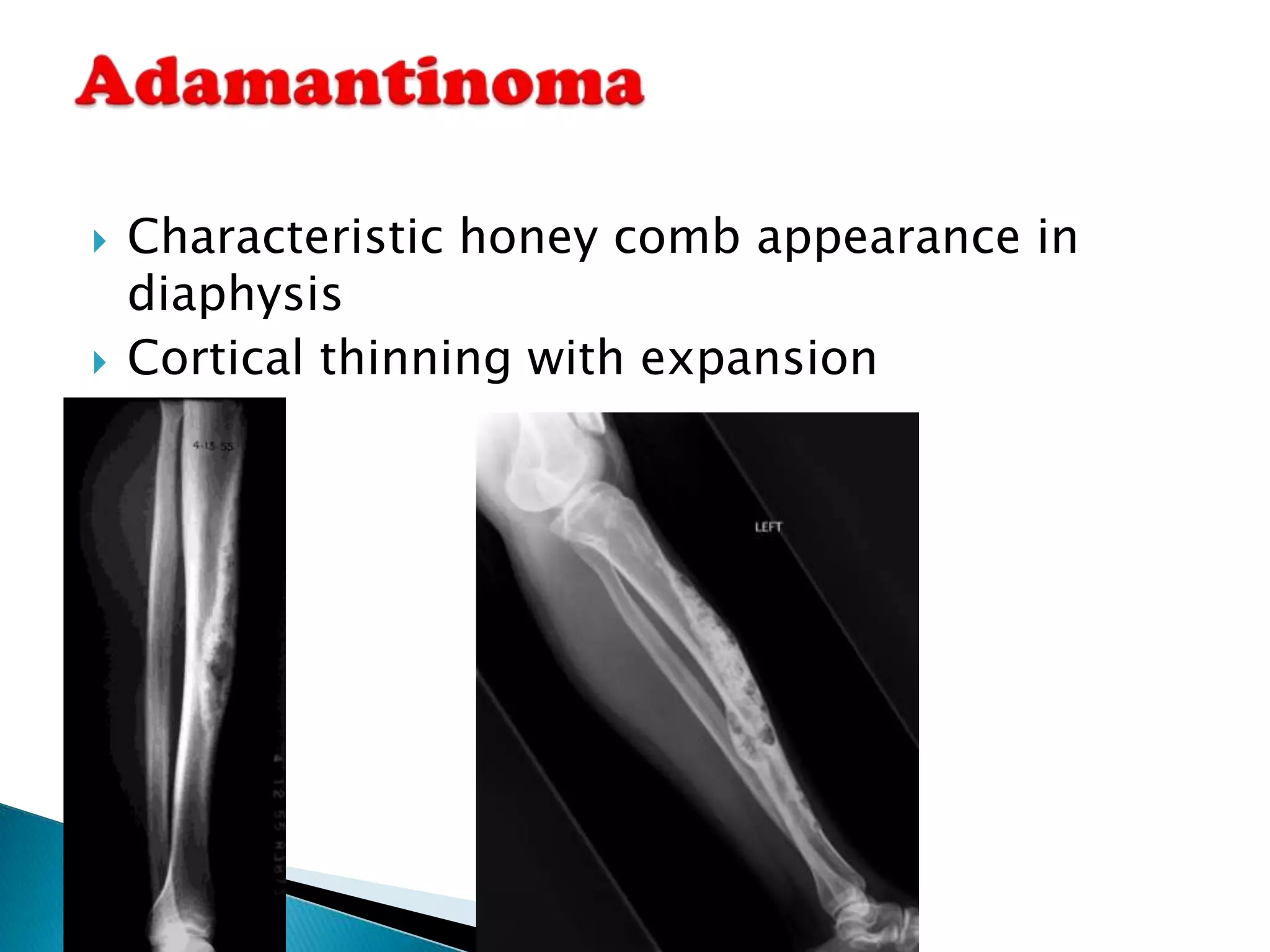
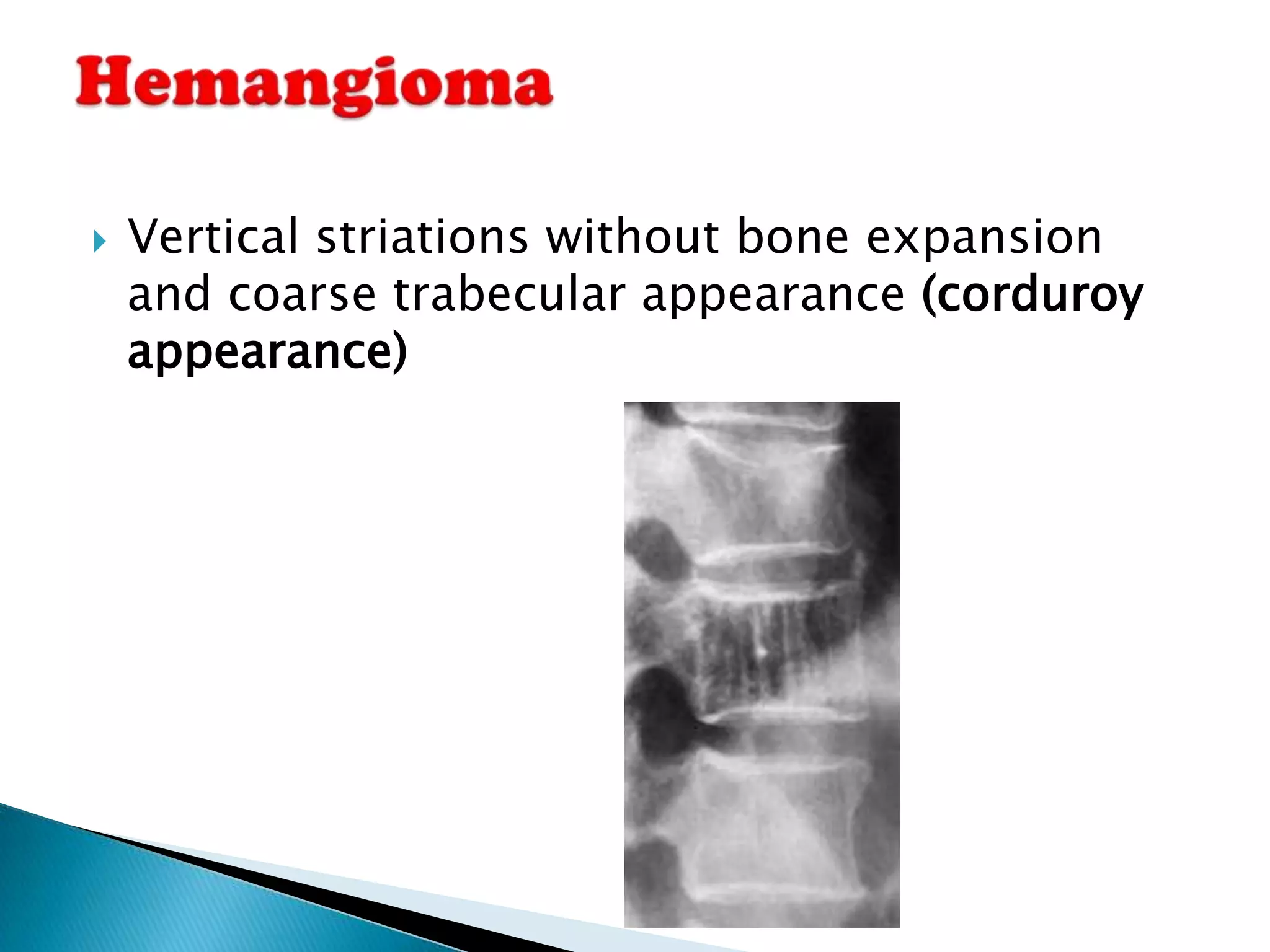
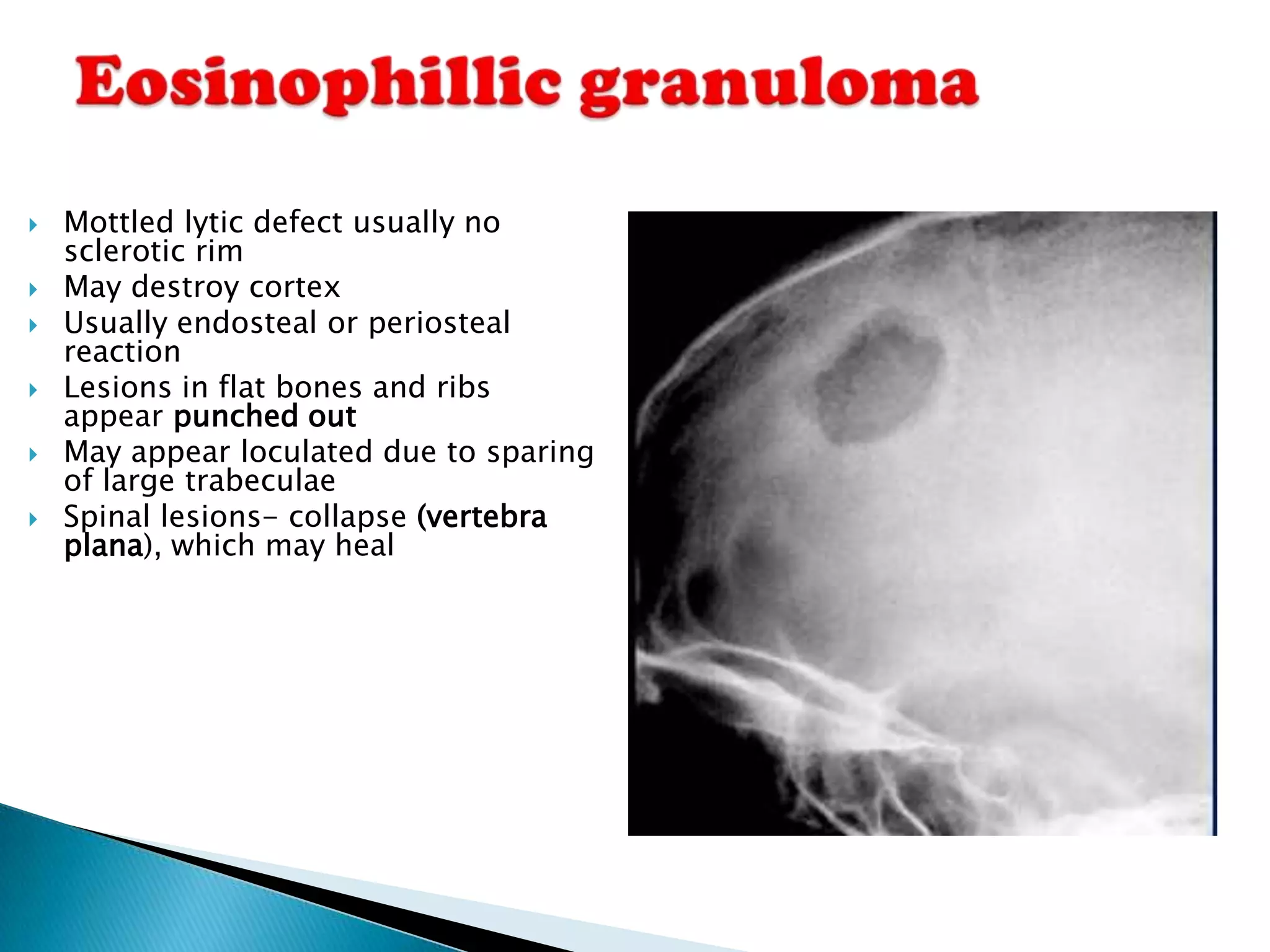
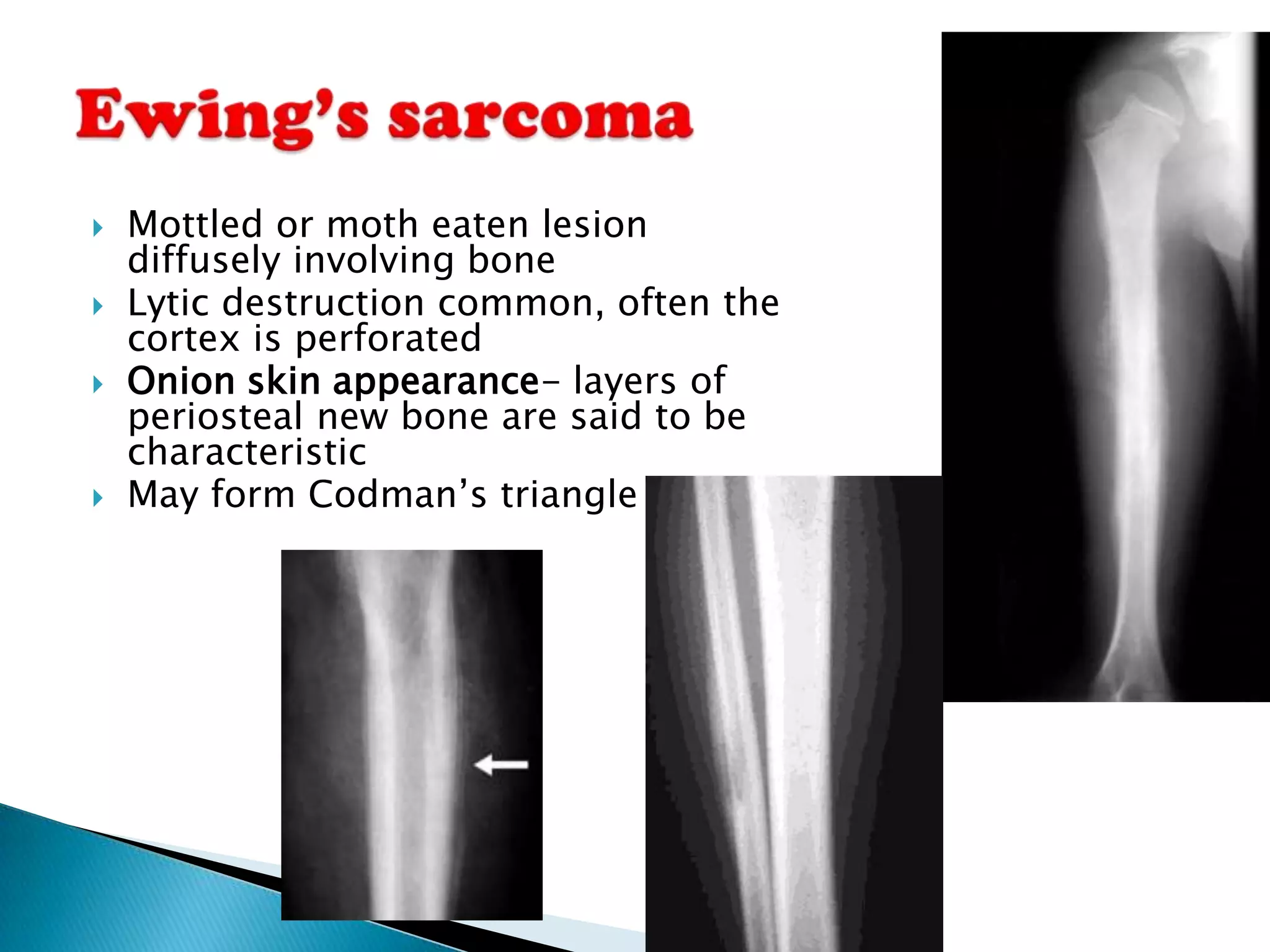
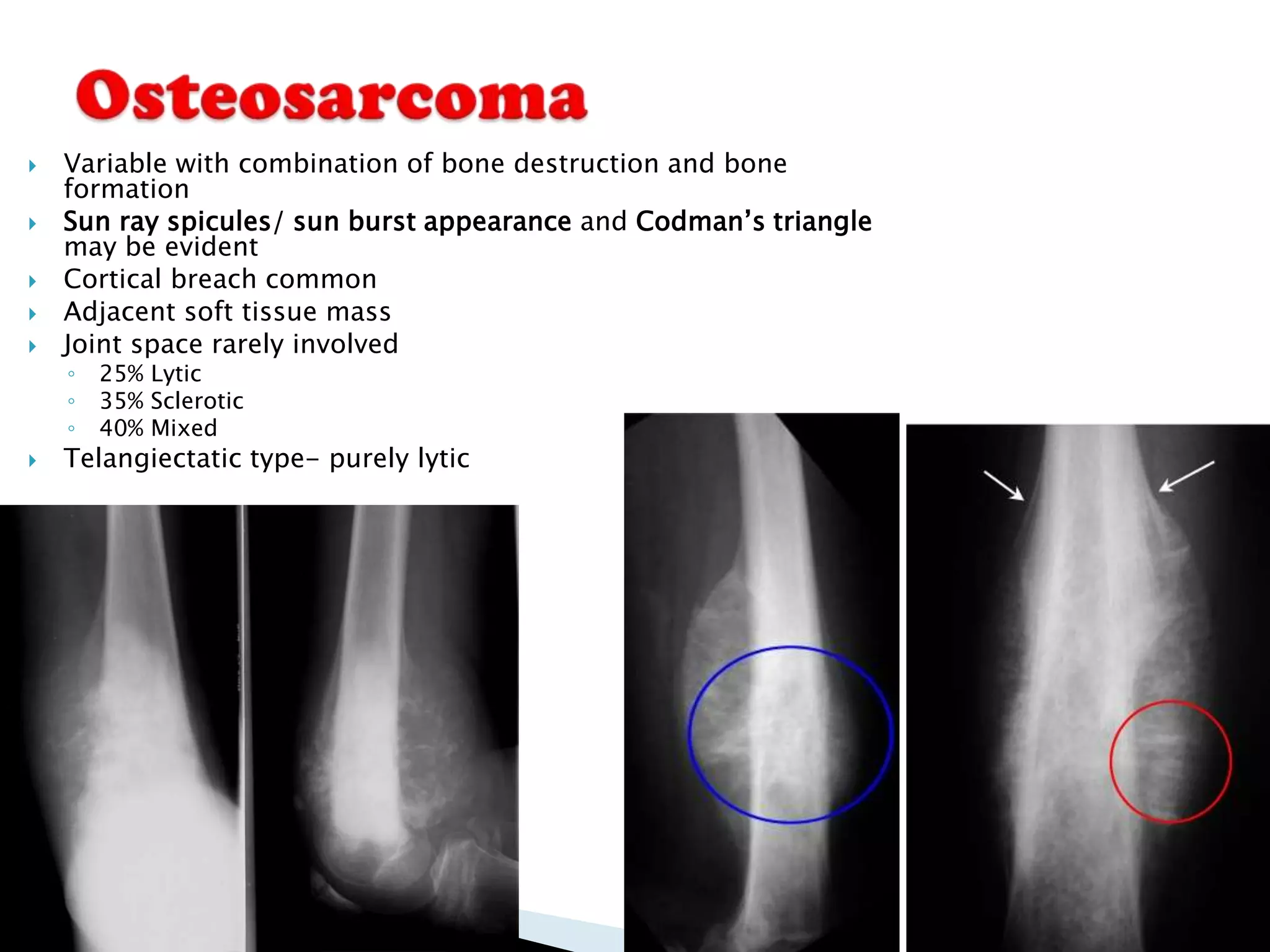
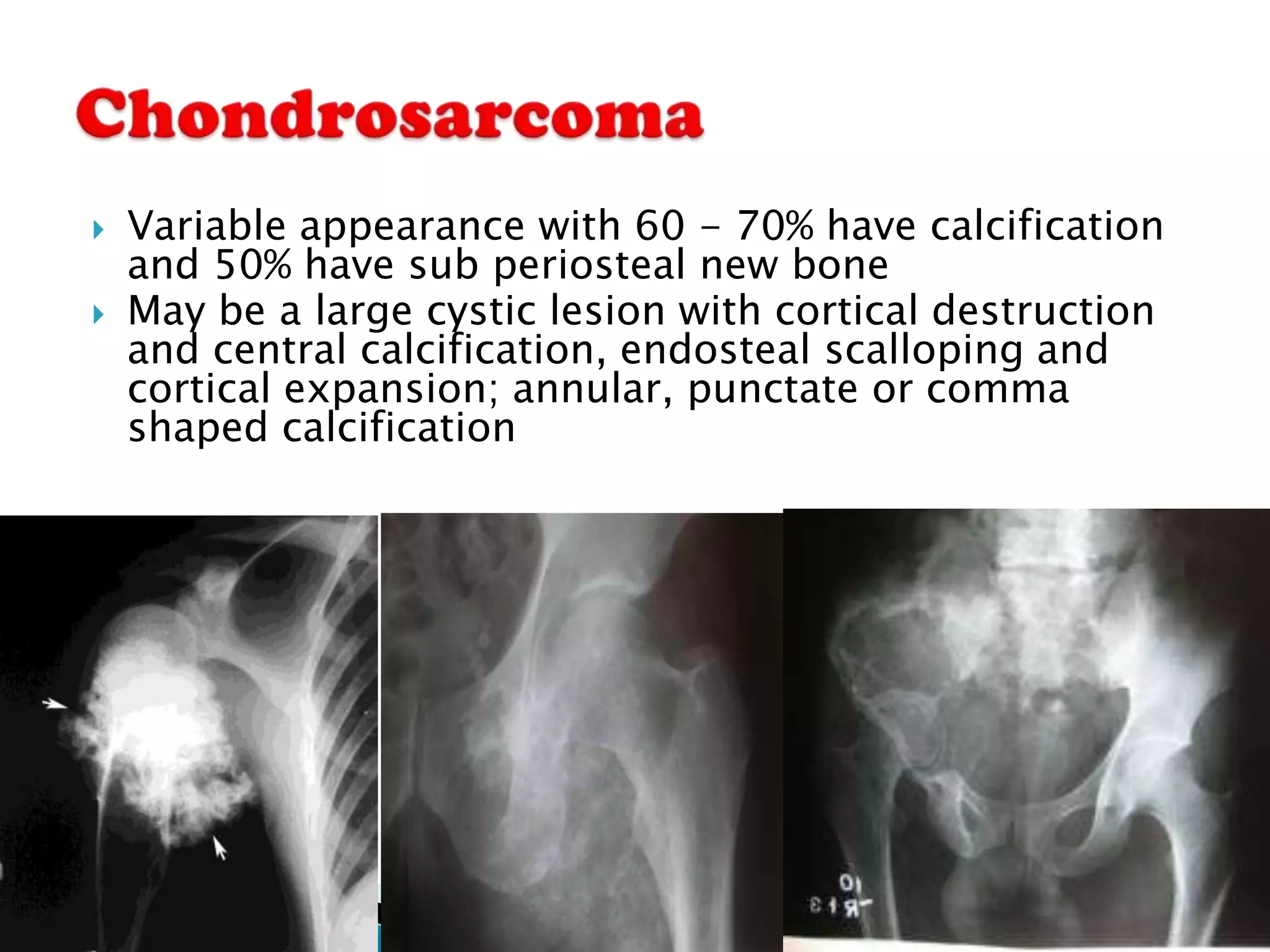
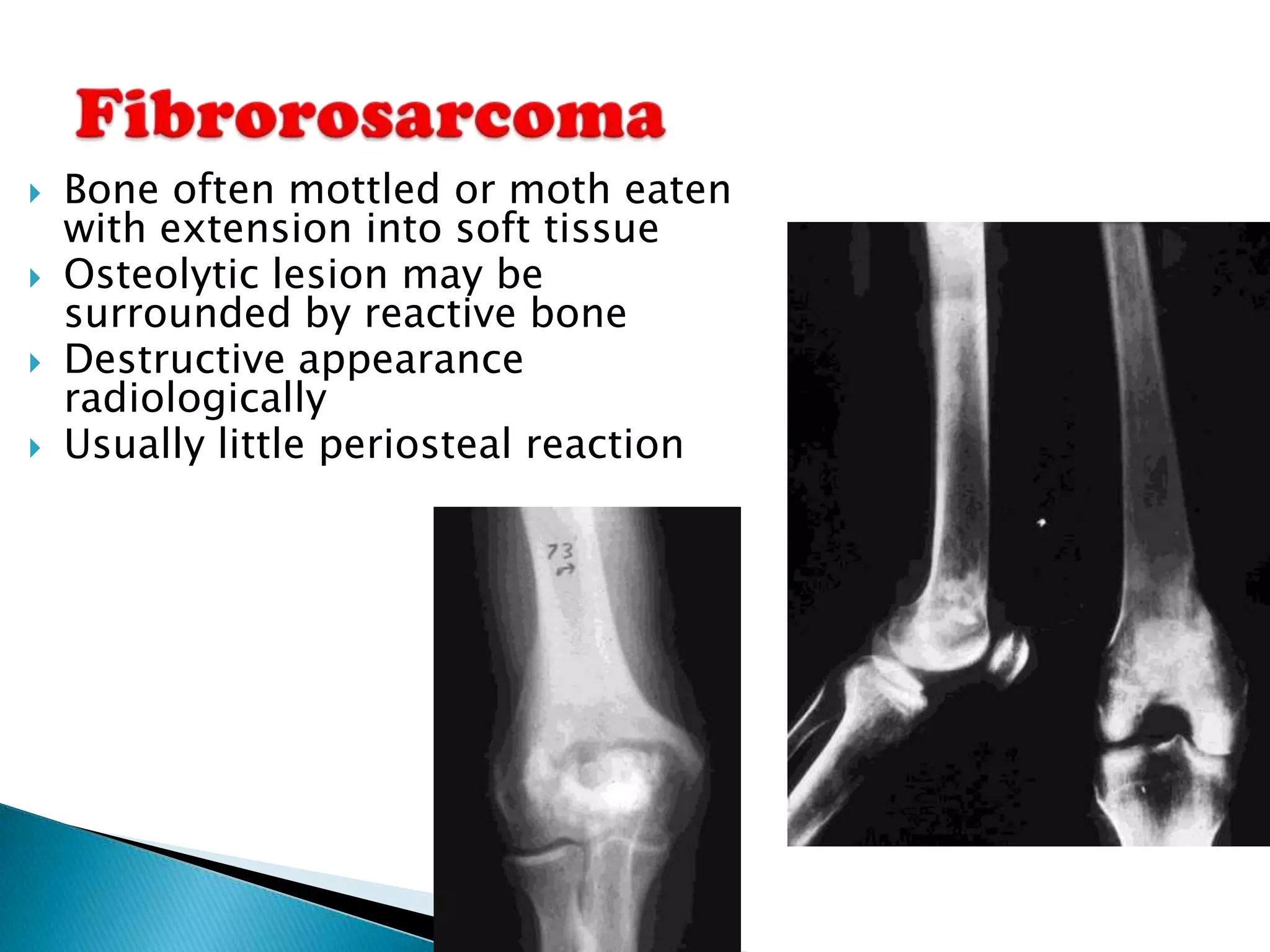
This document discusses how to classify primary bone tumors based on location and age of the patient using plain radiographs. Key factors include the location of the lesion within the bone (epiphyseal, metaphyseal, diaphyseal), the extent of the lesion, and features of the lesion and bone's response that provide clues to the tissue type. Common bone tumors are listed for each location. Characteristic patterns of bone destruction and periosteal reactions are also described.