Valvular Heart Disease
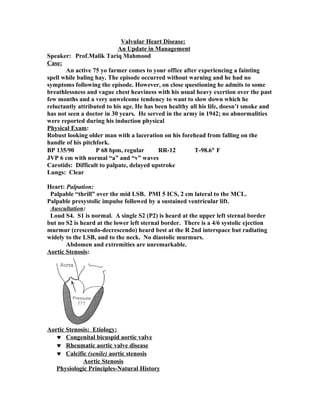
- 1. Valvular Heart Disease: An Update in Management Speaker: Prof.Malik Tariq Mahmood Case: An active 75 yo farmer comes to your office after experiencing a fainting spell while baling hay. The episode occurred without warning and he had no symptoms following the episode. However, on close questioning he admits to some breathlessness and vague chest heaviness with his usual heavy exertion over the past few months and a very unwelcome tendency to want to slow down which he reluctantly attributed to his age. He has been healthy all his life, doesn’t smoke and has not seen a doctor in 30 years. He served in the army in 1942; no abnormalities were reported during his induction physical Physical Exam: Robust looking older man with a laceration on his forehead from falling on the handle of his pitchfork. BP 135/90 P 68 bpm, regular RR-12 T-98.6° F JVP 6 cm with normal “a” and “v” waves Carotids: Difficult to palpate, delayed upstroke Lungs: Clear Heart: Palpation: Palpable “thrill” over the mid LSB. PMI 5 ICS, 2 cm lateral to the MCL. Palpable presystolic impulse followed by a sustained ventricular lift. Auscultation: Loud S4. S1 is normal. A single S2 (P2) is heard at the upper left sternal border but no S2 is heard at the lower left sternal border. There is a 4/6 systolic ejection murmur (crescendo-decrescendo) heard best at the R 2nd interspace but radiating widely to the LSB, and to the neck. No diastolic murmurs. Abdomen and extremities are unremarkable. Aortic Stenosis: Aortic Stenosis: Etiology: ♥ Congenital bicuspid aortic valve ♥ Rheumatic aortic valve disease ♥ Calcific (senile) aortic stenosis Aortic Stenosis Physiologic Principles-Natural History
- 2. • Normal aortic valve area is 3.0 - 4.0 cm2 • Circulation affected when valve area is reduced by ~ 75% (i.e. 0.75 - 1.0 cm2) valve area (cm sq) mean gradient (mm Hg)* Mild > 1.5 < 25 Moderate 1.0 - 1.5 25 - 50 Severe < 0.75 > 50 Aortic Stenosis Physiologic Principles-Natural History: • Primary adaptation is concentric hypertrophy • Latent phase usually lasts decades • Risk of sudden death is very low during this phase • Rate of progression ranges from 0-0.3 cm2/yr. (average rate is 0.12 cm2/yr) • 50% of patients with severe AS do not progress • Cannot predict who will Key Physical Findings in Severe Aortic Stenosis: ♥ Carotid impulse: “parvus et tardus” ♥ JVP: Prominent “a” wave ♥ Heart: Systolic thrill Palpable presystolic impulse (S4) Sustained apical systolic impulse S4 Coarse late peaking systolic ejection murmur (may radiate to neck and/or LSB) Attenuated/absent aortic component of S2 Natural History of Aortic Stenosis: ♥ Long asymptomatic “latent” period ♥ “Cardinal” symptoms of severe aortic stenosis Dyspnea Angina Syncope ♥ Sudden death ♥ Left ventricular dilatation and contractile failure ♥ Endocarditis ♥ Arrhythmias Ventricular tachycardia Conduction system disease Atrial fibrillation Natural History of AS:
- 3. Aortic Stenosis Physiologic Principles-Natural History: • Once symptoms develop, average survival is 2-3 yrs • With LV systolic dysfunction, there may be increased risk of sudden death and permanent LV dysfunction Ross J Jr, Braunwald E: Aortic stenosis. Circulation 38[Suppl V]:61, 1968 Aortic Stenosis Management Guidelines: Initial Diagnostic Testing: Lipids, renal fxn, Ca, P---all patients CXR, ECG, Echocardiography---all patients Cardiac catheterization with angiography If clinical and echo data are discordant To assess coronary circulation prior to surgery Aortic Stenosis Management Guidelines: Initial Diagnostic Testing (cont.) Treadmill stress testing Dangerous in symptomatic pts Not useful for dx of CAD May be used to assess functional significance of severe AS in pts who deny symptoms (e.g. bp response) Aortic Stenosis Management Guidelines: Scheduled Follow-up:
- 4. office intervalecho interval Mild AS 12 mos 5 yrs Moderate AS 6 mos 2 yrs Severe AS 6 mos 1 yr Aortic Stenosis Management Guidelines: Low Gradient AS • Special case • Minimal valve mobility and low cardiac output • Calculated valve area is small but pressure gradient is also small • Functional vs. fixed AS? • Consider dobutamine stress test (DSE) to clarify ACC Classification of Recommendations: Class I: Conditions for which there is evidence and/or general agreement that a given procedure or treatment is useful and effective. Class II: Conditions for which there is conflicting evidence and/or a divergence of opinionabout the usefulness/efficacy of a procedure or treatment. IIa. Weight of evidence/opinion is in favor of usefulness/efficacy IIb. Usefulness/efficacy is less well established by evidence/opinion. Class III: Conditions for which there is evidence and/or general agreement that the procedure/treatment is not useful/effective, and in some cases may be harmful. Aortic Stenosis Management Guidelines: Recommendations for AVR Class I Severe AS and symptoms Severe AS (with or without sxs) and need for CABG, other valve replacement or aortic surgery Class IIa Moderate AS and need for other cardiac surgery Asymptomatic severe AS and diminished LVEF or hypotensive response to exercise Aortic Stenosis Management Guidelines: Recommendations for AVR (cont.) Class IIb Asymptomatic AS and VT, severe LVH (>15mm) or valve area <0.6 cm2 Class III Asymptomatic AS with none of the above CASE:A 52 yo salesman is referred to you for evaluation of a heart murmur. He had applied for a pilot’s license and was denied because of the murmur. He is
- 5. asymptomatic and physically active. He denies chest pain, dyspnea or dizzy spells and gives no history of a murmur being mentioned during his last physical exam five years ago. He has no family history of heart disease. He has never had high blood pressure or diabetes, doesn’t smoke, and takes no medications. A lipid profile done five years ago was reported to be “OK”. Physical Exam: BP - 145/45 P - 78 reg RR - 12 Temp:98.6F Carotids: Very brisk with sharp collapse JVP: 5 with normal ‘a’ and ‘v’ waves Lungs: Clear Heart: Palpation: PMI is enlarged (4fb), in the anterior axillary line Auscultation: S1 normal, S2 soft. A 2/6 early peaking systolic ejection murmur at the upper RSB and a 3/6 holodiastolic blowing murmur, heard best at the lower LSB when you ask the patient to hold his breath in expiration and lean forward. There is a different 2/6 low-pitched diastolic murmur at the apex. Pulses are all very prominent and brisk; audible pulse over the femoral arteries Major Causes of Aortic Regurgitation: Leaflet Dysfunction Aortic Root Dilation Rheumatic fever Systemic hypertension Endocarditis Dissecting aneurysm Trauma Aortitis (syphilis) Bicuspid aortic valve Reiter’s syndrome Rheumatoid arthritis Ankylosing spondylitis Myxomatous degeneration Ehlers-Danlos Ankylosing spondylitis Osteogenesis imperfecta Marfan’s syndrome Pseudoxanthoma elasticum Fenfluramine-phentermine Marfan’s syndrome Annulo-aortic ectasia Physical Findings in Aortic Regurgitation: Wide pulse pressure: Bounding pulses Soft aortic second sound (A2) Early diastolic murmur (blowing) immediately after A2 Upper RSB with root dilation Mid to lower LSB with leaflet dysfunction Systolic murmur at base (similar to aortic stenosis) Austin Flint murmur: mid to late diastolic “rumble” at apex Some Really Neat Physical Findings in Severe Chronic Aortic Regurgitation: ♥ deMusset’s sign: Head bob with each systolic pulsation ♥ Corrigans’s pulses: “Pistol shot” pulses over femoral artery ♥ Mueller’s sign: Pulsation of the uvula ♥ Duroziez’s sign: Systolic/diastolic bruit over femoral arterY
- 6. ♥ Quincke’s pulses: Capillary pulsations seen in the nailbeds ♥ Becker’s sign: Pulsation of retinal arteries and pupils ♥ Hill’s sign: Popliteal BP exceeds brachial BP by > 60 mmHg Pathophysiology of Chronic Aortic Regurgitation: ♥ Slowly progressive diastolic volume overload ♥ Augmented stroke volume with rapid runoff Increased systolic pressure with low diastolic pressure: wide pulse pressure ♥ Progressive left ventricular dilation, some hypertrophy ♥ Increased diastolic compliance with maintenance of normal diastolic pressures initially ♥ Late systolic failure with reduced ejection fraction and CHF
- 7. Additional Testing: ECG: LVH with massive voltage in the lateral precordial leads (V4-V6) Chest X-Ray: Large heart, predominant left ventricular enlargement. No congestive heart failure. Echo: Marked left ventricular dilation, estimated EF 65%. The end diastolic dimension is 65 mm and the end diastolic dimension is 55 mm. Aortic valve: bicuspid and thickened. Doppler: Severe aortic regurgitation. The aorta is slightly enlarged (4.2 mm). Acute Aortic Regurgitation: ♥ Sudden diastolic volume overload without LV dilation: - Acute elevation in left ventricular diastolic pressure◊ pulmonary edema - Acute LV systolic failure ◊ hypotension ♥ Provide inotropic support, vasodilator therapy if tolerated, urgent valve replacement Natural History of Chronic Aortic Regurgitation: ♥ Long asymptomatic phase; may be decades long. ♥ Left ventricular systolic dysfunction ( decline in EF) NOTE!! LV dysfunction may occur in the absence of symptoms ♥ Symptoms associated with LV dysfunction: - Exercise intolerance - Dyspnea on exertion ♥ Angina (rare) ♥ Sudden death (rare) Natural history of aortic regurgitation:
- 8. Aortic Regurgitation Physiologic Principles-Natural History: • LV faces combined pressure and volume load • Primary adaptation is dilatation (eccentric hypertrophy) • Since this adaptation takes time, AR classified as acute or chronic • Acute AR results in sudden increase in LVEDP >>> pulmonary edema and cardiogenic shock Aortic Regurgitation Physiologic Principles-Natural History: • Latent phase of AR, like AS, may last decades • Decompensation when • LV systolic function begins to fail • Progressive LV dilatation occurs • Spherical geometry develops • Initially this is reversible • LV systolic function and ESD are the most important predictors of postop survival and LV function Aortic Regurgitation Physiologic Principles-Natural History • In asymptomatic pts with severe AS and nl LV systolic function, progression is slow • 4.3%/yr develop symptoms of LV systolic dysfunction • 1.3%/yr progress to LV dysfunction without symptoms† pooled data from 7 series. 490 pts with mean follow-up of 6.4 yrs Aortic Regurgitation Management Guidelines: Scheduled Follow-up (office and echo) Severe AR without symptoms • q 4-12 month depending on pace of change and current LV ESD/EDD Moderate AR without symptoms • 1st follow-up in 2-3 months to establish pace, then ~ q 12 months
- 9. Aortic Regurgitation Management Guidelines: Vasodilator Therapy • Expected to ι afterload, η stroke volume and ι regurgitant volume • Hemodynamic benefit shown with hydralazine and nifedipine, less consistent results with ACEi • Improvement in clinical outcomes in trial of LA nifedipine vs. digoxin (need for AVR in 143 pts followed for 6 yrs--- 15% vs 34%) • Dose titrated to achieve ι in SBP, not normalization Aortic Regurgitation Management Guidelines: Vasodilator Therapy Indications Class I • Severe AR with symptoms or severe LV dilatation but contraindications to surgery • Severe AR without symptoms but LV dilatation and elevated SBP • Any degree of AR with hypertension • Persistent LV systolic dysfunction s/p AVR (ACEi) • Short term therapy prior to AVR Aortic Regurgitation Management Guidelines: Vasodilator Therapy Indications Class III • Mild to mod AR without sxs and nl LV function • In lieu of AVR in pts without contraindications Aortic Regurgitation Management Guidelines: Recommendations for AVR (chronic severe AR) Class I • NYHA functional class III or IV sxs • NYHA functional class II sxs and progressive LV dilatation or declining LVEF on serial studies • CCS class II angina • Mild or moderate reduction in EF (25-50%) • Need for CABG or surgery on other valves Aortic Regurgitation Management Guidelines: Class IIa • NYHA class II sxs with nl LVEF (>50%) with stable EF, LV size and exercise tolerance • Asymptomatic pts with nl LVEF but severe LV dilatation (ESD > 55 mm or EDD > 75 mm) Class IIb • LVEF < 25%
- 10. • Asymptomatic pts with nl LVEF and progressive LV dilatation with ESD 50- 55 Valvular Heart Disease Mitral Stenosis A 75 year old woman with loud first heart sound and mid-diastolic murmur: • Chronic dyspnea Class 2/4 • Fatigue • Recent orthopnea/pnd • Nocturnal palpitation • Pedal edema Mitral Stenosis: • Etiology • Symptoms • Physical Exam • Severity • Natural history • Timing of Surgery Mitral Stenosis: Etiology: • Primarily a result of rheumatic fever (~ 99% of MV’s @ surgery show rheumatic damage ) • Scarring & fusion of valve apparatus • Rarely congenital • Pure or predominant MS occurs in approximately 40% of all patients with rheumatic heart disease • Two-thirds of all patients with MS are female. Mitral Stenosis: Pathophysiology • Normal valve area: 4-6 cm2 • Mild mitral stenosis: • MVA 1.5-2.5 cm2 • Minimal symptoms • Mod mitral stenosis • MVA 1.0-1.5 cm2 usually does not produce symptoms at rest • Severe mitral stenosis • MVA < 1.0 cm2 Mitral Stenosis: Symptoms: • Fatigue • Palpitations • Cough • SOB • Left sided failure • Orthopnea • PND
- 11. • Palpitation • Afib • Systemic embolism • Pulmonary infection • Hemoptysis • Right sided failure • Hepatic Congestion • Edema • Worsened by conditions that cardiac output. • Exertion,fever, anemia, tachycardia, Afib, intercourse, pregnancy, thyrotoxicosis Recognizing Mitral Stenosis Palpation: • Small volume pulse • Tapping apex-palpable S1 • +/- palpable opening snap (OS) • RV lift • Palpable S2 ECG: • LAE, AFIB, RVH, RAD Auscultation: • Loud S1- as loud as S2 in aortic area • A2 to OS interval inversely proportional to severity • Diastolic rumble: length proportional to severity • In severe MS with low flow- S1, OS & rumble may be inaudible Mitral Stenosis: Physical Exam • First heart sound (S1) is accentuated and snapping • Opening snap (OS) after aortic valve closure • Low pitch diastolic rumble at the apex • Pre-systolic accentuation (esp. if in sinus rhythm) Common Murmurs and Timing (click on murmur to play) Systolic Murmurs • Aortic stenosis • Mitral insufficiency • Mitral valve prolapse • Tricuspid insufficiency Diastolic Murmurs • Aortic insufficiency • Mitral stenosis Auscultation- Timing of A2 to OS Interval: • Width of A2-OS inversely correlates with severity
- 12. • The more severe the MS the higher the LAP the earlirthe LV pressure falls below LAP and the MV opens Mitral Stenosis: Natural History: • Progressive, lifelong disease, • Usually slow & stable in the early years. • Progressive acceleration in the later years • 20-40 year latency from rheumatic fever to symptom onset. • Additional 10 years before disabling symptoms Mitral Stenosis: Complications: • Atrial dysrrhythmias • Systemic embolization (10-25%) • Risk of embolization is related to, age, presence of atrial fibrillation, previous embolic events • Congestive heart failure • Pulmonary infarcts (result of severe CHF) • Hemoptysis • Massive: 20 to ruptured bronchial veins (pulm HTN) • Streaking/pink froth: pulmonary edema, or infection • Endocarditis • Pulmonary infections Mitral Stenosis: EKG: • LAE • RVH • Premature contractions • Atrial flutter and/or fibrillation • freq. in pts with mod-severe MS for several years • A fib develops in ≈ 30% to 40% of pts w/symptoms A 75 year old woman with loud first heart sound and mid-diastolic murmer:
- 13. Mitral Stenosis: Role of Echocardiography: • Diagnosis of Mitral Stenosis • Assessment of hemodynamic severity • mean gradient, mitral valve area, pulmonary artery pressure • Assessment of right ventricular size and function. • Assessment of valve morphology to determine suitability for percutaneous mitral balloon valvuloplasty • Diagnosis and assessment of concomitant valvular lesions • Reevaluation of patients with known MS with changing symptoms or signs. • F/U of asymptomatic patients with mod-severe MS Mitral Stenosis:Therapy:
- 14. • Medical • Diuretics for LHF/RHF • Digitalis/Beta blockers/CCB: Rate control in A Fib • Anticoagulation: In A Fib • Endocarditis prophylaxis • Balloon valvuloplasty • Effective long term improvement Recommendations for Mitral Valve Repair for Mitral Stenosis: • ACC/AHA Class I • Patients with NYHA functional Class III-IV symptoms, moderate or severe MS (mitral valve area <1.5 cm 2 ),*and valve morphology favorable for repair if percutaneous mitral balloon valvotomy is not available • Patients with NYHA functional Class III-IV symptoms, moderate or severe MS (mitral valve area <1.5 cm 2 ),*and valve morphology favorable for repair if a left atrial thrombus is present despite anticoagulation • Patients with NYHA functional Class III-IV symptoms, moderate or severe MS (mitral valve area <1.5 cm 2 ),* and a non-pliable or calcified valve with the decision to proceed with either repair or replacement made at the time of the operation. Recommendations for Mitral Valve Repair for Mitral Stenosis: • ACC/AHA Class IIB • Patients in NYHA functional Class I, moderate or severe MS (mitral valve area <1.5 cm 2 ),* and valve morphology favorable for repair who have had recurrent episodes of embolic events on adequate anticoagulation. ACC/AHA Class III Patients with NYHA functional Class I-IV symptoms and mild MS. *The committee recognizes that there may be a variability in the measurement of mitral valve area and that the mean trans-mitral gradient, pulmonary artery wedge pressure, and pulmonary artery pressure at rest or during exercise should also be considered. Mitral Stenosis Physiology/Natural History: • Normal MVA 4 -5 cm2 • Symptoms not apparent until area < 2.5 cm2 • valve area (cm sq) mean gradient (mmHg)* Mild > 1.5 < 5 Moderate 1.0 - 1.5 5 -10 Severe < 1.0 > 10 Mitral Stenosis Physiology/Natural History: • Akin to severe diastolic dysfunction • V = IR (electrical) • P = QR (hydraulic) • Q = P/Rvalve
- 15. Mitral Stenosis Physiology/Natural History: • LA pressure → PV pressure → interstitial edema → ± alveolar flooding • Adaptations: -pulmonary vascular constriction, intimal hyperplasia, medial hypertrophy → reversible pulmonary hypertension → ± fixed pulm htn -downregulation of neuroreceptors, lymphatic drainage Mitral Stenosis Physiology/Natural History: • Latent (subclinical) phase in RHD 20-40 yrs • 10 yrs of symptoms before disabling • With physically limiting symptoms • 10 yr survival 0-15% • 10-20% systemic embolism • 30-40% develop AF • With onset of severe pulm hypertension • Mean survival < 3 yrs Mitral Stenosis Management Guidelines: Initial Evaluation • History • Physical • ECG • CXR • Echocardiogram • ± Exercise echocardiogram Mitral Stenosis Management Guidelines: Medical Therapy • Rheumatic fever prophylaxis • Infective endocarditis prophylaxis • Limitation of strenuous physical activities • Control of HR (negative chronotropes) • Na restriction, intermittent diuretic use • Prompt management of AF Mitral Stenosis Management Guidelines: Interventional and Surgical Options • Percutaneous mitral balloon valvotomy (PMBV) • Closed commissurotomy (obselete) • Open commissurotomy • Mitral valve replacement Mitral Stenosis Management Guidelines:
- 16. Indications for PMBV (class I and IIa) • Suitable anatomy, no LA clot, ≤ mild MR • Symptomatic pts (NYHA class II-IV) with MVA <1.5 cm2 • Asymptomatic pts with MVA <1.5 cm2 and PASP 50 mmHg at rest, 60 with exercise Mitral Stenosis Management Guidelines: Indications for MVR (class I and IIa) • Symptomatic pts (NYHA class III and IV) with MVA < 1.5 cm2 unsuitable for PMBV • NYHA class I and II pts with MVA < 1.0 cm2 and PASP >60 at rest unsuitable for PMBV Acute Mitral Regurgitation Management Guidelines: Medical Stabilization (while gathering OR team) • If normotensive: nitroprusside • If hypotensive: nitroprusside + dobutamine or intra-aortic balloon pump (IABP) Case 4 • On exam: • obese, loquacious man with petite wife • HR 86. BP 170/94. BMI 45. • JVP 12 cm H2O. Nl carotid upstrokes • diminished bs, no crackles • apical impulse not palpable • Neither S1 or S2 are well heard, obscured by a holosystolic blowing murmur at apex and left parasternal border Case 4: • ECG: • SR, RAD, LA abn, R>S in V1, NSSTT abn • CXR: • LA and LV enlargement • Echo: • severe LA enlargement, mild LV dilatation (ESD 45mm), nl LVEF (60%), pulmonary hypertensio (est PASP 55 mmHg) Chronic Mitral Regurgitation Physiology and Natural History: • Gradual development allows adaptation • LA dilatation and increase in compliance • LV dilatation and EF (via preload and ↓ afterload) → maintenance of forward SV • Compensation often adequate for vigorous exercise • May last many years
- 17. Chronic Mitral Regurgitation Physiology and Natural History: • Eventually, volume overload → LV decompensation • Preop LVEF (>60%) and LVESD (<45 mm) are primary predictors of postop survival Acute Mitral Regurgitation Physiology and Natural History: • Abrupt volume load---no time for adaptation • Sudden ↓ in forward stroke volume • Sudden in LA volume/pressure → PV pressure • Rapidly fatal Chronic Mitral Regurgitation Management Guidelines: Initial evaluation • History • Physical Exam • ECG • CXR • Echo • ± Exercise echo Chronic Mitral Regurgitation Management Guidelines Scheduled Follow-up* Instruct all pts to report any cv symptoms office intervalecho interval Mild MR 12 mos if sxs Moderate MR 12 mos 1-2 yrs Severe MR 6-12 mos 6-12 mos** Chronic Mitral Regurgitation Management Guidelines: Medical Therapy • No generally accepted rx in asymptomatic pts • No long term studies suggesting benefit of afterload reduction in absence of hypertension • ACEi if hypertensive • AF requires rate control, anticoagulation and 1 attempt at restoration of SR Chronic Mitral Regurgitation Management Guidelines: Surgical Options • Mitral valve repair • Mitral valve replacement with preservation of subvalvular apparatus • Mitral valve replacement with excision of subvalvular apparatus • MVR with CABG (in ischemic MR)
