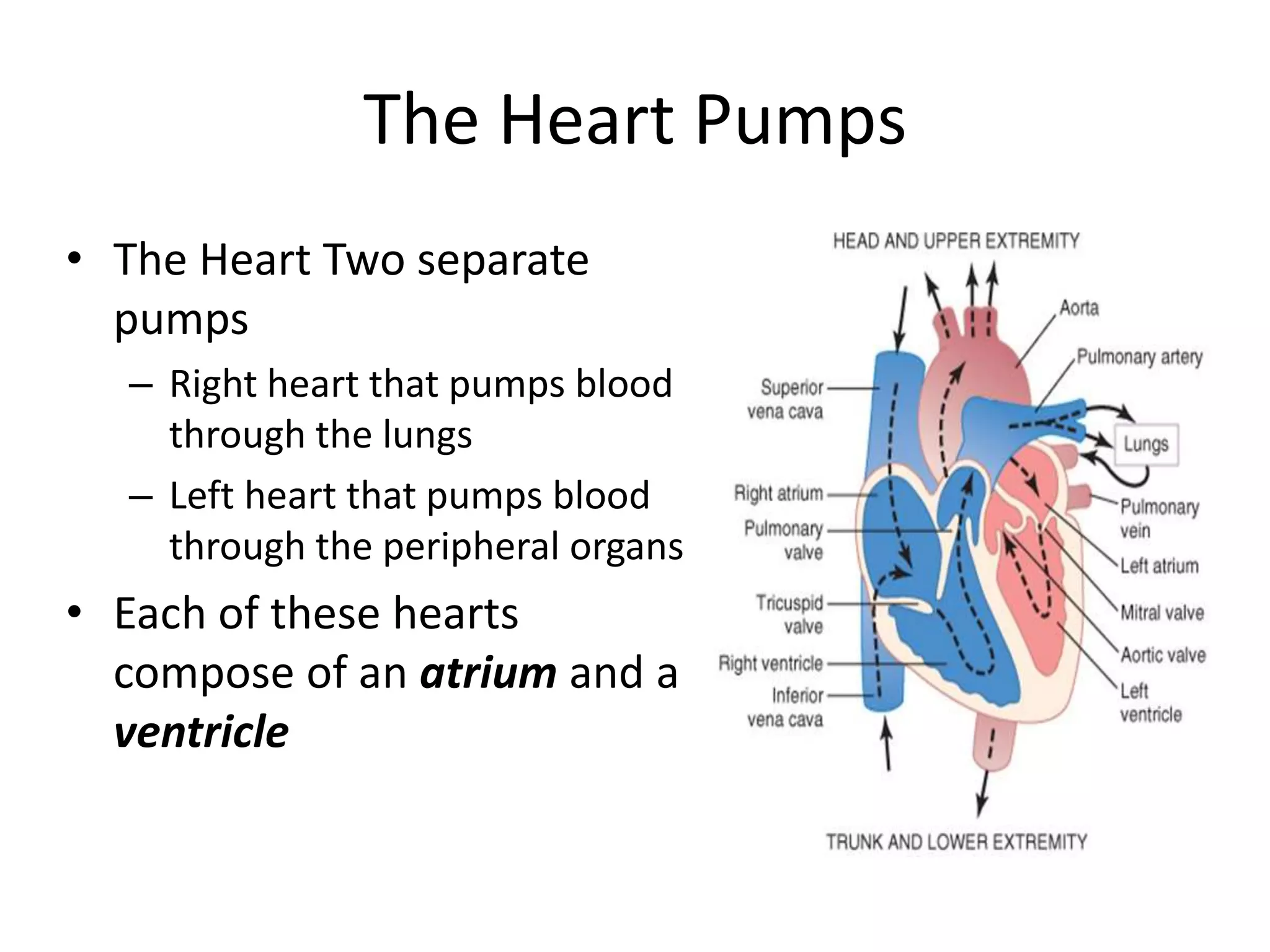
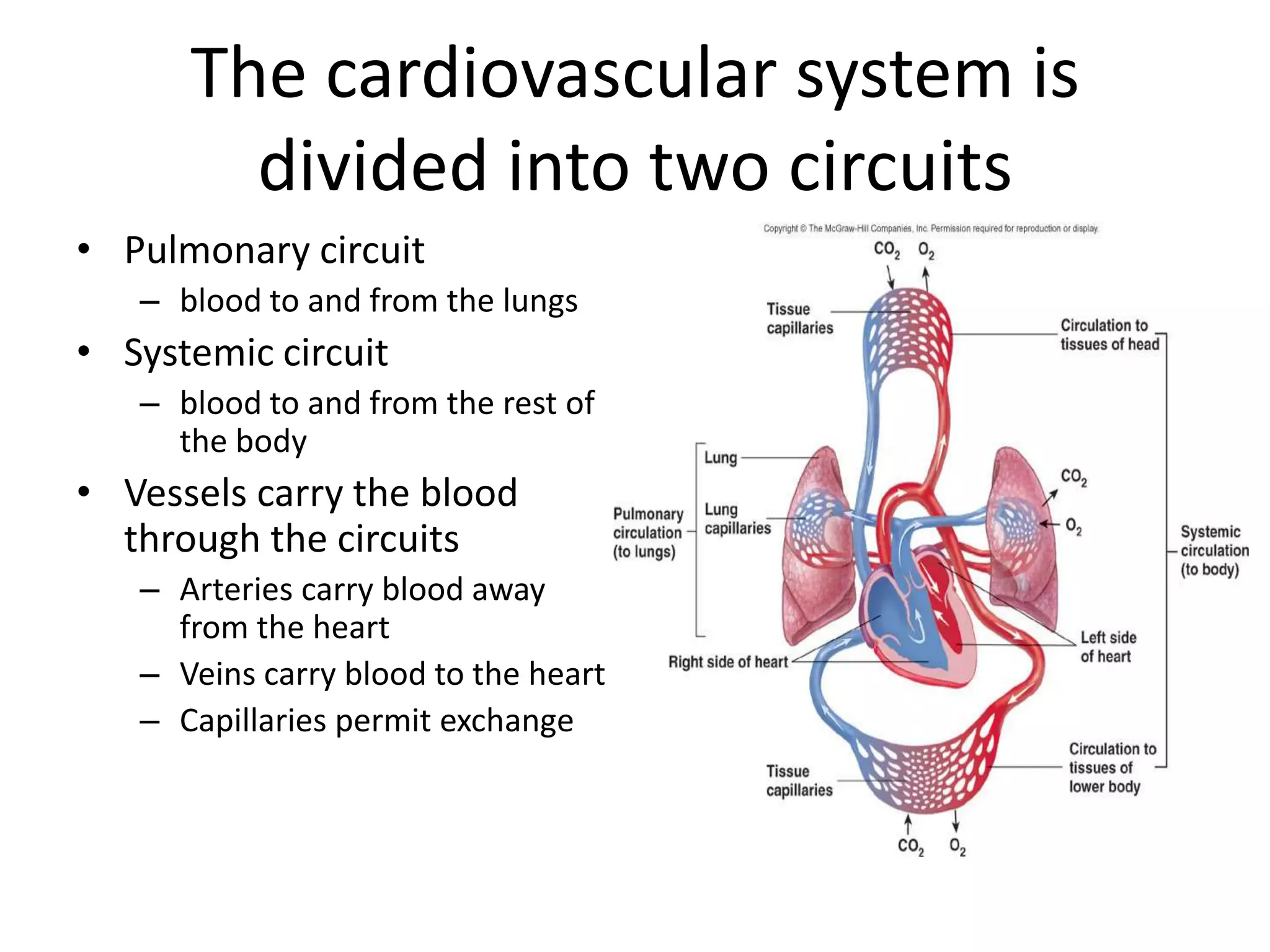
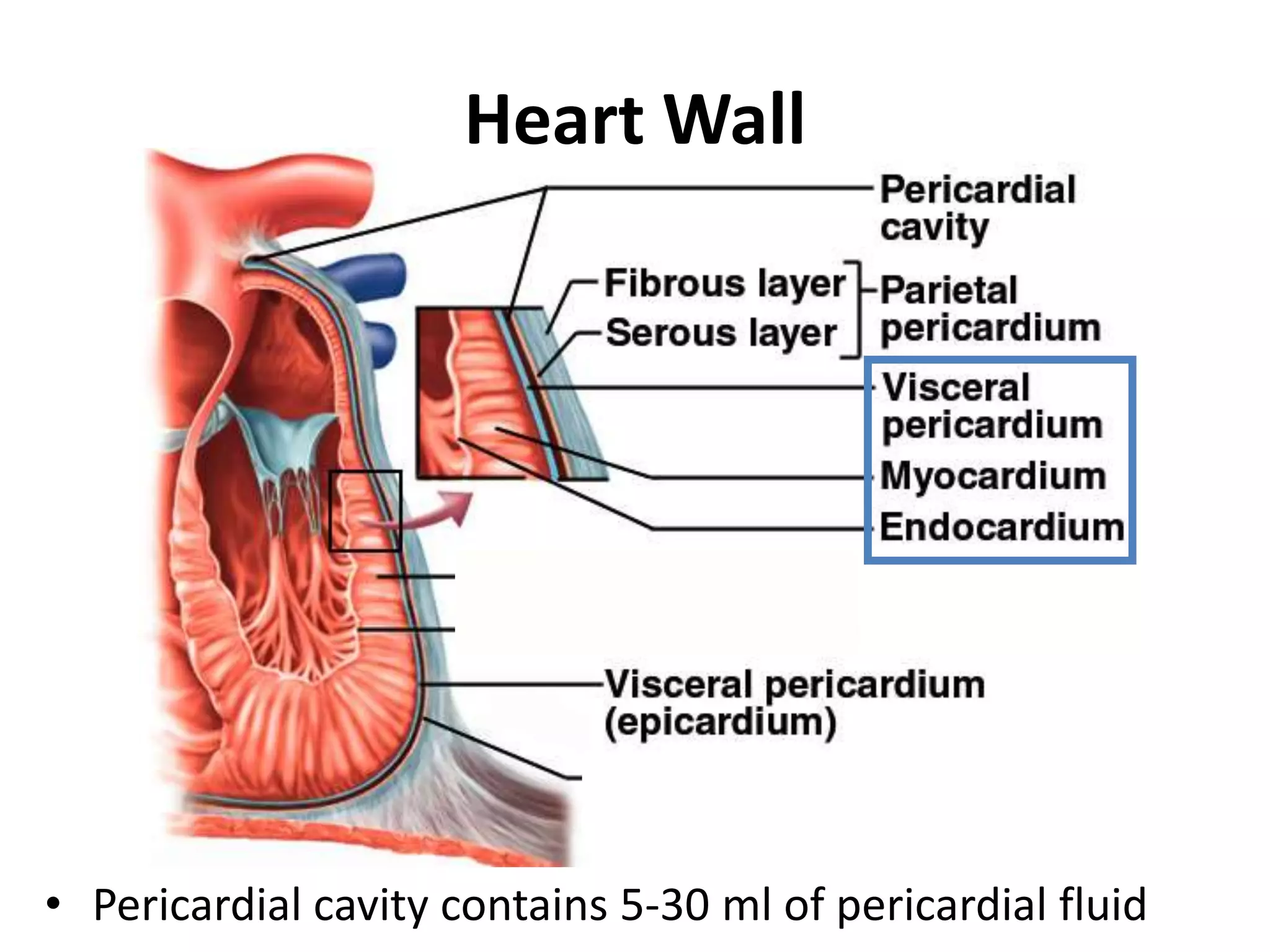
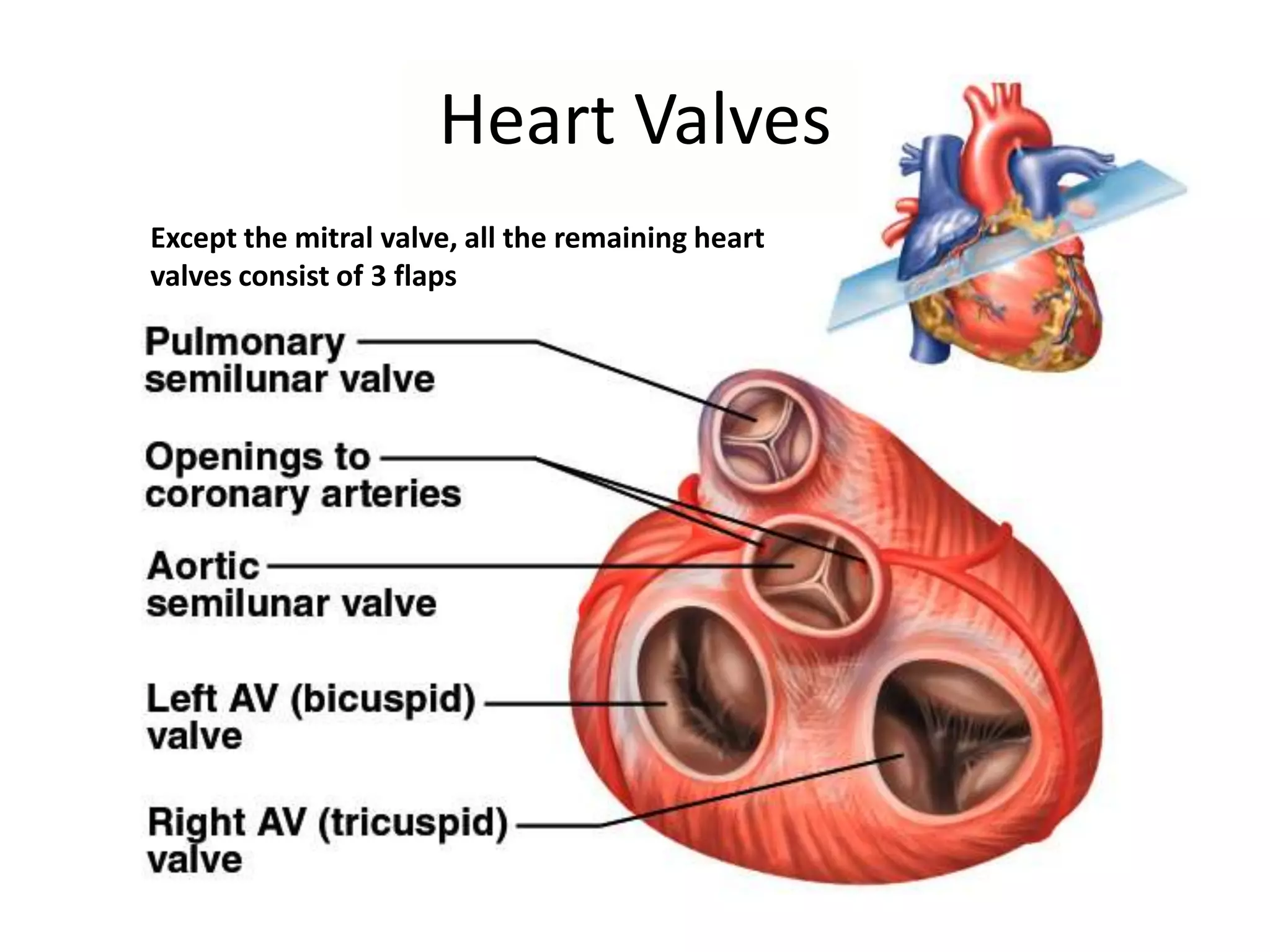
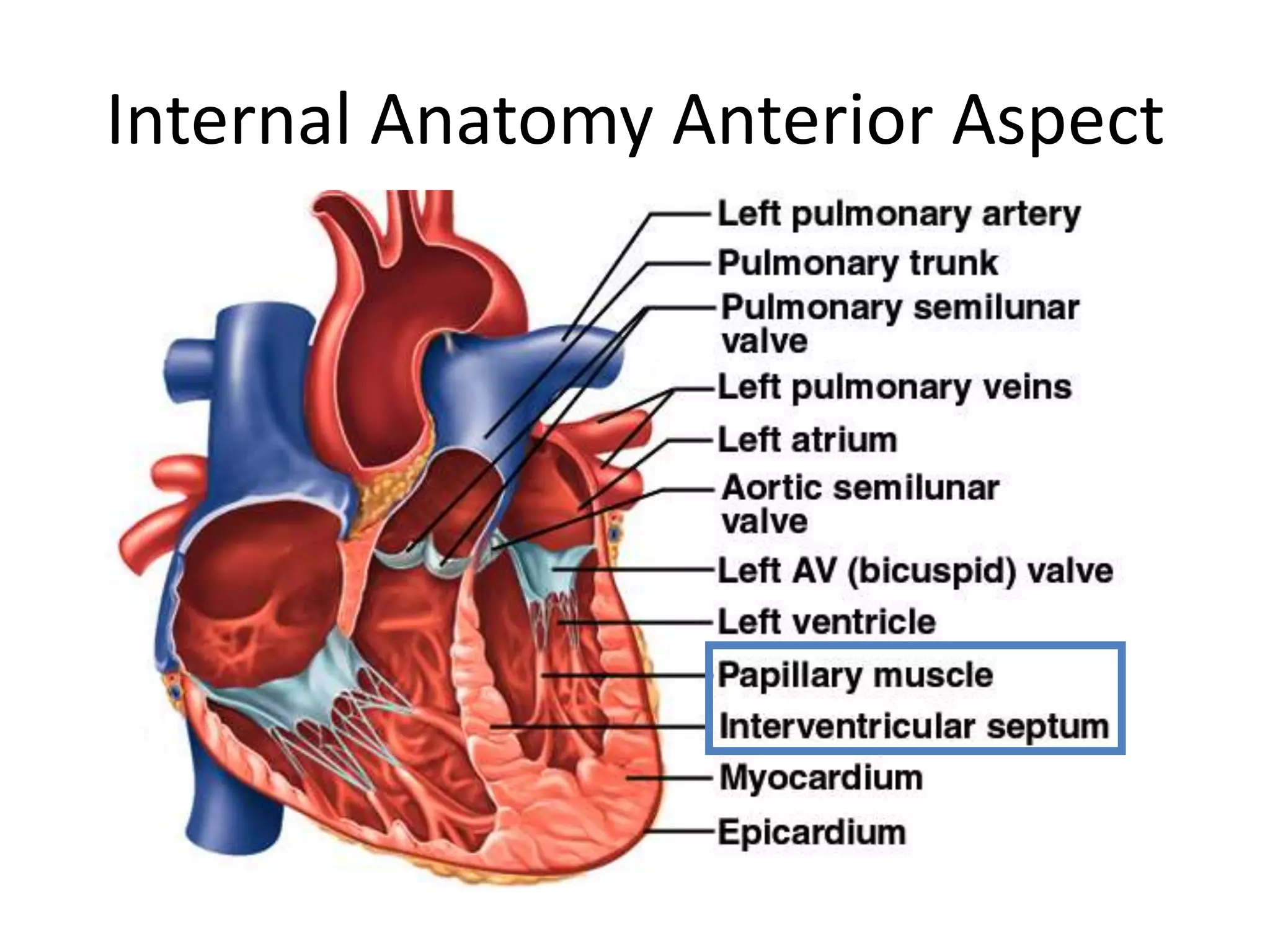
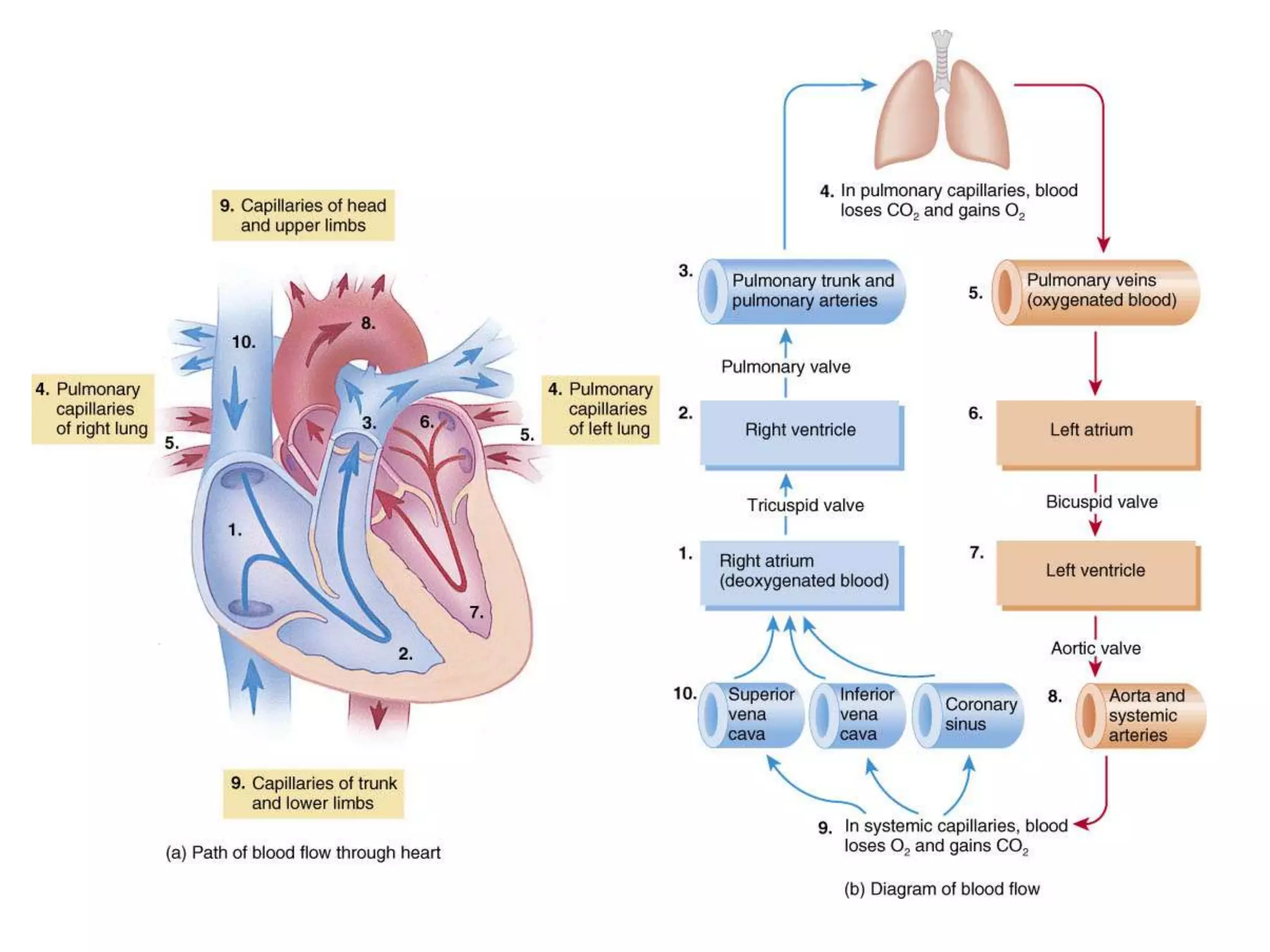
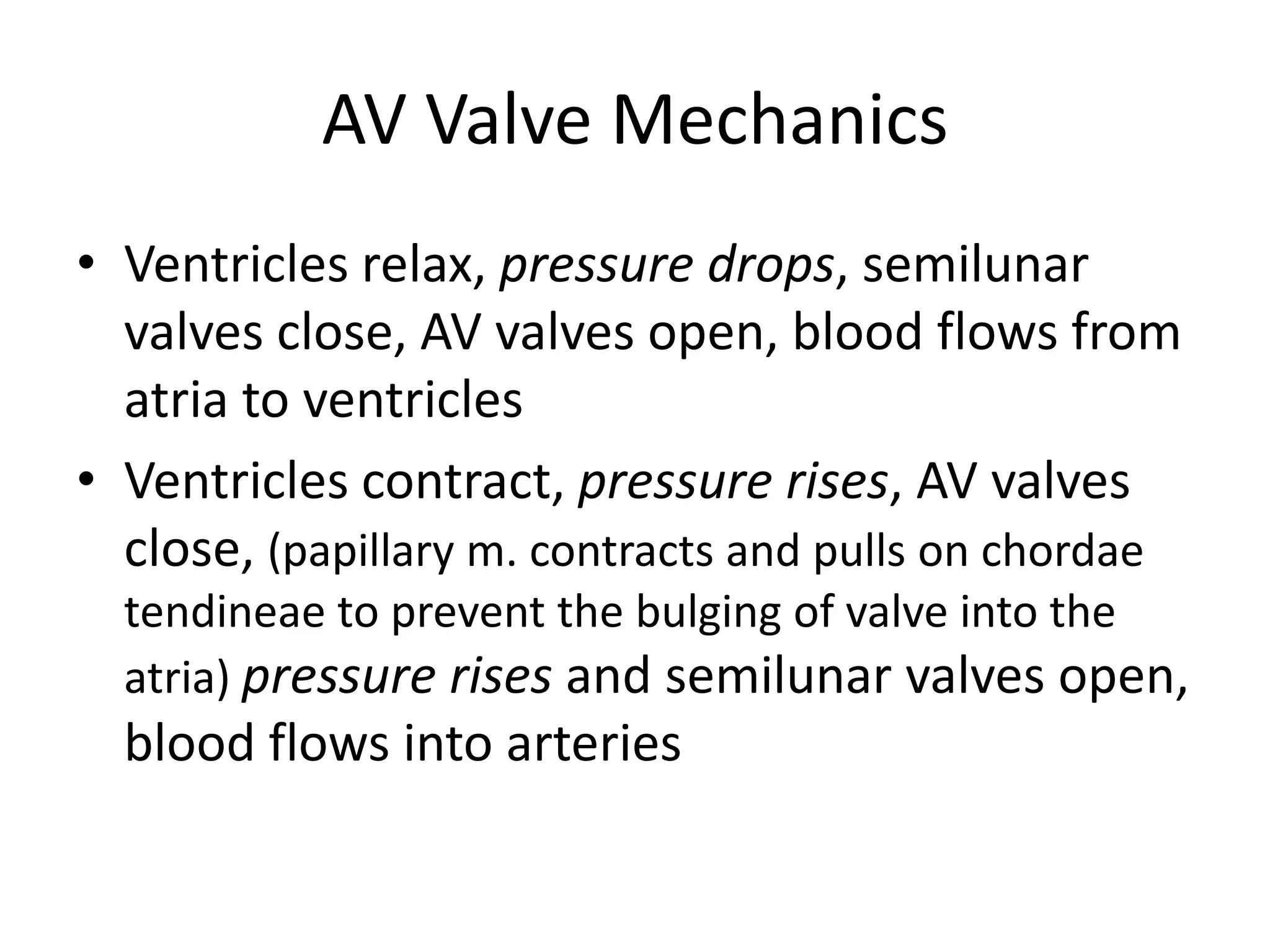
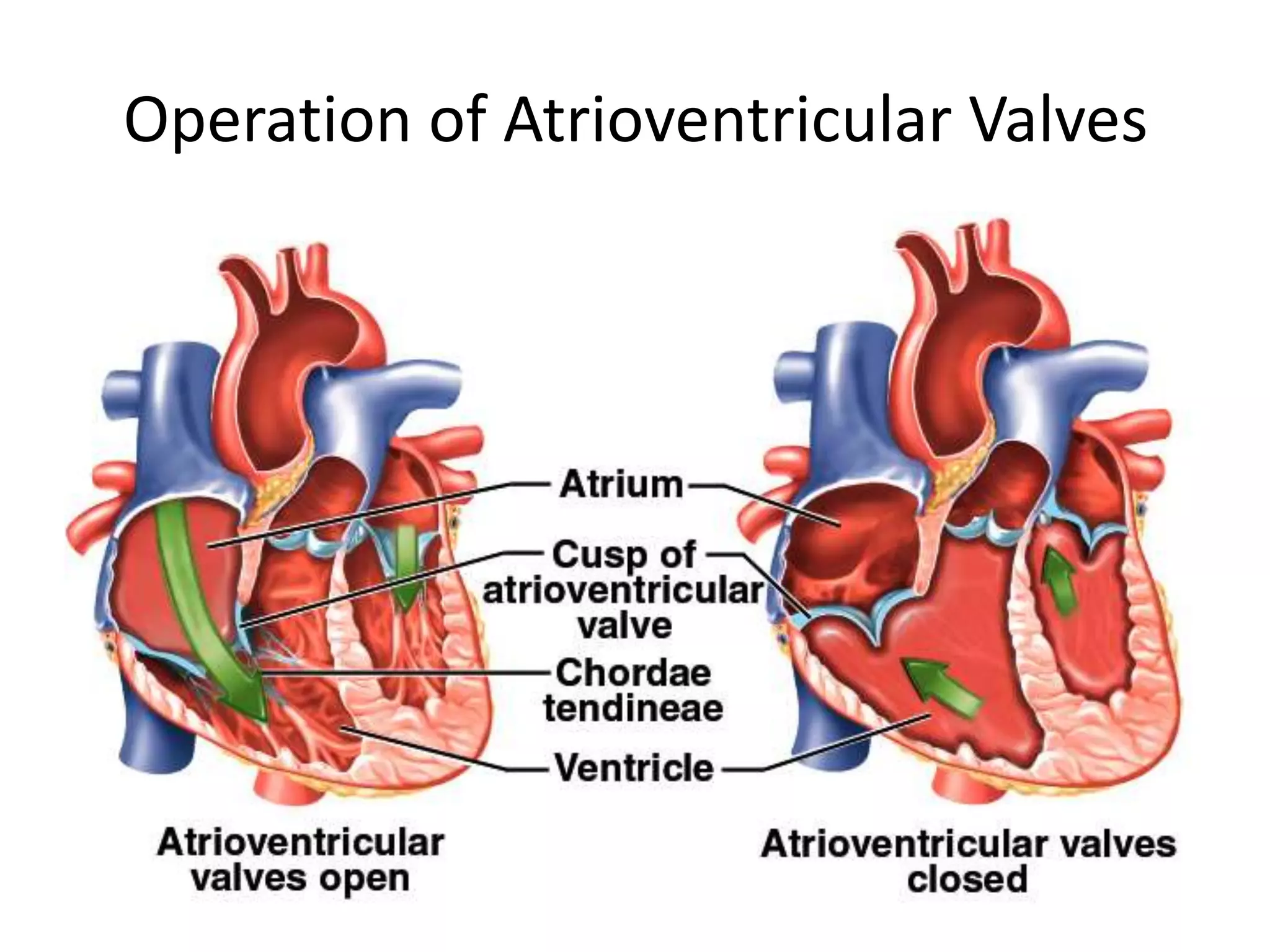
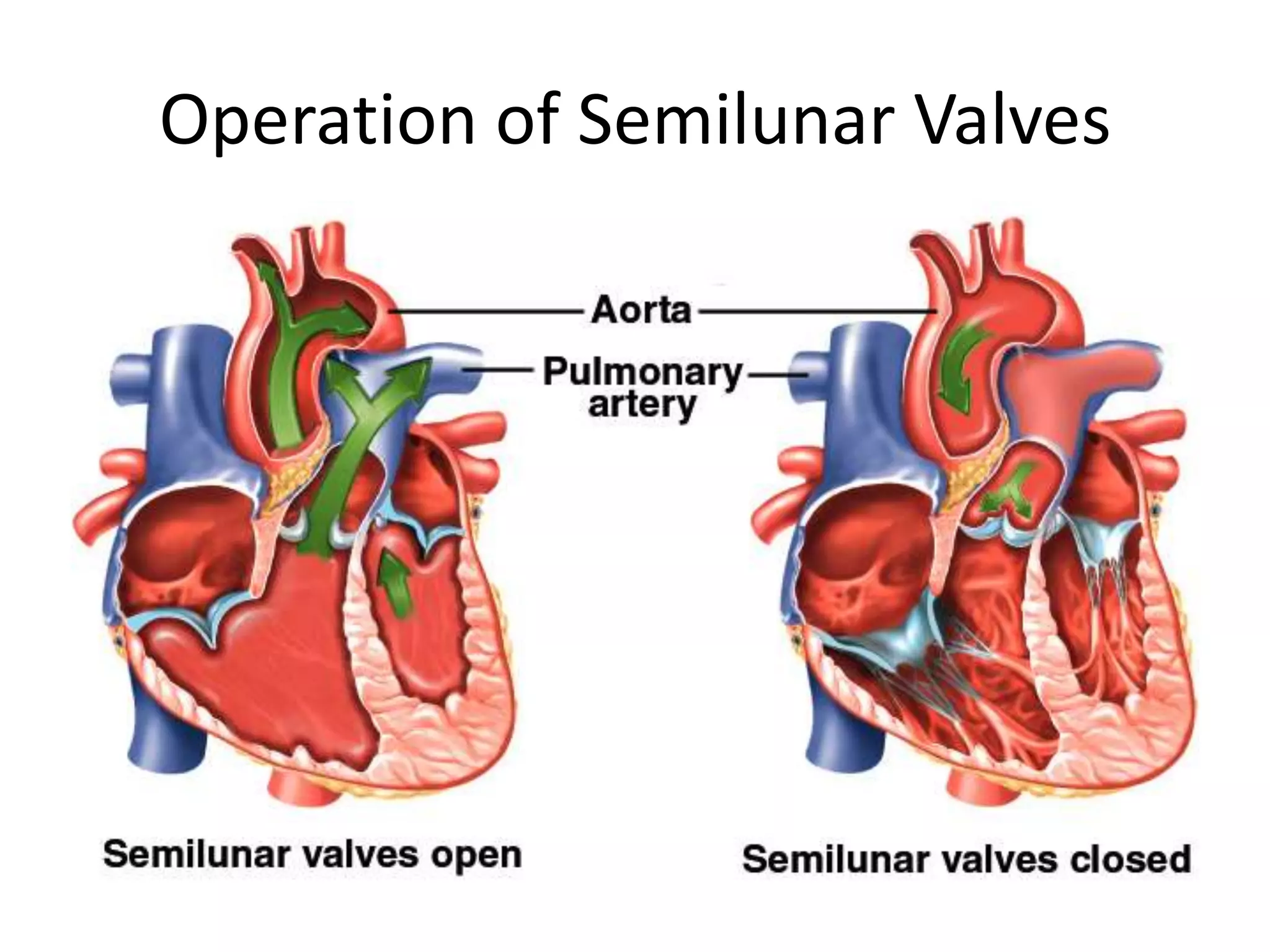
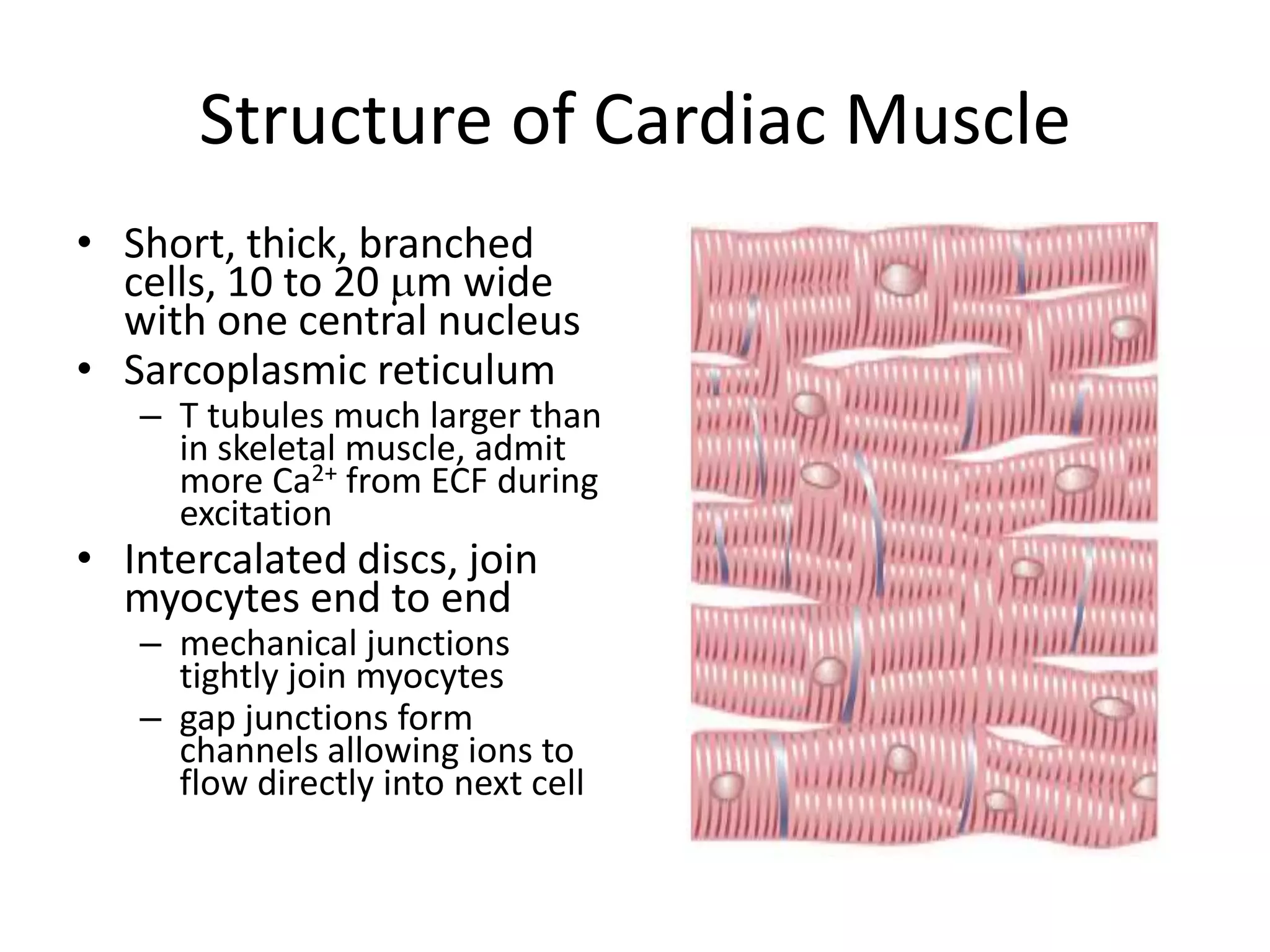
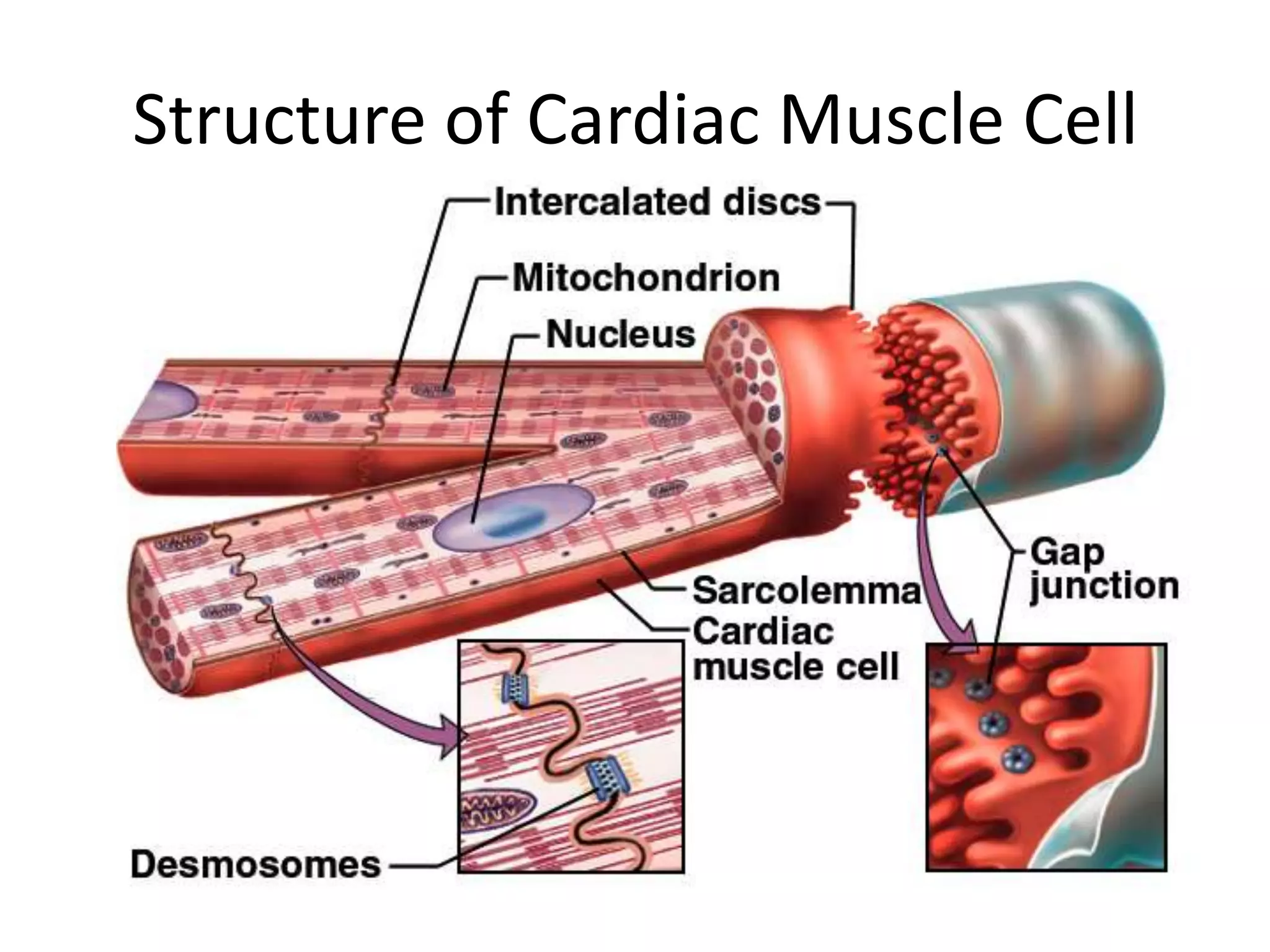
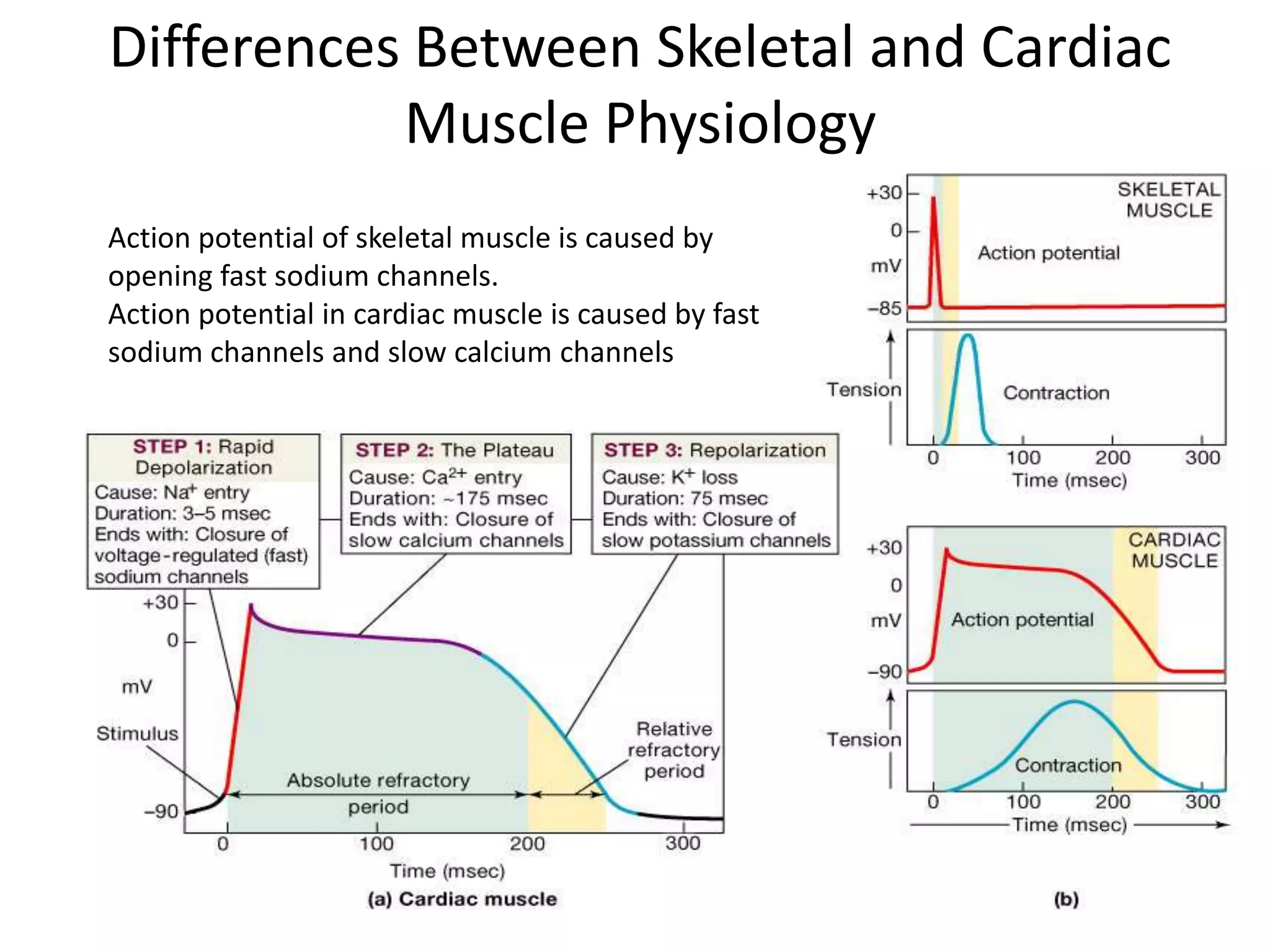
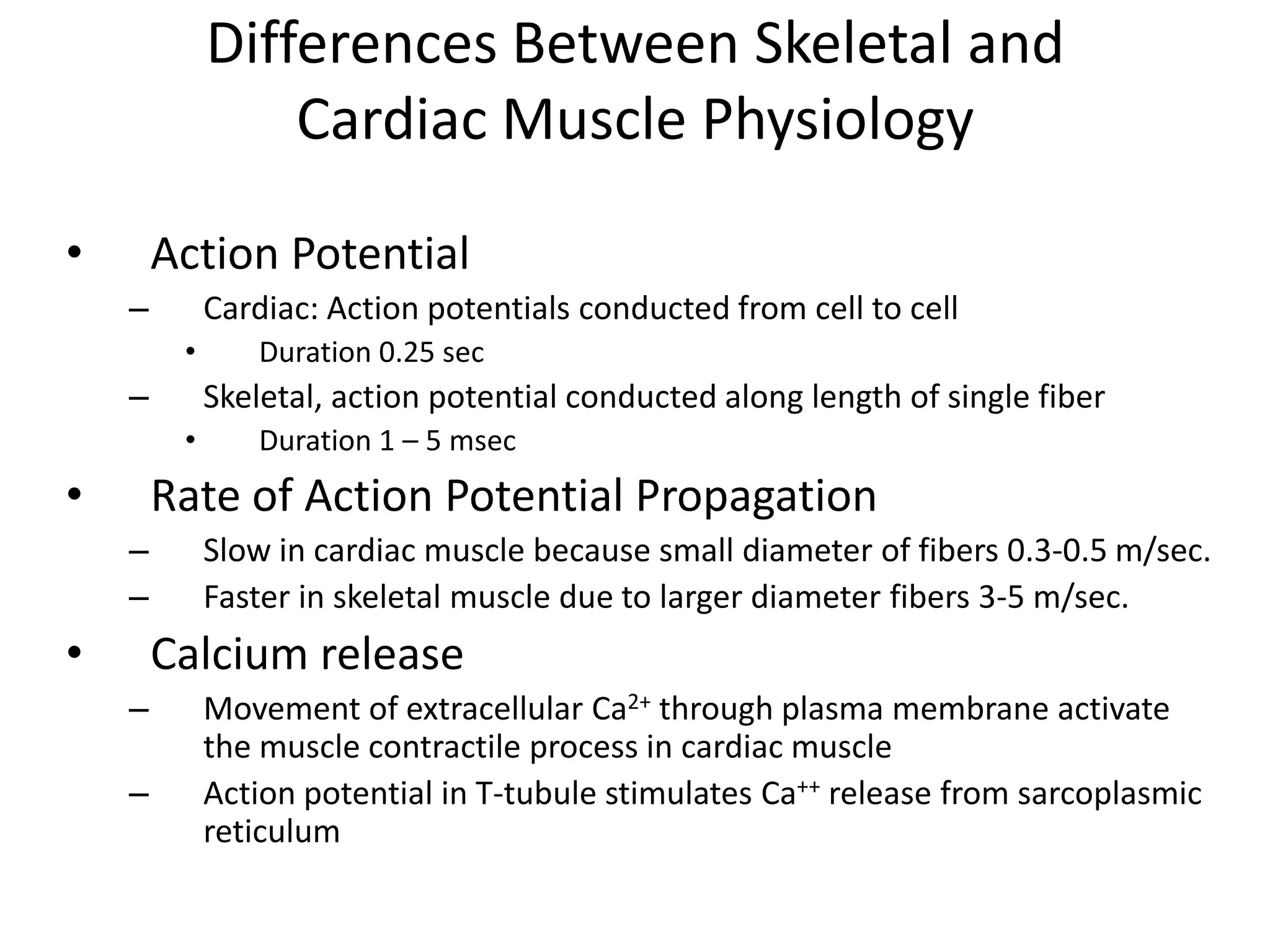
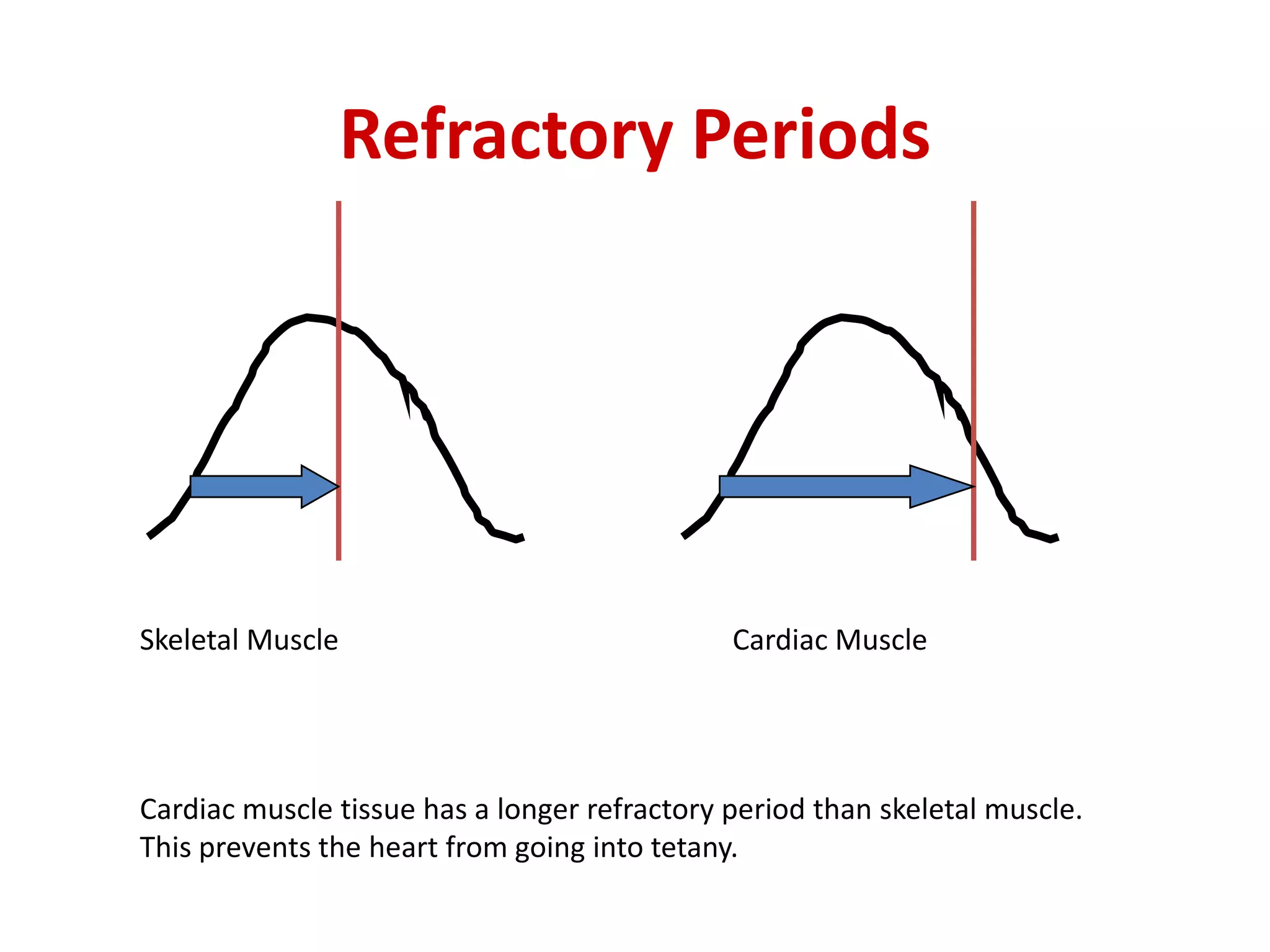
The heart has two pumps - the right heart pumps deoxygenated blood to the lungs and the left heart pumps oxygenated blood from the lungs to the rest of the body. Blood flows through the heart via the pulmonary and systemic circuits. The heart has four chambers separated by septa - the right and left atria receive blood returning to the heart while the right and left ventricles pump blood out of the heart. Heart valves prevent backflow of blood - atrioventricular valves between atria and ventricles and semilunar valves at the exits of the ventricles. Cardiac muscle has an extended action potential and refractory period compared to skeletal muscle to coordinate the pumping of the heart.