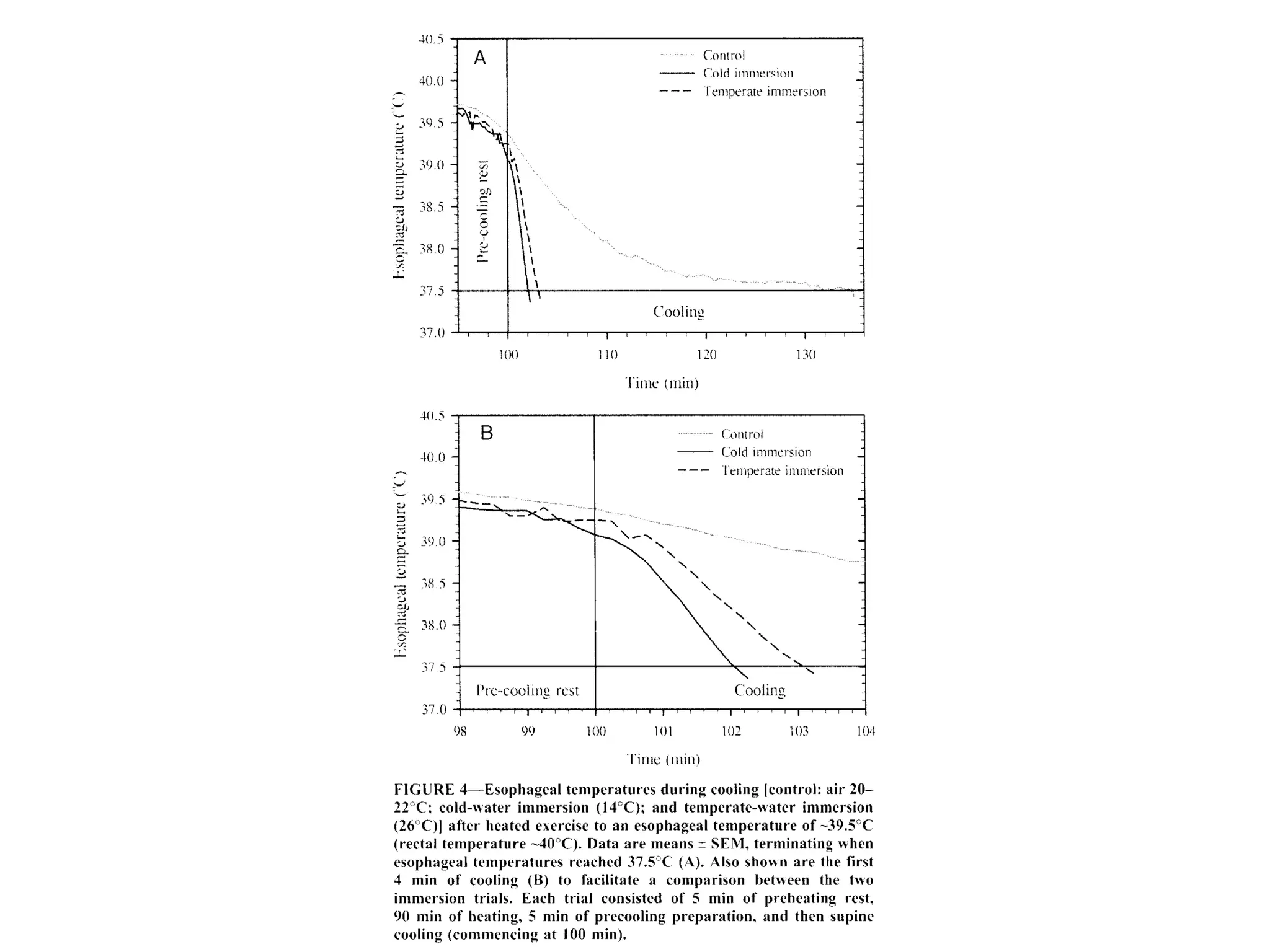
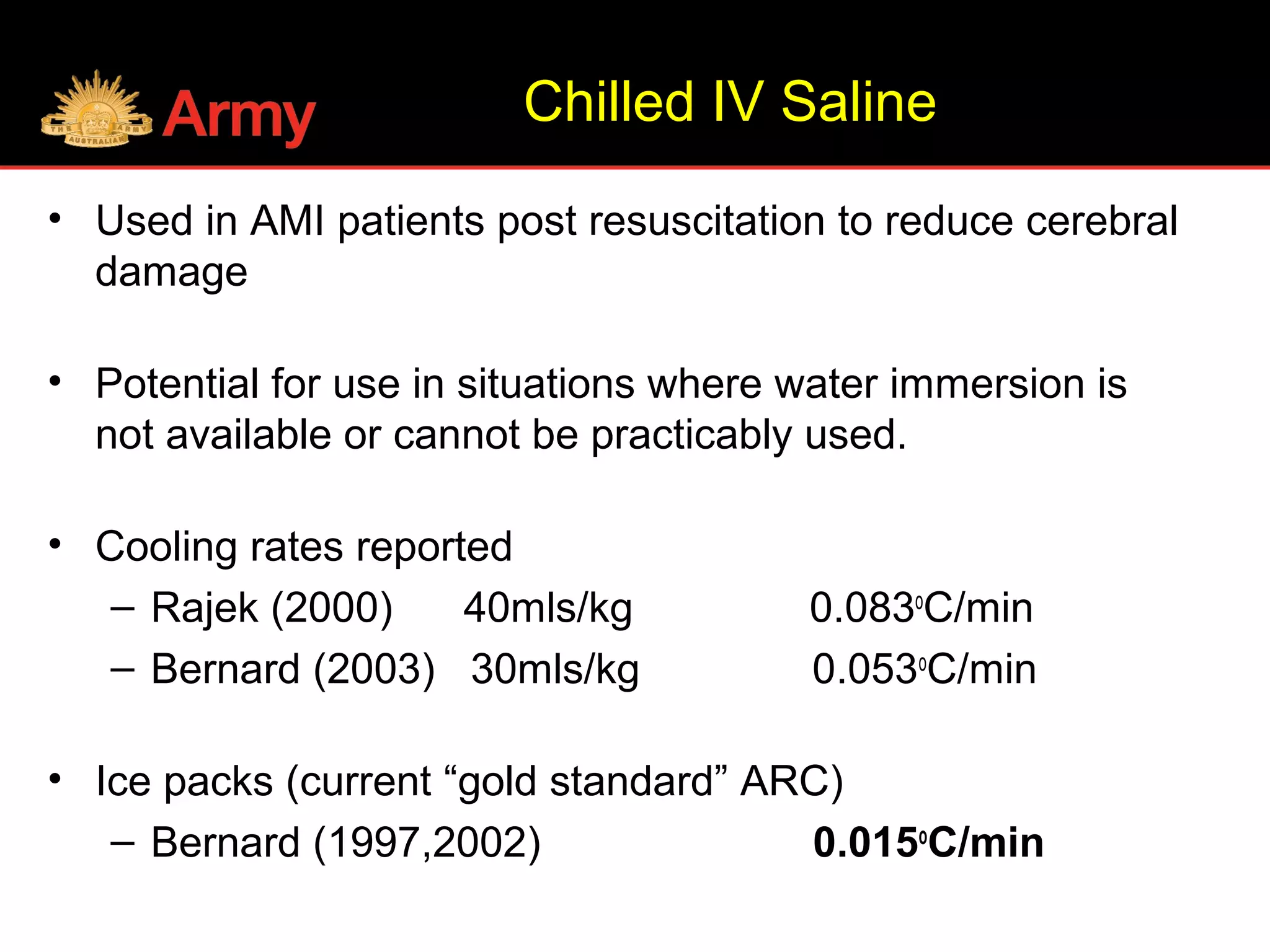
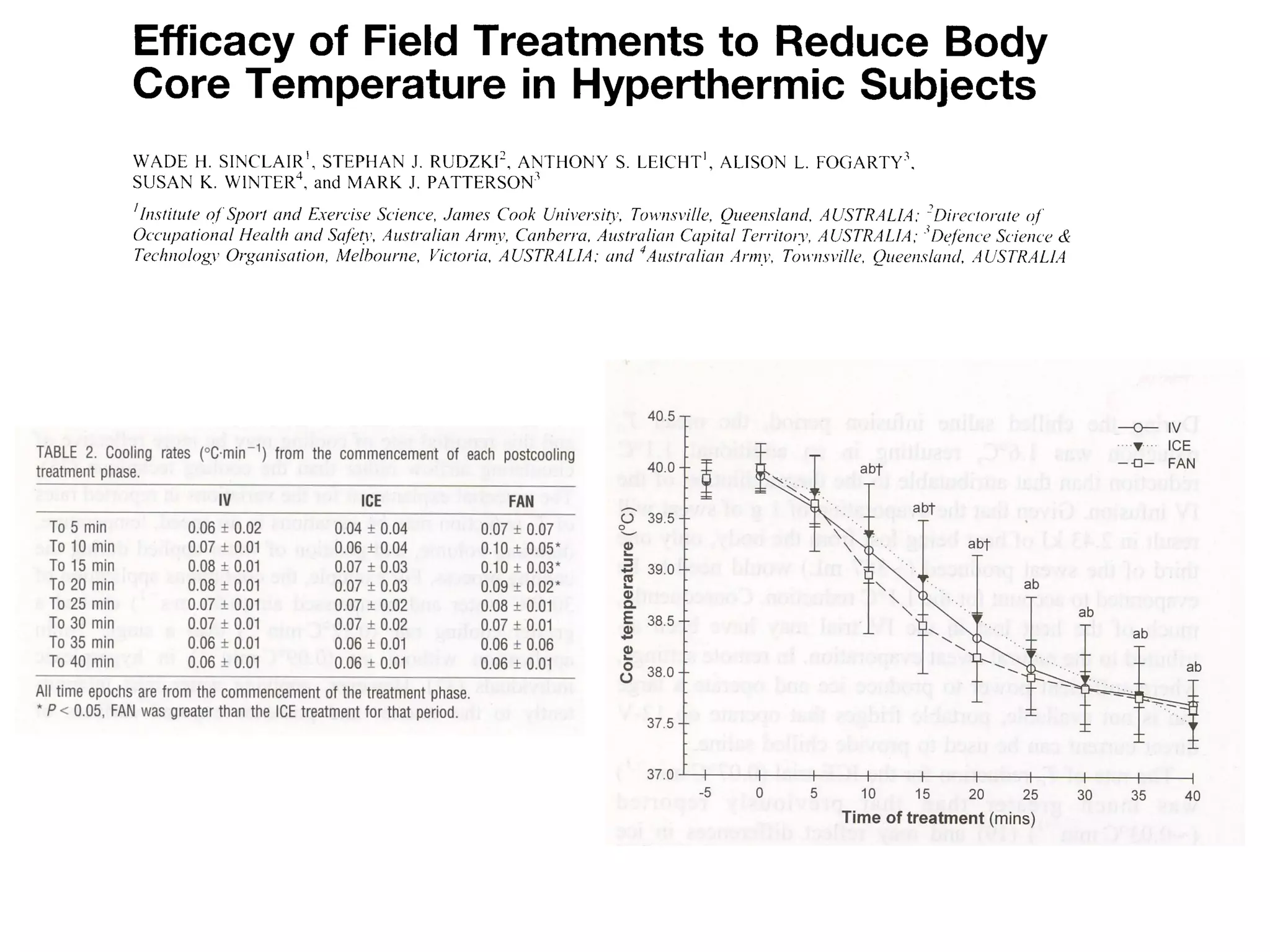
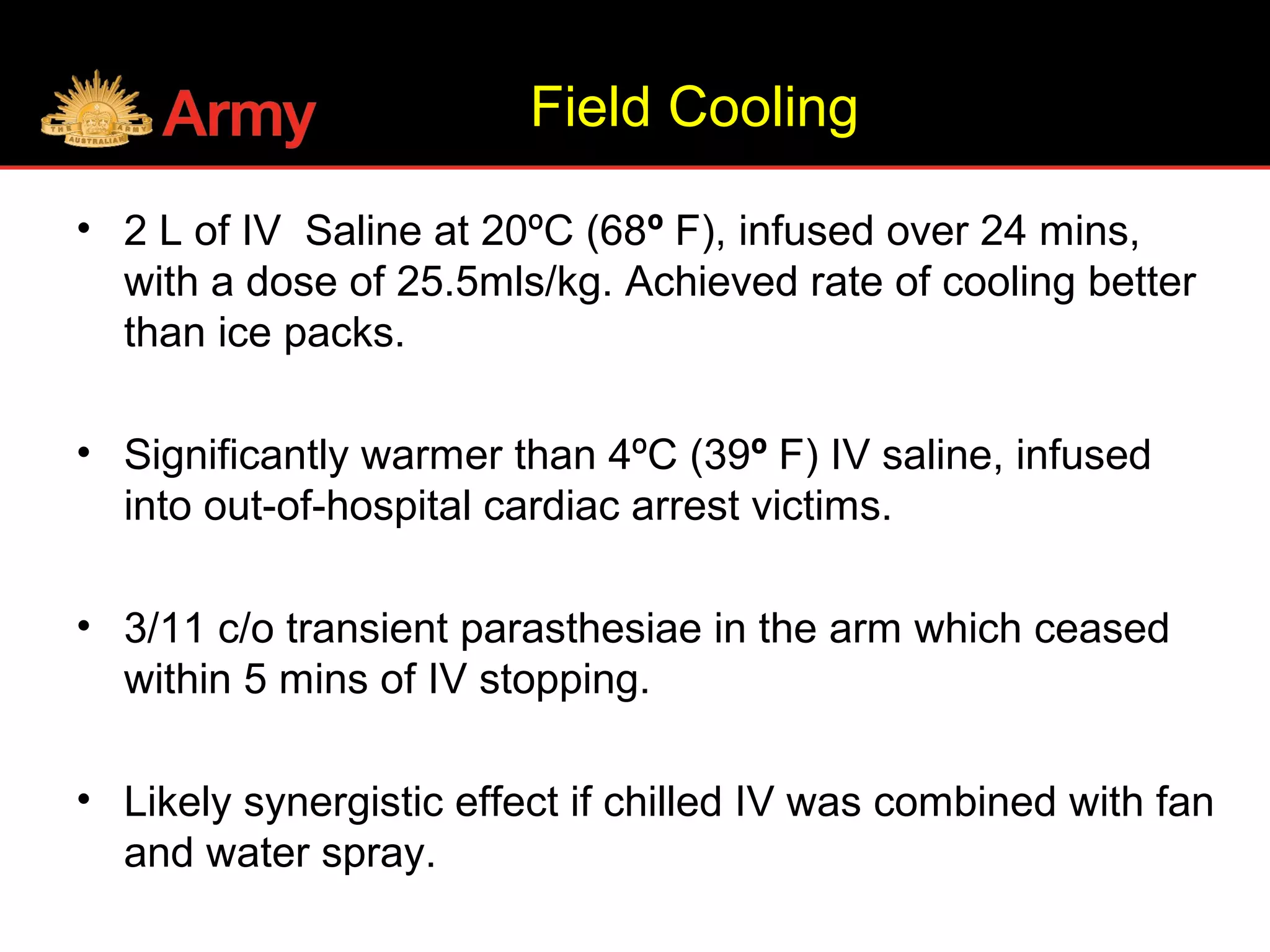
A soldier died of heatstroke during military training in the Northern Territory wet season. The early signs of heatstroke were not identified and ice packs were used to treat the soldier, which is an ineffective cooling method. The document identifies lessons around prevention, diagnosis, and treatment of heat injuries. It emphasizes that heatstroke is a medical emergency requiring rapid cooling through methods like cold water immersion or IV saline infusion, rather than slow methods like ice packs. The military has since improved heat injury education, policies, and management to prevent future deaths.
![Dehydration
• Humans are the only mammal to have salt in
their sweat.
• Thirst is driven by the concentration of
sodium [Na+
] in the plasma.
• Animals just lose water and increase their
plasma [Na+
] concentration. They then drink
to end their thirst, which occurs when their
[Na+
] concentration returns to normal.](https://image.slidesharecdn.com/ausheatstrokelessonslearnt-161108151058/75/Aus-heatstroke-lessons-learnt-10-2048.jpg)
![• Humans lose salt and water, so [Na+] can
change little, despite the loss of significant
fluid.
• The thirst reflex in humans does not kick in
until a person is 2-3% dehydrated.
• If you just drink WATER to thirst you will
always be around 2% dehydrated after
exercise.
Dehydration](https://image.slidesharecdn.com/ausheatstrokelessonslearnt-161108151058/75/Aus-heatstroke-lessons-learnt-11-2048.jpg)
![• Extra water you drink will not stay in the
plasma unless consumed with sufficient
salt [Na+].
• If you wish to avoid dehydration after
activity
You MUST replace your salt losses.
Dehydration](https://image.slidesharecdn.com/ausheatstrokelessonslearnt-161108151058/75/Aus-heatstroke-lessons-learnt-12-2048.jpg)