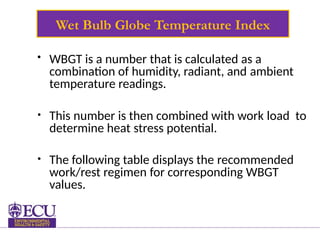
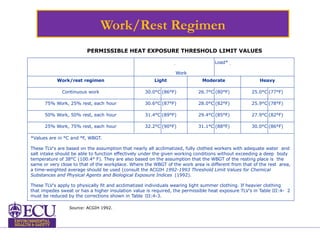
The document outlines the risks and symptoms associated with occupational heat stress, emphasizing factors such as environmental conditions and personal attributes that can exacerbate the issue. It details various heat disorders including heat exhaustion and heat stroke, along with prevention methods and treatment strategies for affected individuals. Monitoring heat stress through the Wet Bulb Globe Temperature Index (WBGT) is also discussed to ensure worker safety in hot environments.