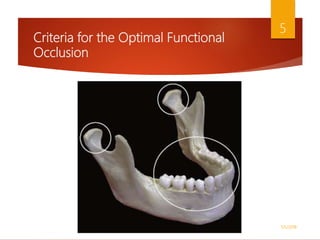
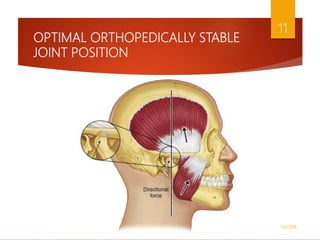
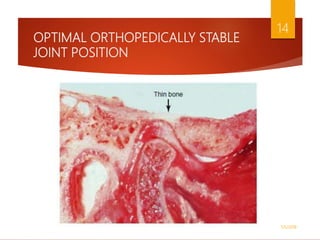
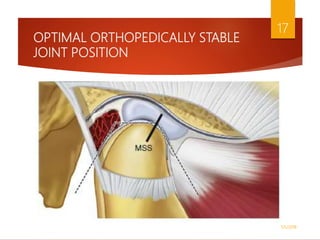
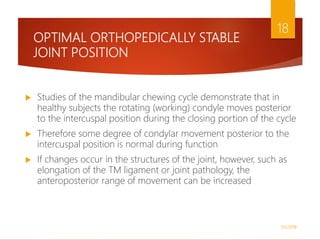
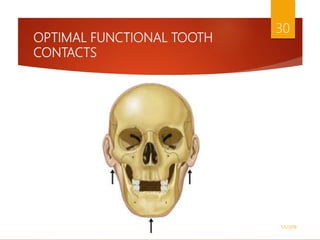
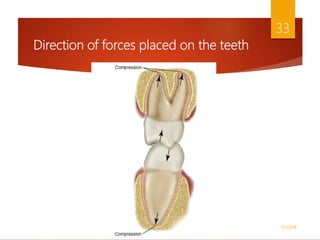
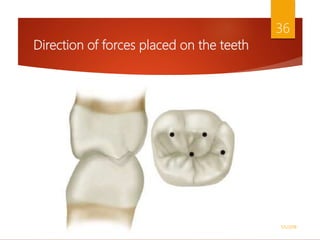
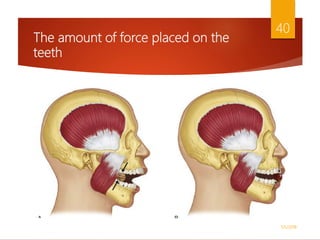
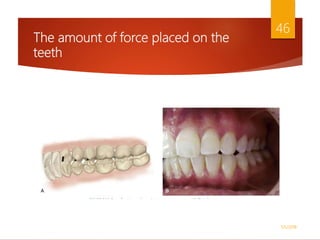
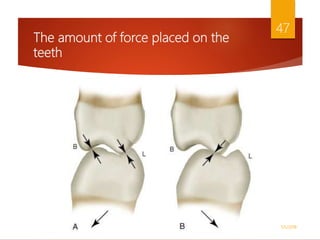
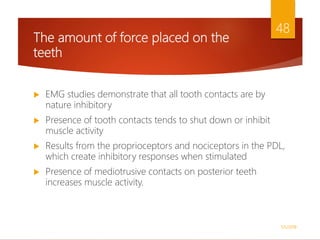
The document details the history and criteria for optimal functional occlusion in dentistry, highlighting key concepts such as balanced occlusion, dynamic individual occlusion, and centric relation. It emphasizes the importance of achieving a musculoskeletally stable joint position and effective tooth contacts during functional movements to minimize damage to the masticatory system. Optimal occlusal conditions should facilitate even and simultaneous contact of teeth when the condyles are in their most superoanterior position against the articular eminences.