This document discusses the development of quality standards for colposcopy education, training, and practice in Europe from 2010-2019. It summarizes discussions and consensus reached at several European Federation of Colposcopy (EFC) satellite meetings and congresses regarding:
1) The status of colposcopy education/training and how colposcopy is practiced across Europe.
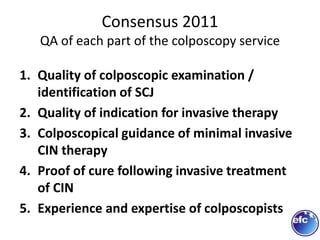
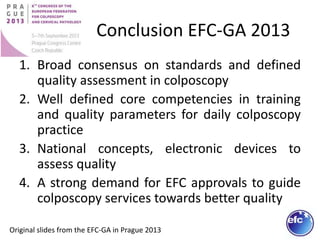
2) Developing European standards for colposcopy including minimum requirements for training programs, case loads for trainees/practitioners, and qualifications for trainers.
3) Reaching consensus on core competencies for colposcopy training and quality indicators for colposcopy services through repeated Delphi studies involving EFC member countries.