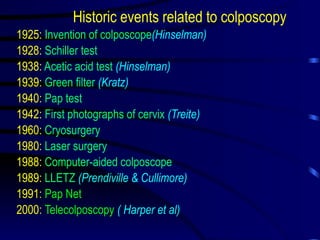
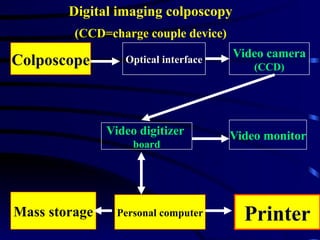
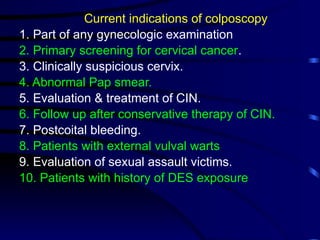
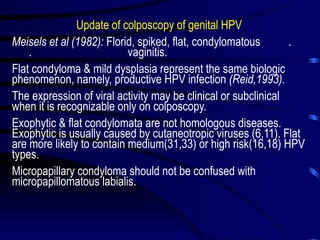
Colposcopy, established in gynecologic practice since 1925, is essential for examining cytologically detected lesions of the cervix, vagina, and vulva, with a growing global presence and training programs. Technological advancements have improved diagnostic capabilities, making colposcopy a preferred screening method for cervical cancer and other conditions. Future research aims to enhance computerized documentation and address the clinical significance of lesions related to HPV, while the demand for quality control and cost-effectiveness in patient care continues to rise.