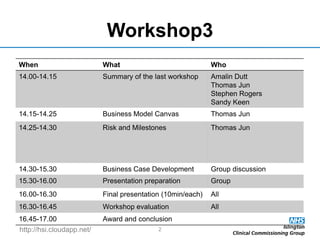
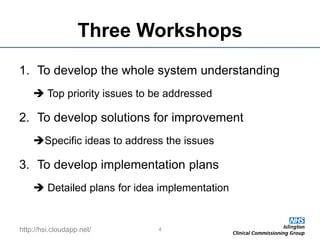
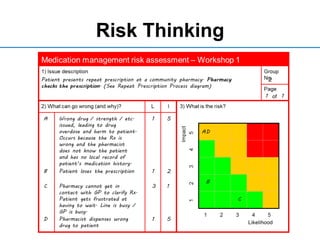
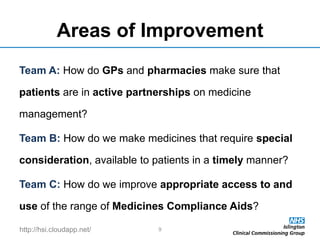
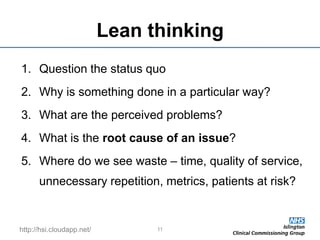
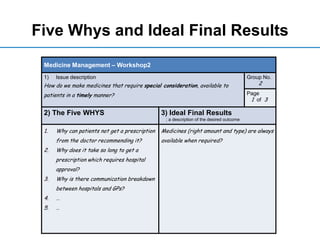
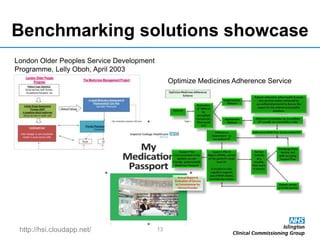
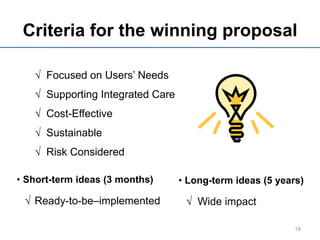
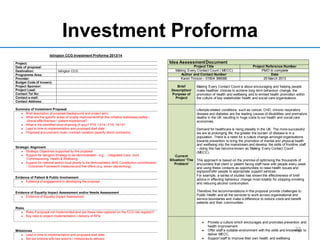
The document outlines an agenda for a workshop on safer medicine management among older people living at home. The workshop will include presentations on business model canvases, risk and milestones, and business case development. Attendees will work in groups to develop business cases for three proposals: using "teach back" to engage patients, improving inter-professional communication around specialized medications, and changing systems for medicine optimization. The workshop aims to create implementation plans to address safer medication management.