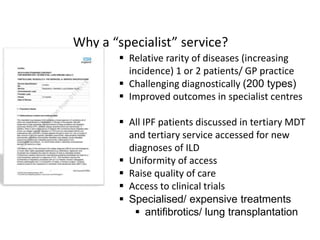
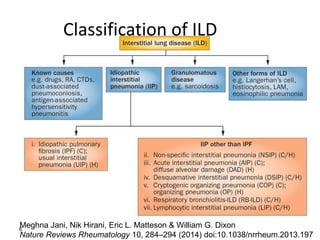
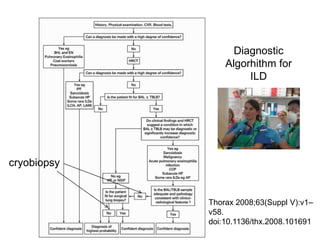
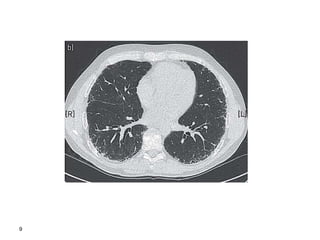
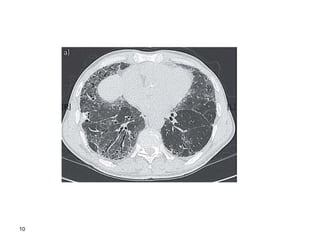
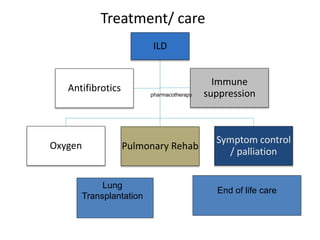
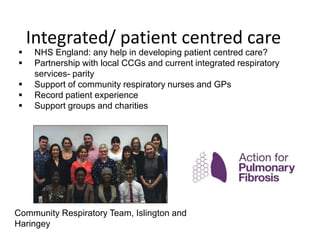
The presentation discusses the structure and importance of specialist Integrated Lung Disease (ILD) services, highlighting the rarity and diagnostic challenges of ILDs and the improved outcomes associated with specialist centers. It emphasizes the need for comprehensive care that includes pharmacological treatments, non-pharmacological interventions like pulmonary rehabilitation, and coordinated palliative care. The document also covers clinical trials and research efforts aimed at understanding and treating various forms of ILD, underscoring the necessity for integrated, patient-centered care models.