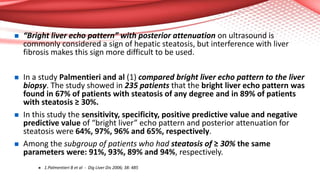
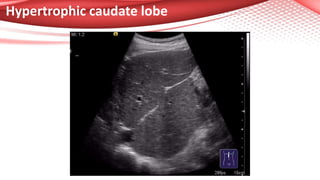
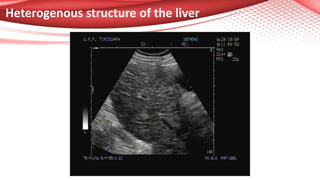
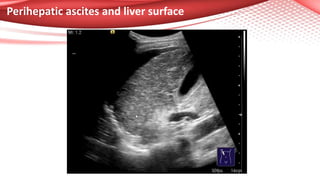
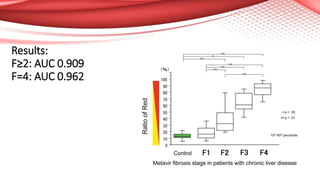
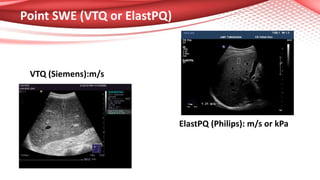
This document discusses the role of ultrasound in evaluating diffuse changes in the liver. It provides an overview of how ultrasound can detect and quantify steatosis by identifying a "bright liver" appearance with posterior attenuation. Studies have shown ultrasound has good sensitivity and specificity for detecting moderate or severe steatosis compared to liver biopsy. Ultrasound can also detect advanced liver fibrosis by identifying features like an irregular liver surface, signs of portal hypertension, and splenomegaly. Liver stiffness measurements using elastography techniques like transient elastography or shear wave elastography provide a quantitative assessment of fibrosis. However, ultrasound cannot differentiate non-alcoholic steatohepatitis from non-progressive non-alcoholic fatty liver