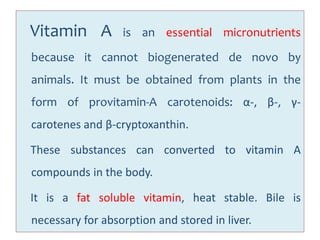
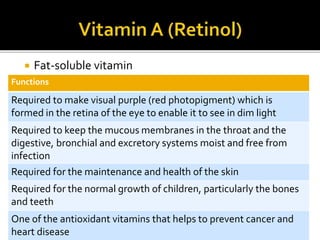
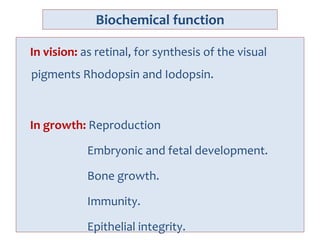
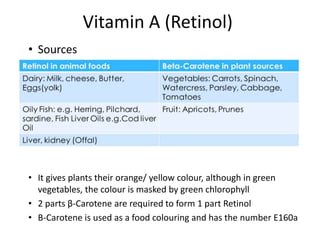
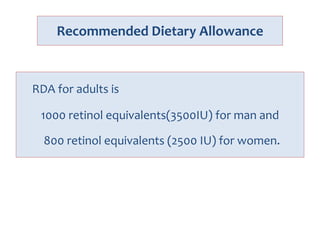
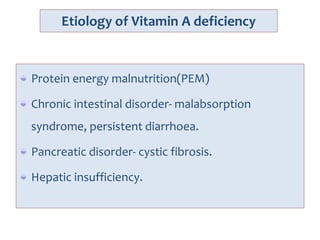
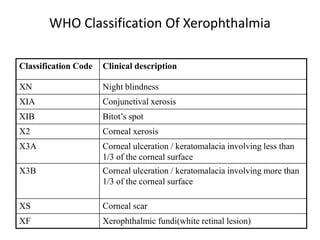
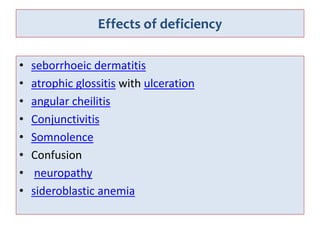
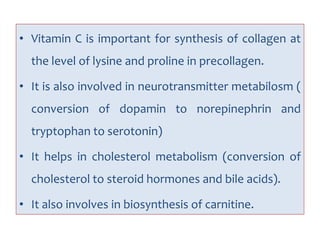
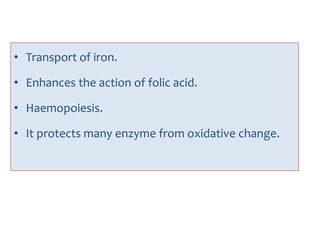
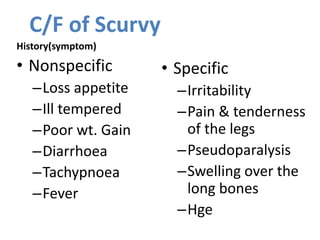
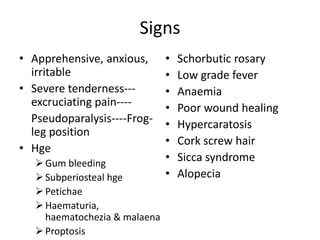
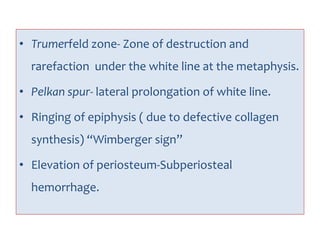
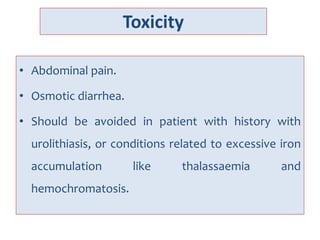
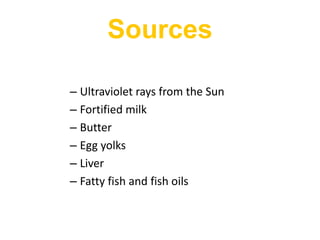
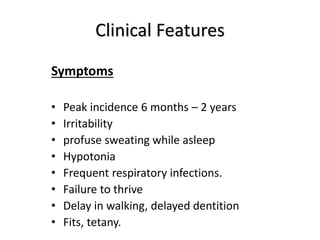
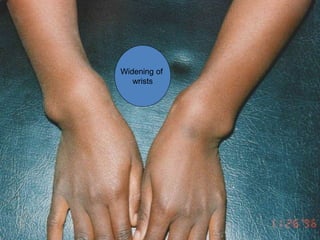
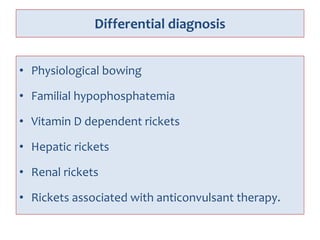
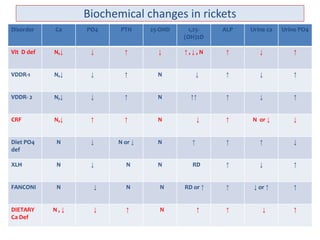
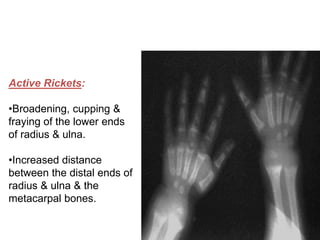
This document discusses vitamins and their roles and functions. It begins by defining a vitamin as an organic compound needed in small amounts for normal bodily processes that cannot be synthesized in the body. Vitamins are classified as either fat-soluble or water-soluble. The document then provides details on specific vitamins including Vitamin A, the B vitamins, Vitamin C, and Vitamin D. For each vitamin, the document outlines its biochemical functions, dietary sources, deficiency symptoms, recommended daily allowances, and other relevant information.