Vascular_Poster
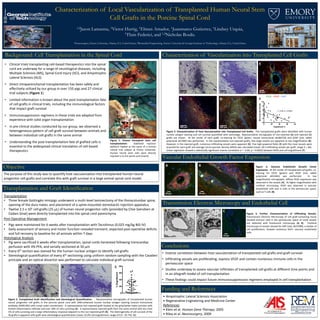
- 1. Characterization of Local Vascularization of Transplanted Human Neural Stem Cell Grafts in the Porcine Spinal Cord 1,2Jason Lamanna, 1Victor Hurtig, 1Elman Amador, 1Juanmarco Gutierrez, 1Lindsey Urquia, 1Thais Federici, and 1,2Nicholas Boulis. Background: Cell Transplantation in the Spinal Cord • Clinical trials transplanting cell-based therapeutics into the spinal cord are underway for a range of neurological diseases, including Multiple Sclerosis (MS), Spinal Cord Injury (SCI), and Amyotrophic Lateral Sclerosis (ALS) • Direct intraparenchymal transplantation has been safely and effectively utilized by our group in over 150 pigs and 27 clinical trial subjects (Figure 1) • Limited information is known about the post-transplantation fate of cell grafts in clinical trials, including the immunological factors that impact graft survival • Immunosuppression regimens in these trials are adapted from experience with solid organ transplantation • In pre-clinical studies conducted by our group, we observed a heterogeneous pattern of cell graft survival between animals and between individual cell grafts in the same animal • Understanding the post-transplantation fate of grafted cells is essential to the widespread clinical translation of cell-based therapeutics Objective The purpose of this study was to quantify host vascularization into transplanted human neural progenitor cell grafts and correlate this with graft survival in a large animal spinal cord model. Transplantation and Graft Identification Funding and References • Amyotrophic Lateral Sclerosis Association • Regenerative Engineering and Medicine Center References • Klein et al. Human Gene Therapy, 2005 • Riley et al. Neurosurgery, 2009 Vascular Endothelial Growth Factor Expression Conclusions Characterization of Vascularization into Transplanted Cell Grafts 1Neurosurgery, Emory University, Atlanta, GA, United States; 2Biomedical Engineering, Emory University & Georgia Institute of Technology, Atlanta, GA, United States Figure 1: Human intraspinal stem cell transplantation. Stabilized injection platform fixated to the spine of a human clinical trial subject at Emory University. Human neural stem cells were directly injected in to the spinal cord (insert). Transplantation • Three female Gottingën minipigs underwent a multi-level laminectomy of the thoracolumbar spine, opening of the dura mater, and placement of a spine-mounted stereotactic injection apparatus • Twelve 2.5 x 105 cell grafts (25 μL) of human neural progenitor cells (provided by Clive Svendsen at Cedars Sinai) were directly transplanted into the spinal cord parenchyma Post-Operative Management • Pigs were maintained for 6 weeks after transplantation with Tacrolimus (0.025 mg/kg BID IV) • Daily assessment of sensory and motor function revealed transient, expected post-operative deficits and full recovery to baseline for all animals within 7 days Histological Analysis • Pig were sacrificed 6 weeks after transplantation, spinal cords harvested following transcardiac perfusion with 4% PFA, and serially sectioned at 50 μm • Every 6th section was stained for the human nuclear antigen to identify cell grafts • Stereological quantification of every 6th sectioning using uniform random sampling with the Cavalieri principle and an optical dissector was performed to calculate individual graft survival 0 20 40 60 80 %Engraftment 200 μm 200 μm Figure 2. Transplanted Graft Identification and Stereological Quantification. Representative micrographs of transplanted human neural progenitor cell grafts in the porcine spinal cord with DAB-enhanced human nuclear antigen staining (mouse monoclonal antibody, MAB1281) with cresyl violet counterstain. A representative non-rejected graft located at the grey/white mater junction with limited inflammatory infiltrate and over 30% of cells surviving (A). A representative rejected graft from the same animal with less than 5% of cells surviving and a large inflammatory response adjacent to the non-rejected graft (B). The heterogeneity of cell survival of the 36 grafts is apparent with graft-wise stereological quantification (mean 22.0% cell engraftment, range of 0.0 - 65.7%) (C). A B C 200 μm 200 μm A B 0 20 40 60 80 0 2 4 6 8 10 Engraftment % MicrovascularDensity r = -0.60, p = 0.0002 D EC F Figure 3. Characterization of Host Vascularization into Transplanted Cell Grafts. The transplanted grafts were identified with human nuclear antigen staining and cell survival quantified with stereology. Representative micrographs of non-rejected (A) and rejected (C) grafts are shown. At the center of each graft, co-staining for CD31 (green, mouse monoclonal ab186720) and GFAP (red, rabbit polyclonal ab7260) was performed. In the representative non-rejected grafts, few large vessels are apparent at low magnification (B). However, in the rejected graft, numerous infiltrating vessels were apparent (D). Five high-powered fields (E) with the most vessels were acquired for each graft and average micro-vascular density (MVD) was calculated (mean 18.3 infiltrating vessels per graft, range 3 – 46). Linear regression showed a statistically significant inverse correlation (r = -0.60, p = 0.0002) between MVD and cell engraftment (F). CD31 - GFAP - DAPI • Inverse correlation between host vascularization of transplanted cell grafts and graft survival • Infiltrating vessels are proliferating, express VEGF and contain numerous immune cells in the perivascular space • Studies underway to assess vascular infiltrates of transplanted cell grafts at different time points and in an allograft model of cell transplantation • These findings could impact future immunosuppression regimens employed in cell transplantation Transmission Electron Microscopy and Endothelial Cell Proliferation BA Figure 4. Vascular Endothelial Growth Factor Expression. At the center of transplanted cell grafts, co- staining for CD31 (green) and VEGF (red, rabbit polyclonal ab53465) was performed. In low magnification micrographs, diffuse VEGF expression was observed in the vessels (A). At higher magnification with confocal microscopy, VEGF was observed in vascular endothelial cells and in cells in the perivascular space, such as T cells (B). Figure 5. Further Characterization of Infiltrating Vessels. Transmission Electron Microscopy of cell graft-containing tissue showed immune cells in the perivascular space of small vessels not detected with fluorescent microscopy (A, B). Confocal microscopy of vessels stained for Ki67 (red, ab15580), a marker of cell proliferation, showed numerous Ki67+ vascular endothelial cells. CBA