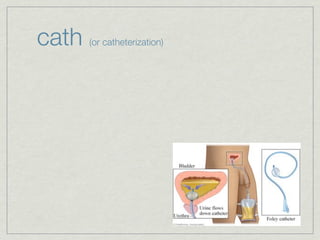
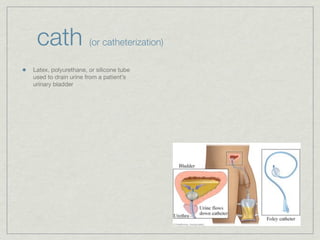
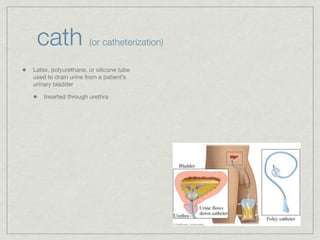
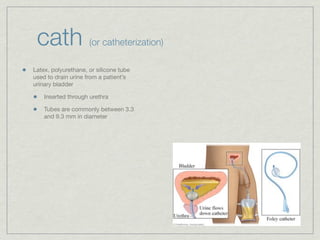
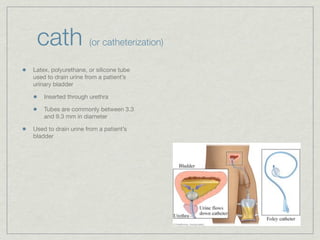
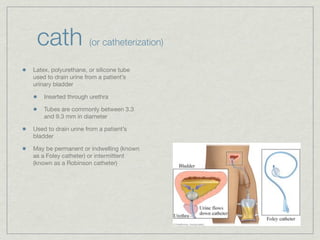
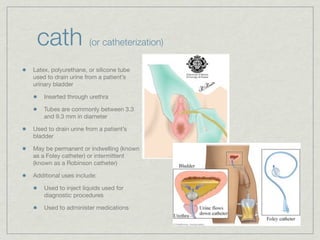
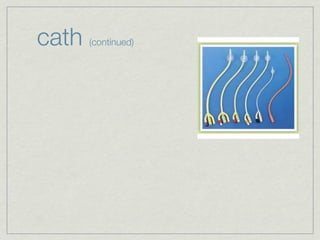
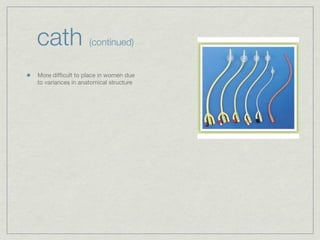
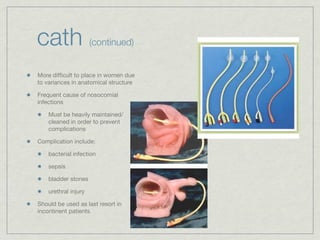
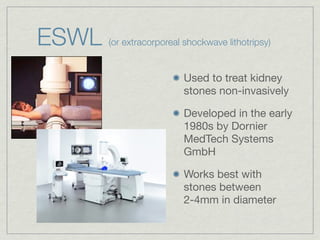
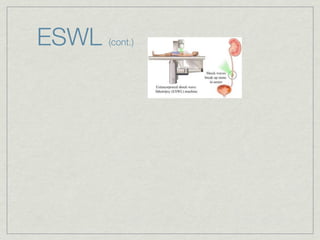
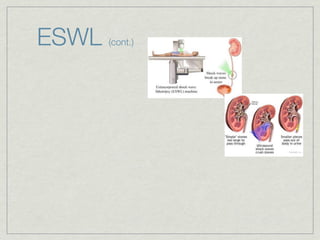
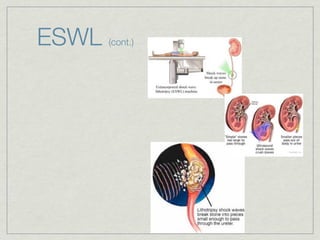
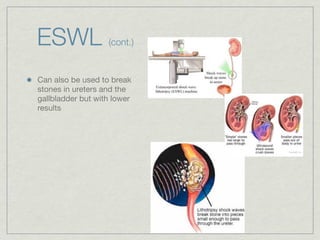
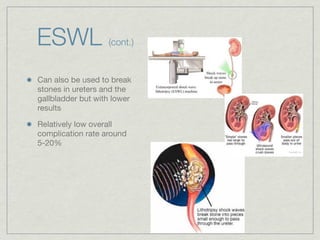
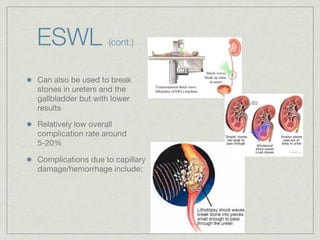
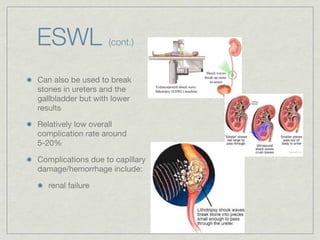
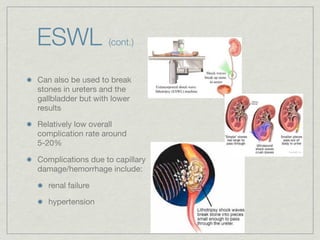
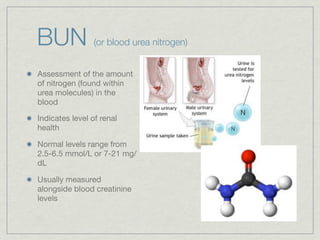
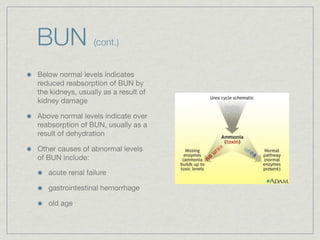
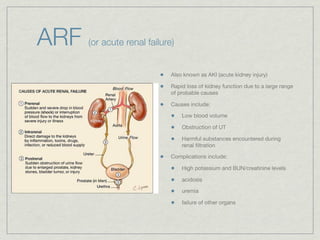
Cath is shorthand for catheterization, which is a latex, silicone, or polyurethane tube inserted through the urethra to drain urine from the bladder. Catheters can be permanent, indwelling devices or temporary and come in varying diameters. Complications include infection, sepsis, bladder stones, and injury. ESWL stands for extracorporeal shockwave lithotripsy, a noninvasive procedure developed in 1980s to treat kidney stones 2-4mm in size using shockwaves. Potential complications include renal failure and hypertension. BUN measures blood urea nitrogen to assess kidney function, with normal ranges being 7-21 mg/dL. Abnormal levels can indicate kidney damage or dehydr