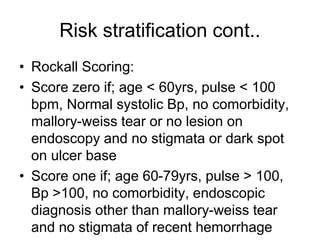
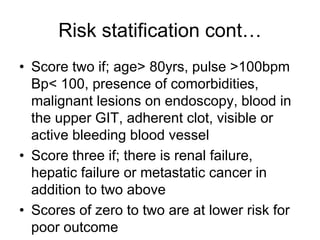
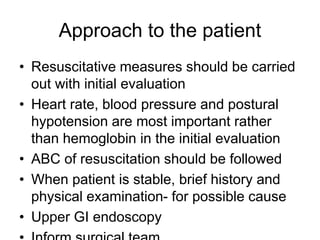
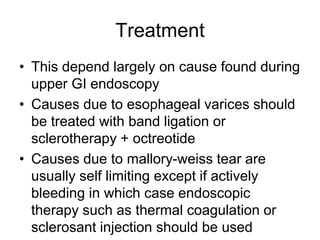
Upper gastrointestinal bleeding occurs proximal to the ligament of Treitz and may present as hematemesis, melena, or other symptoms. The annual incidence in the U.S. is 0.1% with a mortality rate of 5-10%, and risk factors are assessed using scoring systems like the Rockall score. Treatment varies significantly based on the specific cause identified during endoscopy, with options including endoscopic therapy, intravenous PPI, and management of underlying conditions.