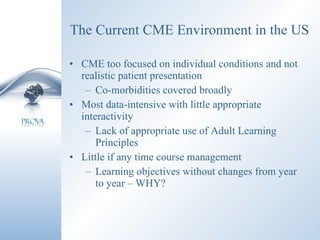
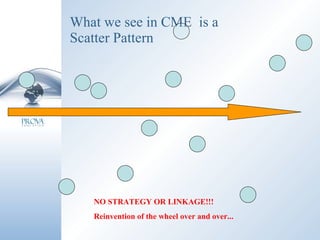
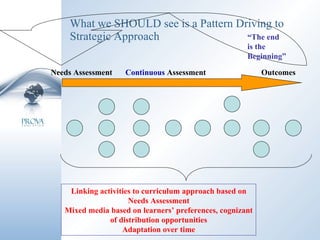
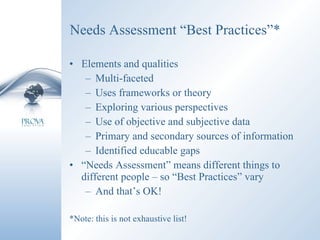
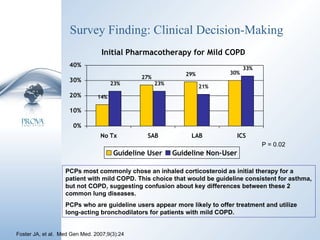
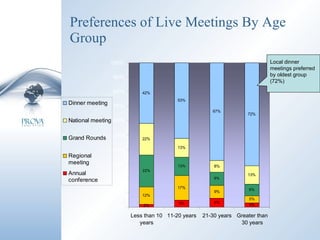
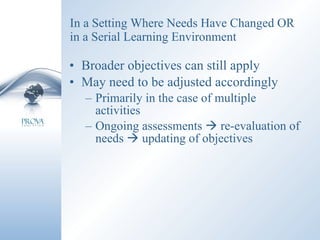
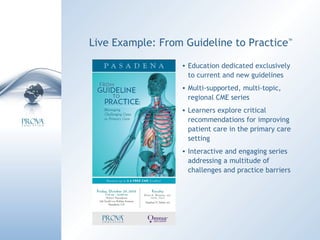
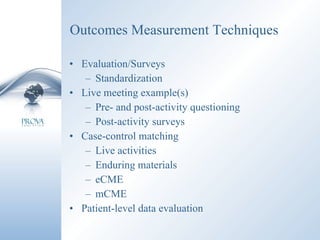
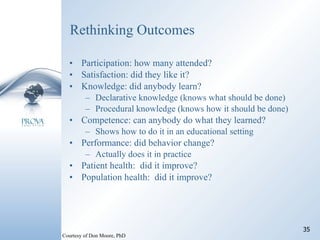
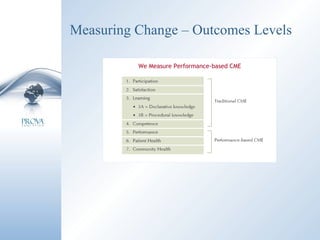
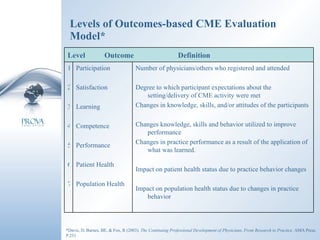
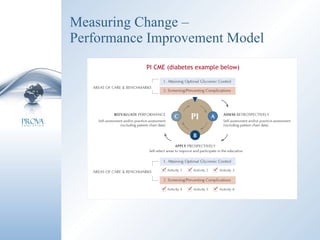
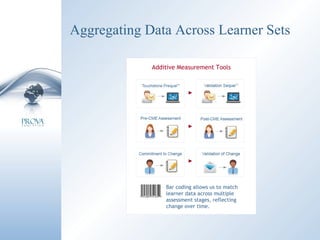
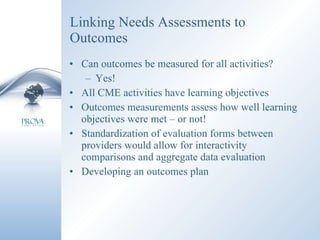
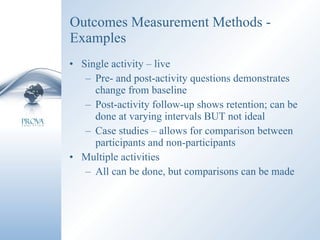
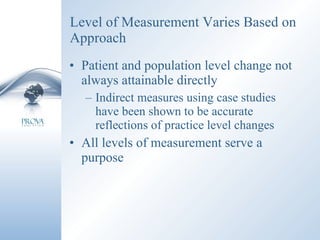
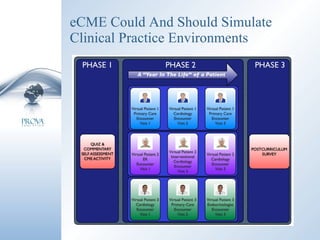
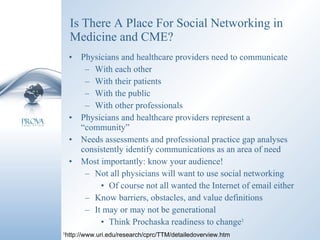
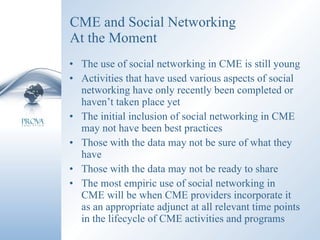
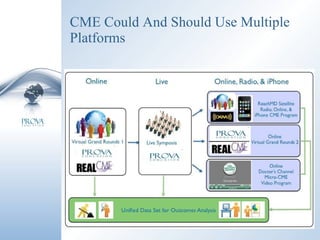
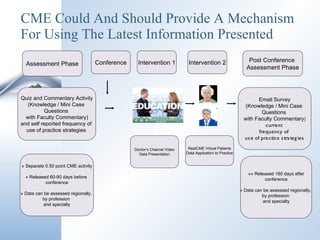
The document discusses optimizing continuing medical education (CME) and continuing professional development (CPD) worldwide. It addresses assessing learner needs, optimizing live CME/CPD activities, using technology in CME/CPD, and adopting a curricular approach. The discussion emphasizes conducting thorough needs assessments, enhancing the learning environment, measuring outcomes, and linking activities to objectives and assessments to drive strategic CME rather than isolated events.