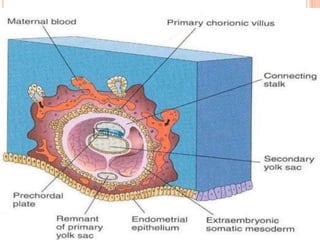
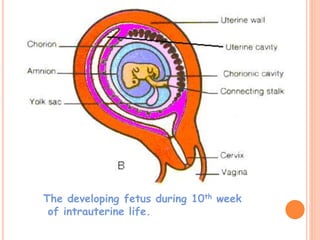
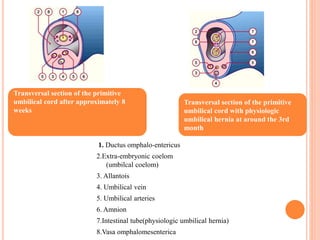
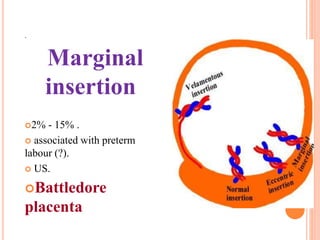
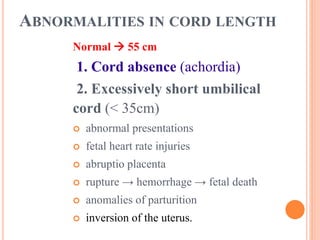
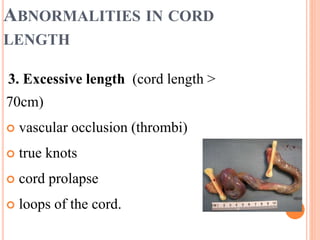
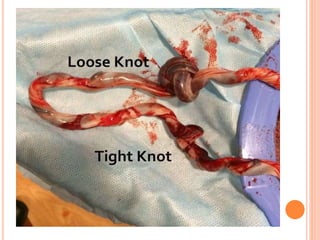
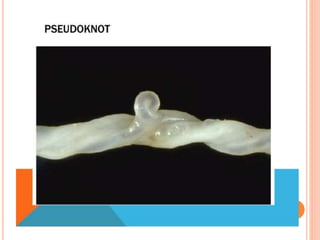
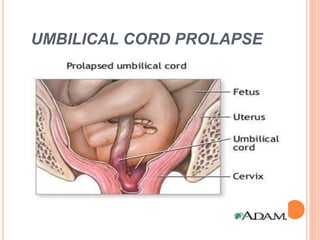
The umbilical cord develops between 4-8 weeks of gestation when the body stalk, ductus omphaloentericus, and umbilical coelom are enveloped by the amnion. As the fetus develops, the cord lengthens to allow for fetal movement while some structures like the ductus omphaloentericus and umbilical vesicle degrade. The normal cord is about 55cm long and contains two umbilical arteries and one vein. Abnormalities can include short or long cord, knots, velamentous insertion exposing blood vessels, and prolapse of the cord into the birth canal. Accidental issues like thrombosis, ruptures, or compression from loops or knots can also occur.