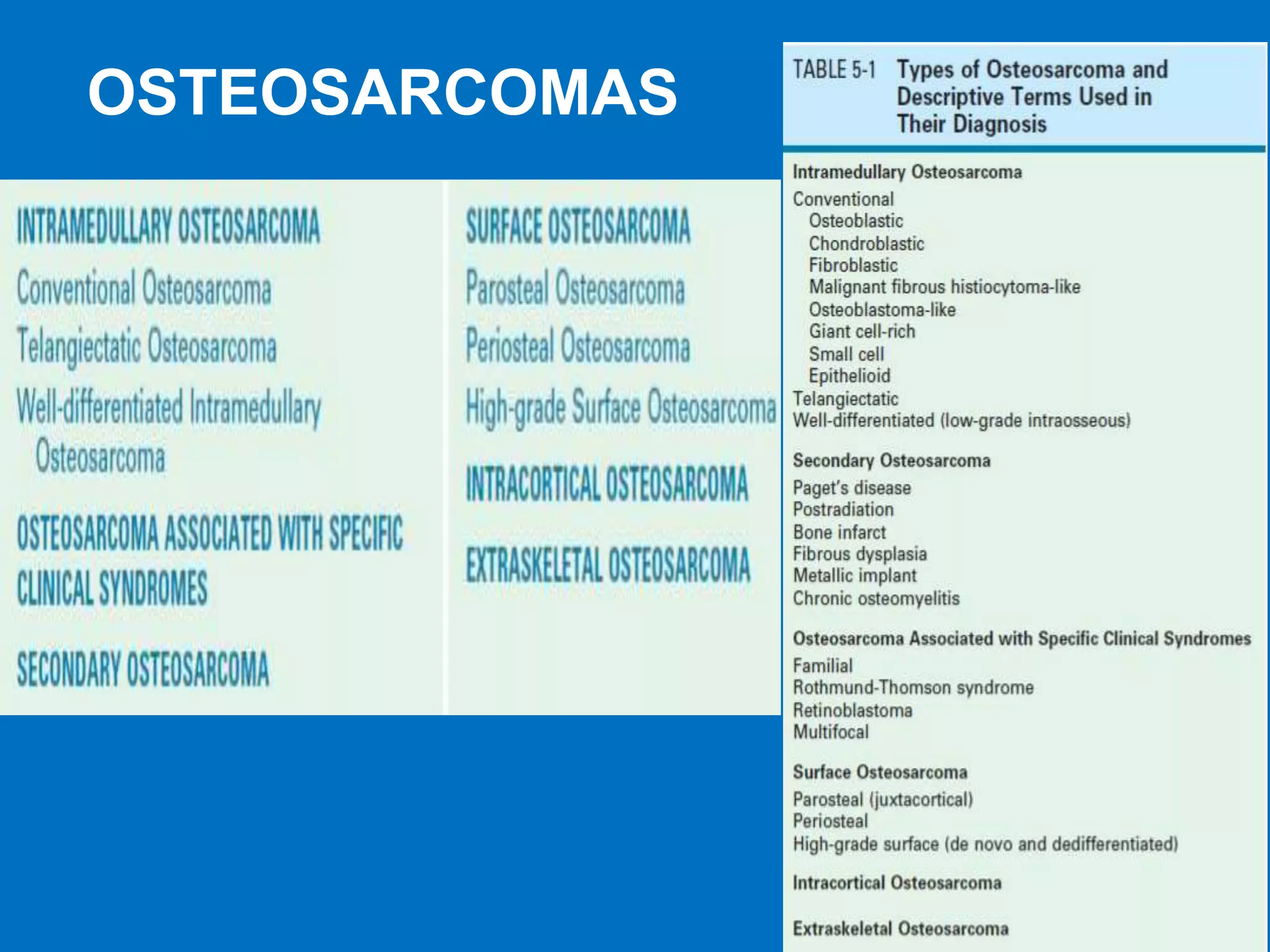
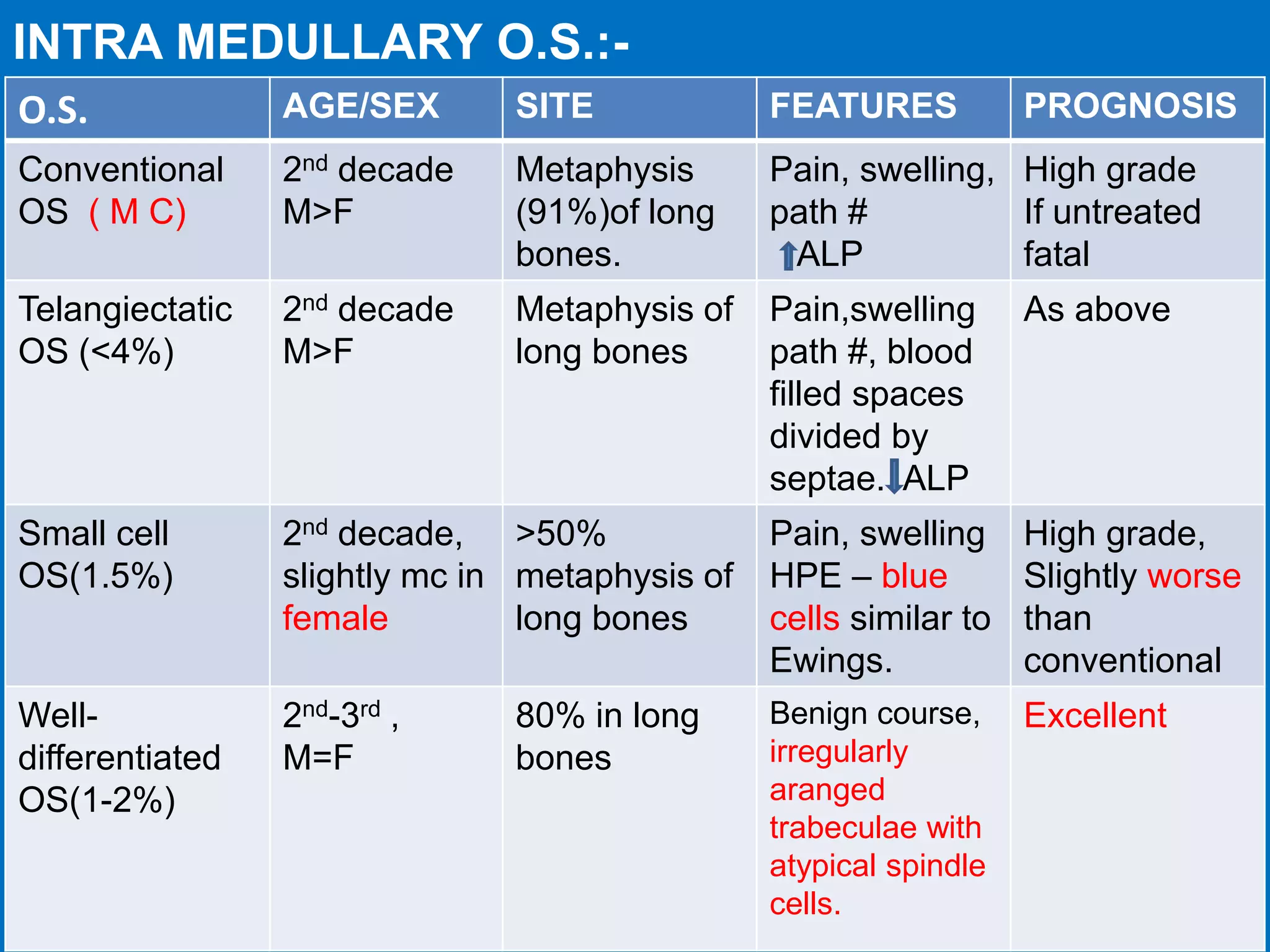
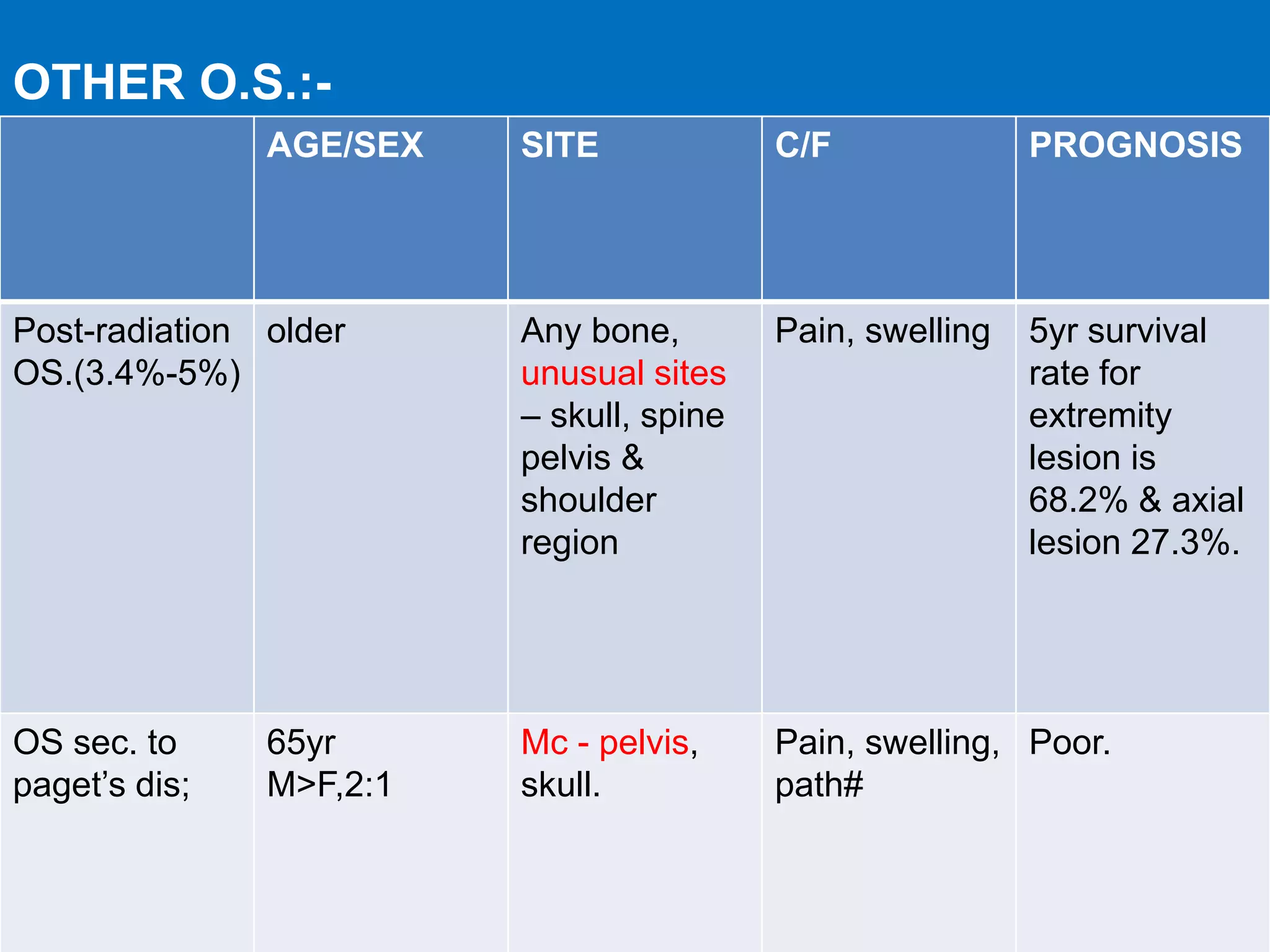
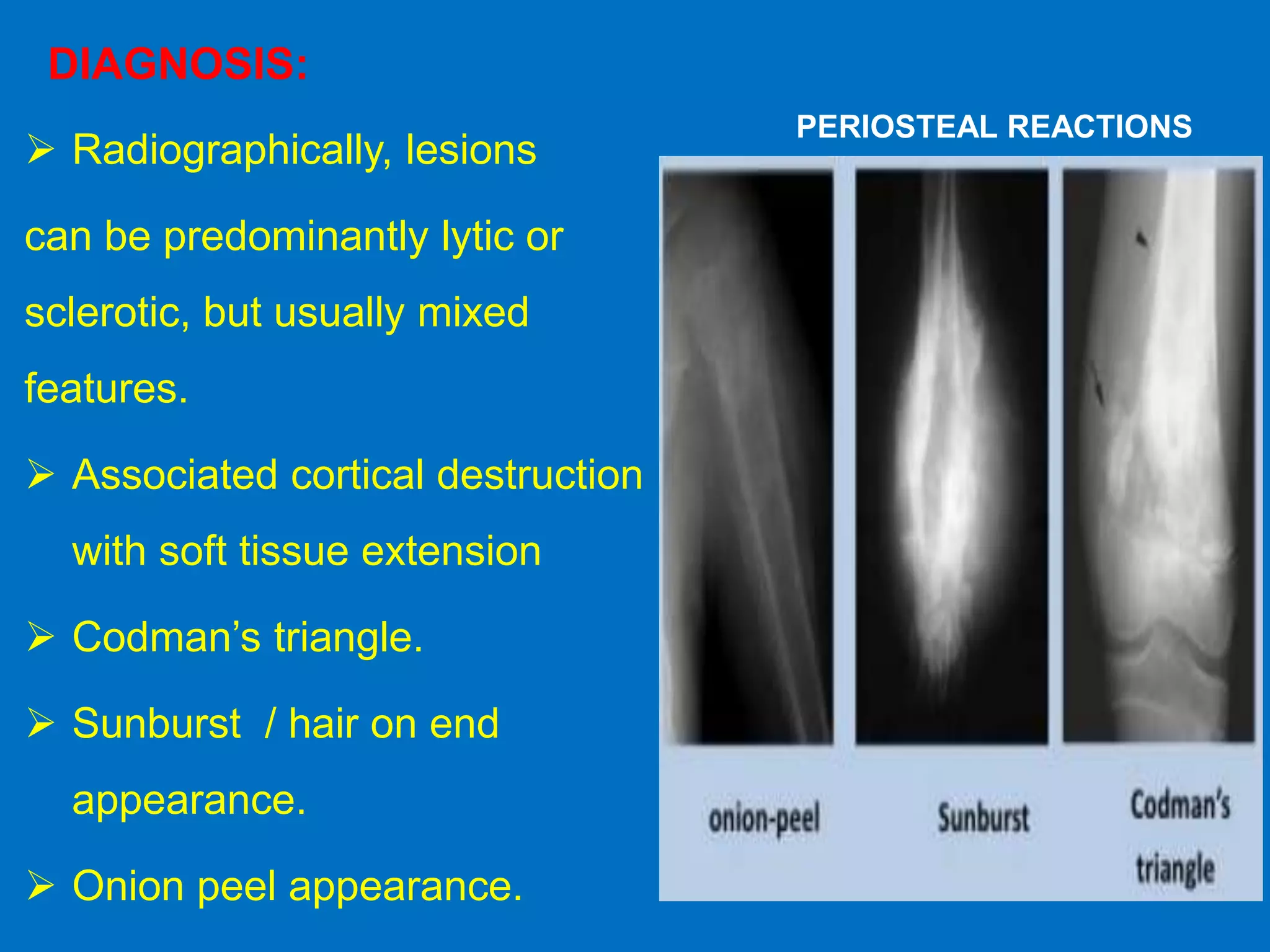
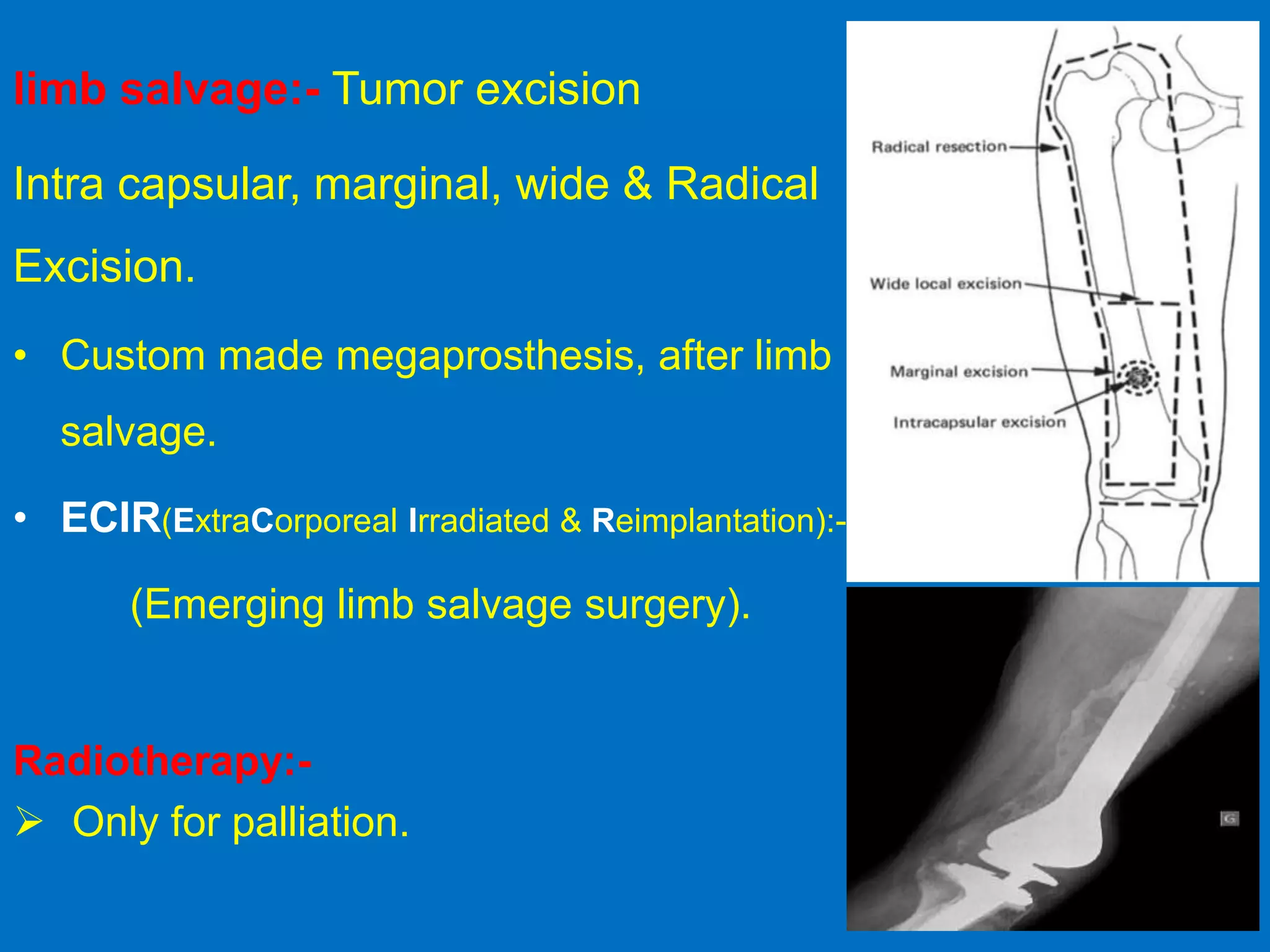
This document provides an overview of osseous bone tumors, including benign and malignant types. It discusses key benign tumors like osteoid osteoma, osteoblastoma, and bone islands. It also covers osteosarcoma in depth, describing its various subtypes, characteristics, diagnosis involving imaging and biopsy, Enneking staging system, and treatment approaches including chemotherapy, surgery, and prognosis factors. The summary focuses on key details about classification and management of important osseous bone tumors.


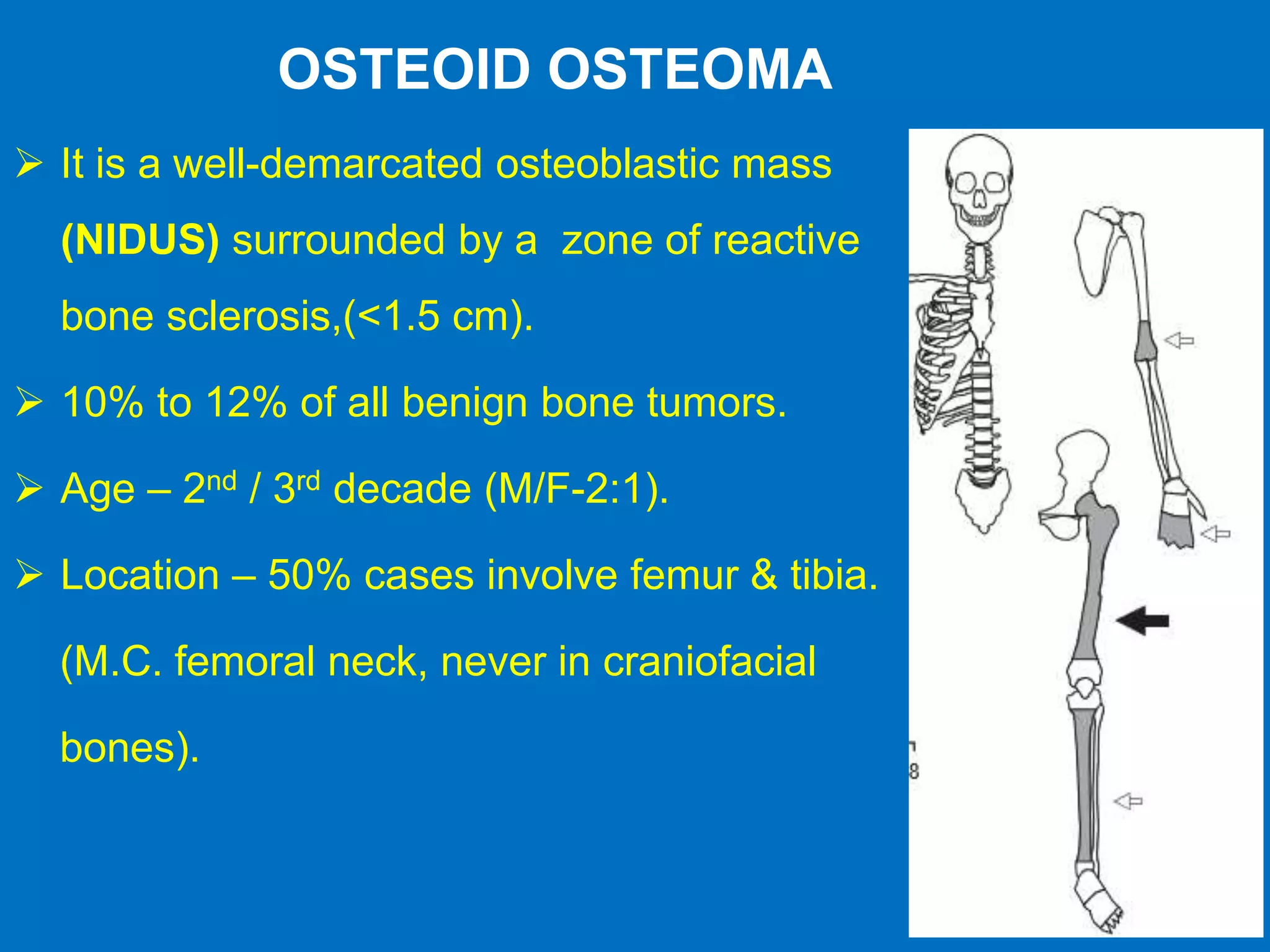


![ Age: 5-45 yrs (2nd & 3rd decade).
M:F is 2:1.
Incidence : <1% of all primary bone tumor.
M.C location -Axial skeleton(>40%).
2nd M.C - jaw bone craniofacial bones
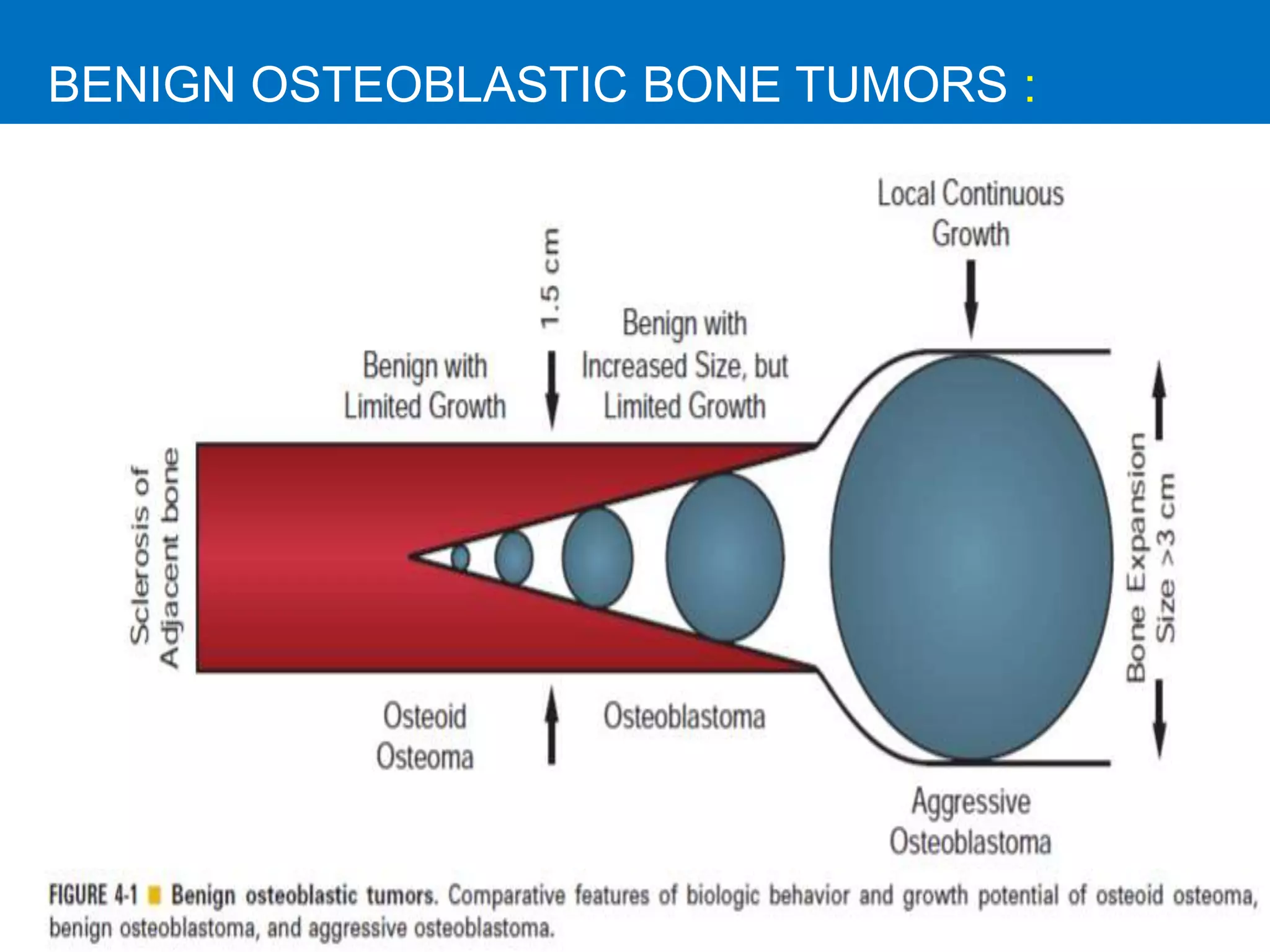
Osteoblastomas:-
1. Benign osteoblastomas(1.5-4cm),
2. Aggressive osteoblastomas(>4cm).
[CEMENTOBLASTOMA]](https://image.slidesharecdn.com/tumorsofosseousoriginmeera-180325130459/75/Tumors-of-osseous-origin-11-2048.jpg)