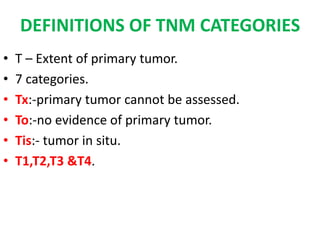
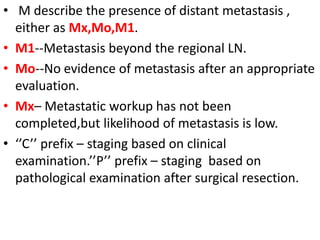
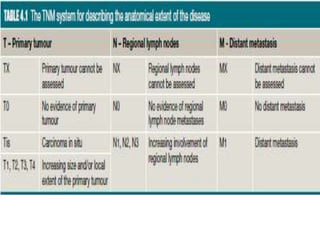
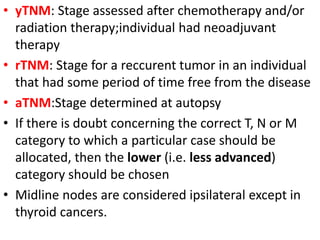
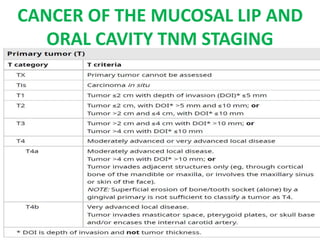
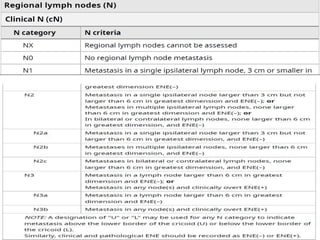
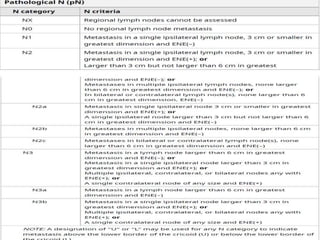
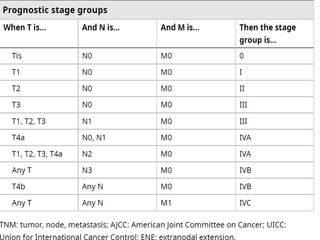
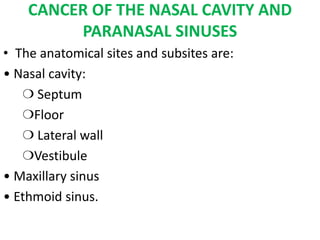
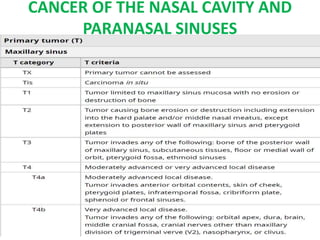
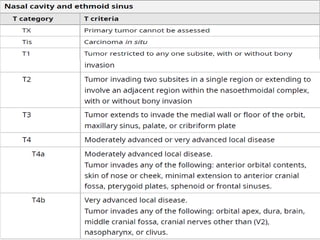
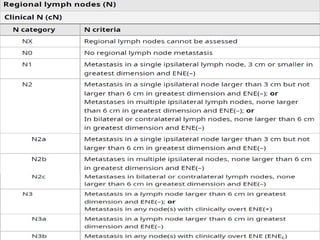
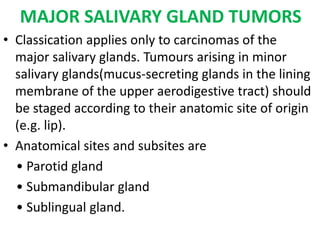
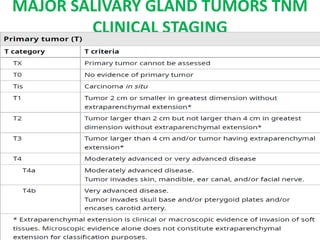
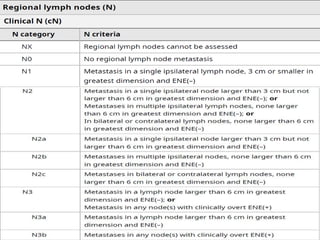
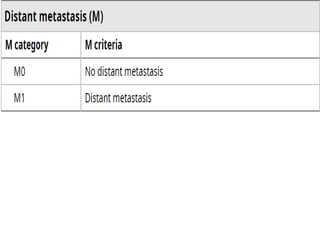
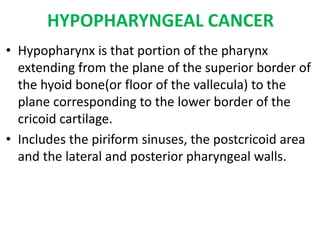
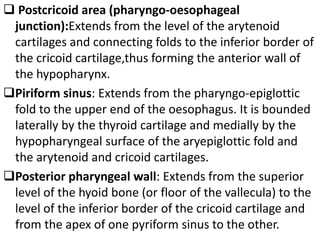
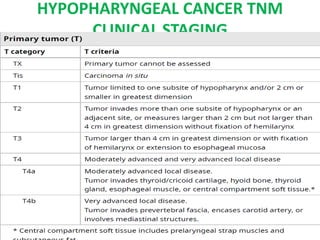
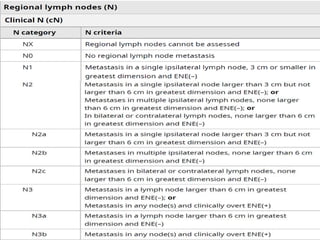
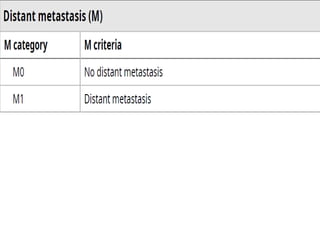
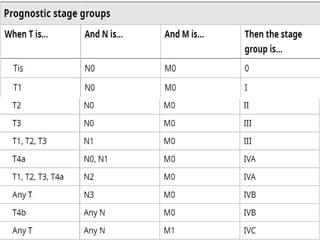
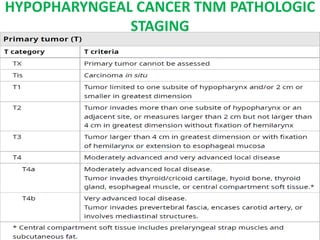
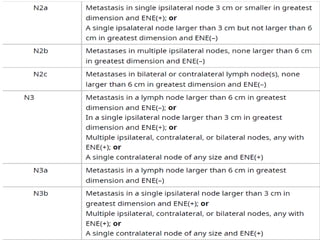
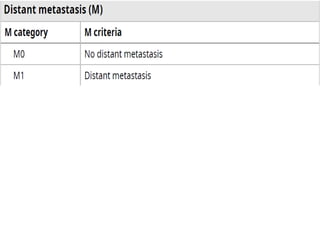
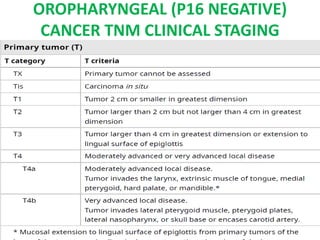
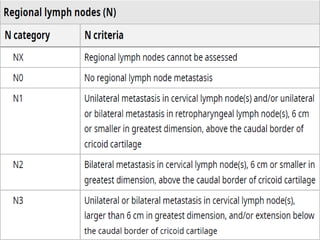
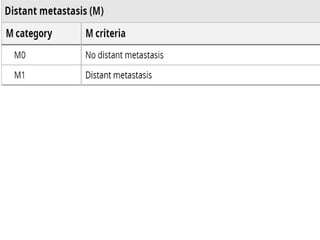
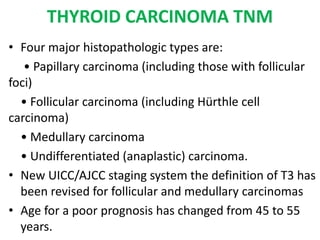
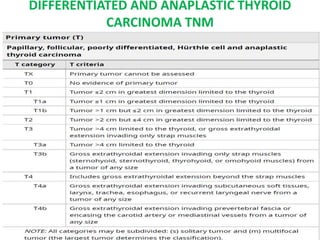
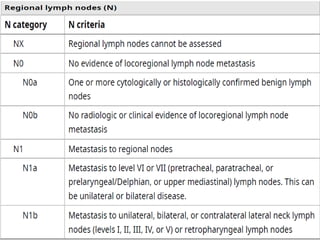
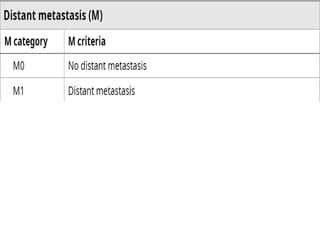
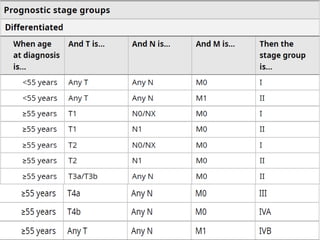
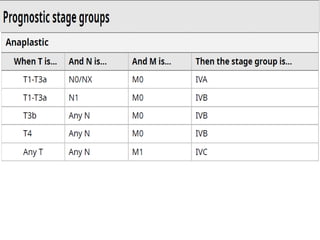
This document discusses the TNM staging system used for head and neck cancers. It provides definitions for the TNM categories describing tumor size, lymph node involvement, and metastasis. It then outlines the TNM staging criteria for various head and neck cancer types, including cancers of the oral cavity, larynx, hypopharynx, nasopharynx, thyroid, and major salivary glands. It also discusses limitations of the TNM system and the benefits it provides for treatment planning and prognostication.
![• Within head & neck , size of the tumor generally
defines the T stage.
• Exception :- vocal fold mobility in CA larynx
• Depth of invasion is now included within AJCC 8th
edition staging system of oral cavity CA & is
considered a separate entity to tumor thickness.
• Modifiers ‘’a’’ [less severe] & ‘’b’’ [more severe] can
be used within some T categories – further describe
tumor](https://image.slidesharecdn.com/tnmsystemsinent-221215182219-eee2de14/85/TNM-SYSTEMS-IN-ENT-pptx-9-320.jpg)
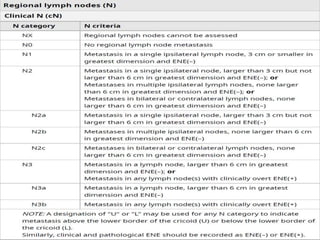
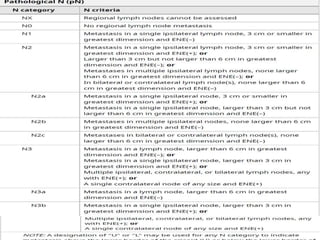
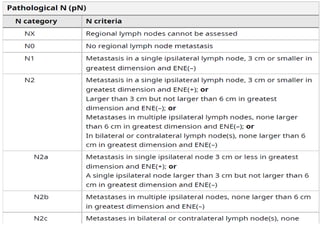
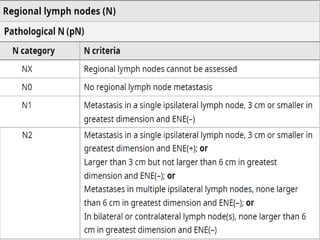
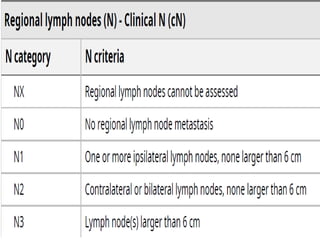
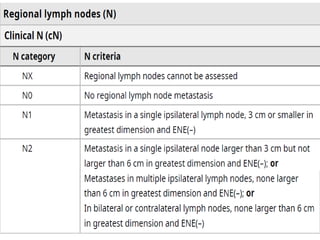
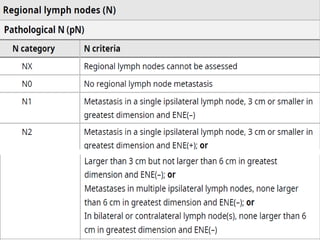
![• N describe spread of cancer to regional lymph
nodes.
• 5 categories.
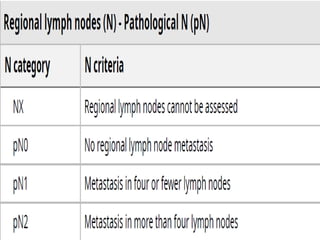
• Nx :- regional lymph nodes cannot be assessed.
• No,N1,N2,&N3.
• Basically described by size of the lymph node & is
modified by location of the involved nodes.
• Evaluation of surgically excised LN by a pathologist
can further affect N stage.
• Specifically ,8th edtn of AJCC includes additional
modifier of Extra-Nodal Extension[ENE] –denote
spread of tumor outside of the capsule of a LN on
HP sectioning.](https://image.slidesharecdn.com/tnmsystemsinent-221215182219-eee2de14/85/TNM-SYSTEMS-IN-ENT-pptx-10-320.jpg)
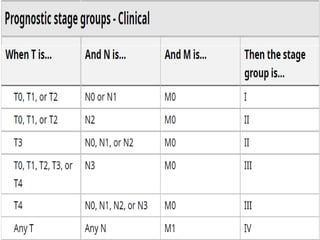
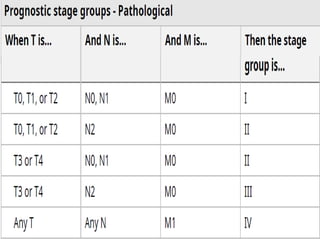
![• Clinical classification [pretreatment clinical
classification,designated cTNM] is evidence
acquired before primary treatment.Based on
information available prior to first definitive
treatment
• Pathological classification [postsurgical
histopathological classification,designated pTNM]
• Clinical stage is essential to selecting & evaluating
primary therapy.
• Pathological stage gives information for estimating
prognosis and calculating end results](https://image.slidesharecdn.com/tnmsystemsinent-221215182219-eee2de14/85/TNM-SYSTEMS-IN-ENT-pptx-13-320.jpg)
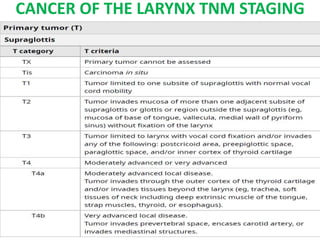
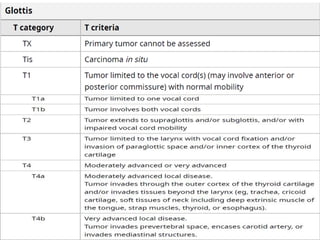
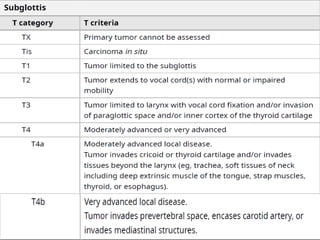
![CANCER OF THE LARYNX
• Anatomical sites and subsites are:
Supraglottis:
❍ Suprahyoid epiglottis (including tip, lingual [anterior],
and laryngeal surfaces)
❍ Aryepiglottic fold, laryngeal aspect
❍ Arytenoid
❍ Infrahyoid epiglottis
❍ Ventricular bands (false cords)
Glottis:
❍ Vocal cords
❍ Anterior commissure
❍ Posterior commissure
Subglottis.](https://image.slidesharecdn.com/tnmsystemsinent-221215182219-eee2de14/85/TNM-SYSTEMS-IN-ENT-pptx-24-320.jpg)

![LIMITATIONS OF ‘N’ STAGING
• Observer variability [presence of nodal
disease & size measurement]
• No inclusion of immunological status
• Importance of extra capsular spread
• N2 [B/L involvement] implies better prognosis
than N3[large nodes greater than 6cm]](https://image.slidesharecdn.com/tnmsystemsinent-221215182219-eee2de14/85/TNM-SYSTEMS-IN-ENT-pptx-102-320.jpg)
![CONCLUSION
• Current TNM system relies on morphology of the
tumor[anatomical site &extent of disease]with
little or no attention given to patient factors
• AJCC Task Force maintains that any new system
should be comprehensive and easily applicable to
all the major sites.
• Changes in the TNM classification should and will
only occur , based on the appropriate collection ,
presentation & analysis of data , in the forum of
the UICC & AJCC](https://image.slidesharecdn.com/tnmsystemsinent-221215182219-eee2de14/85/TNM-SYSTEMS-IN-ENT-pptx-104-320.jpg)
![REFERENCE
• AJCC Cancer Staging Manual, Eighth Edition
(2017) published by Springer International
Publishing.
• Scott-Brown’s otorhinolaryngology head and
neck surgery[8th edtn]
• Disease of ear nose and throat by Dhingra [7th
edtn]](https://image.slidesharecdn.com/tnmsystemsinent-221215182219-eee2de14/85/TNM-SYSTEMS-IN-ENT-pptx-107-320.jpg)