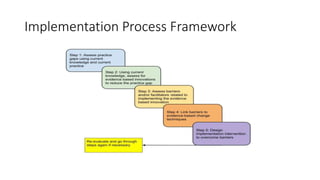
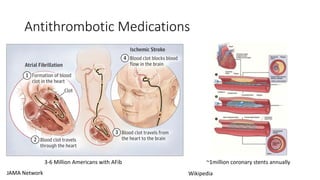
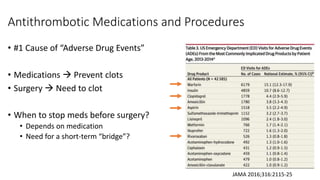
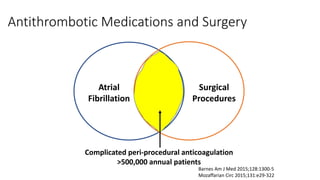
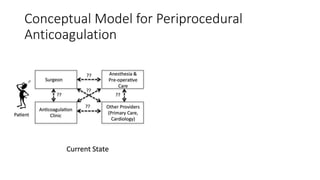
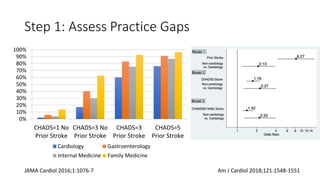
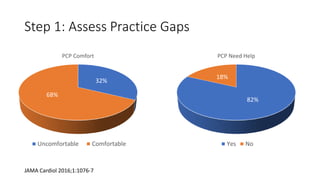
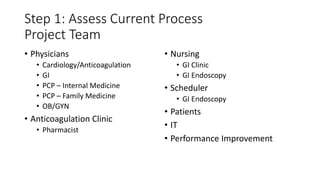
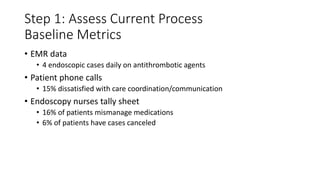
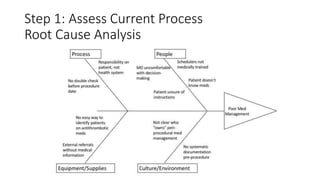
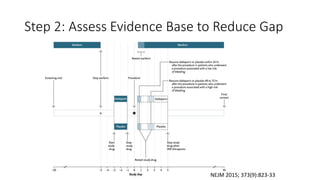
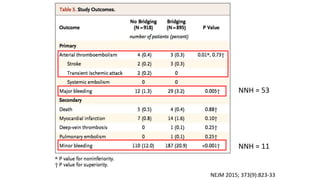
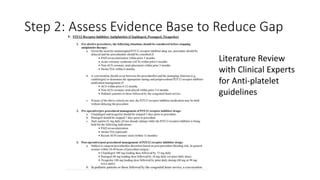
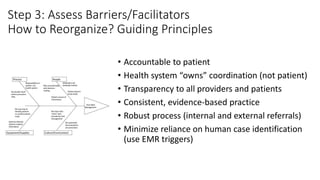
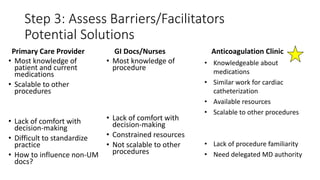
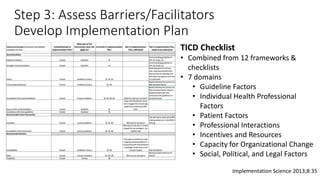
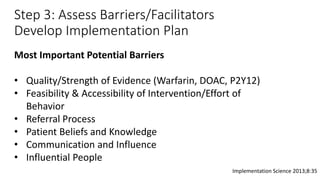
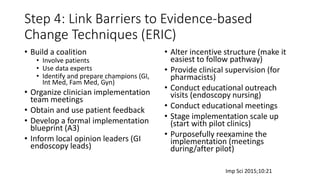
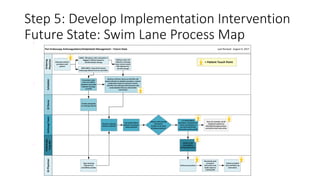
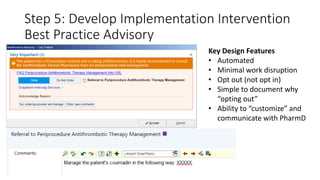
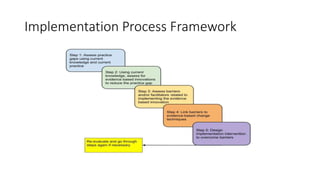
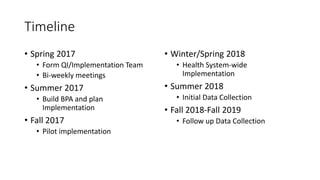
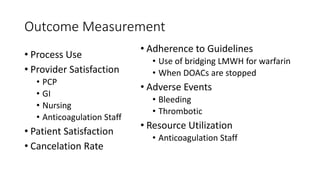
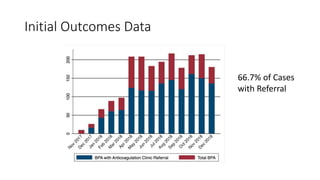
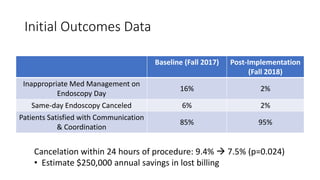
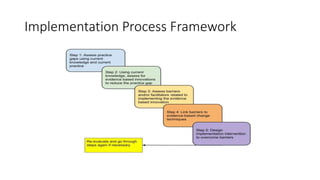
The document outlines a case study on improving antithrombotic management prior to gastrointestinal (GI) endoscopy, highlighting the need for effective medication management to prevent adverse drug events. A comprehensive implementation plan was developed through a multi-disciplinary team assessing practice gaps, evidence-based guidelines, barriers, and facilitators, leading to successful pilot programs that improved patient care coordination and reduced procedure cancellations. Initial outcomes show significant improvements in medication management and patient satisfaction, resulting in estimated cost savings.