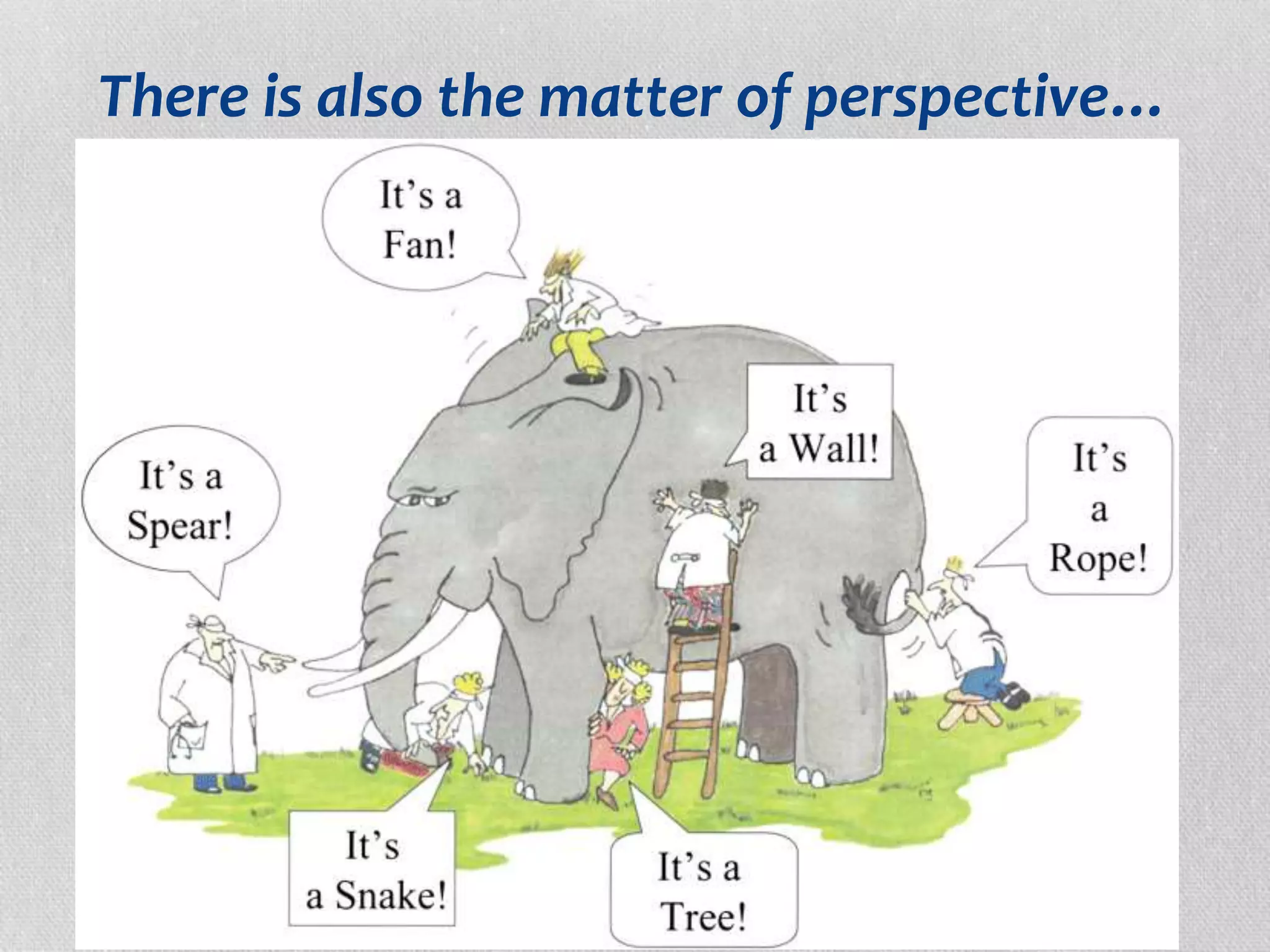
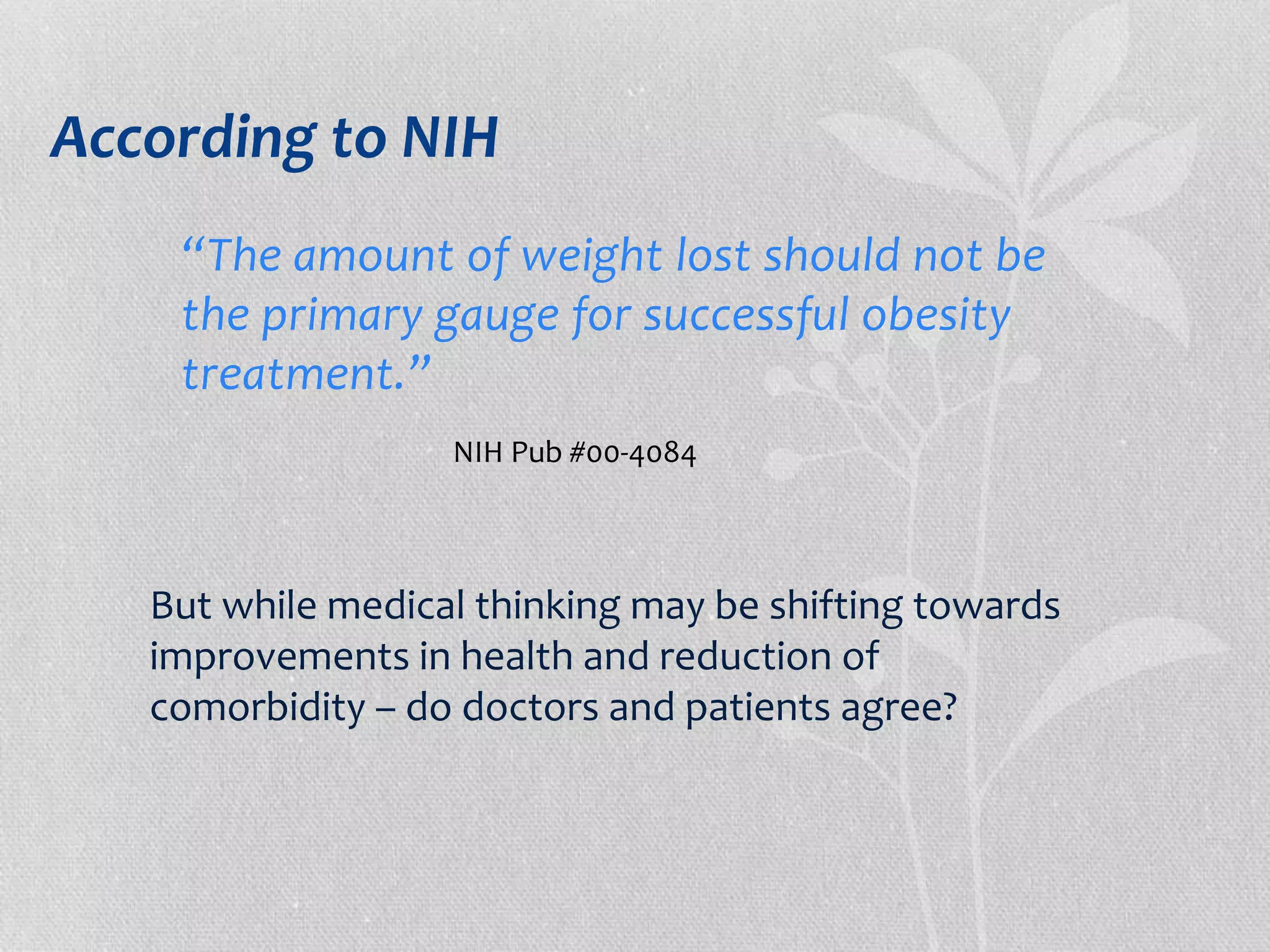
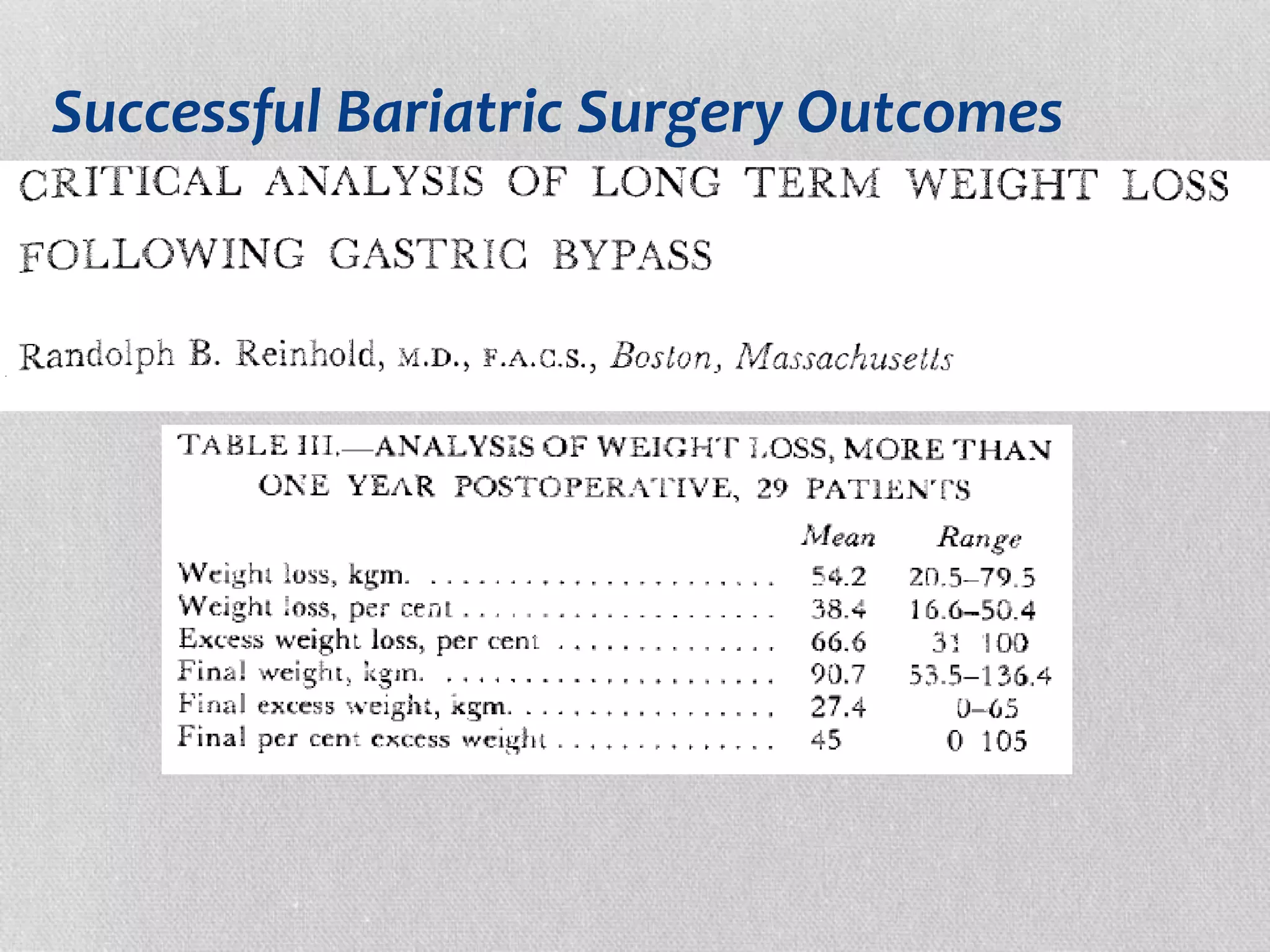
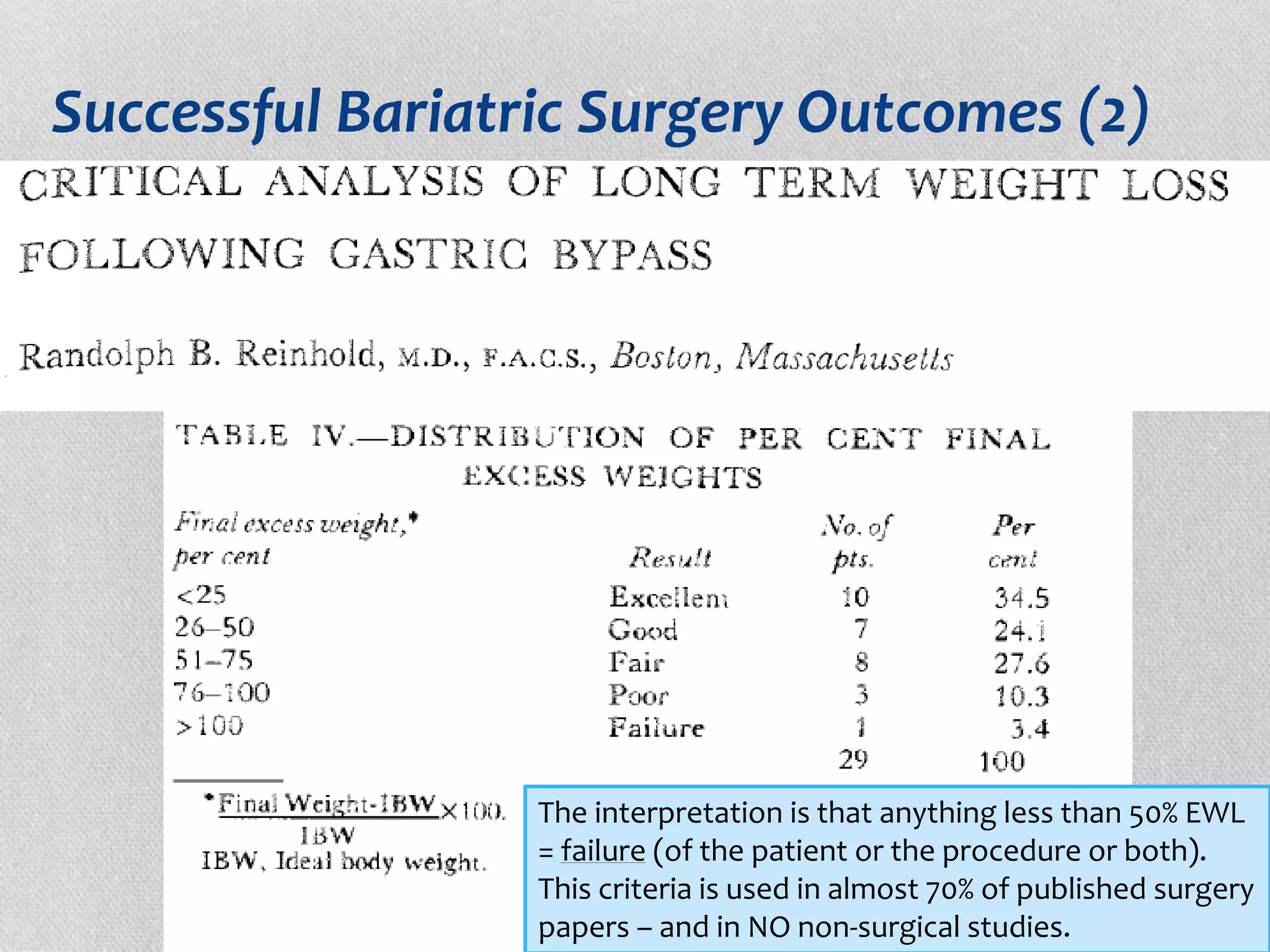
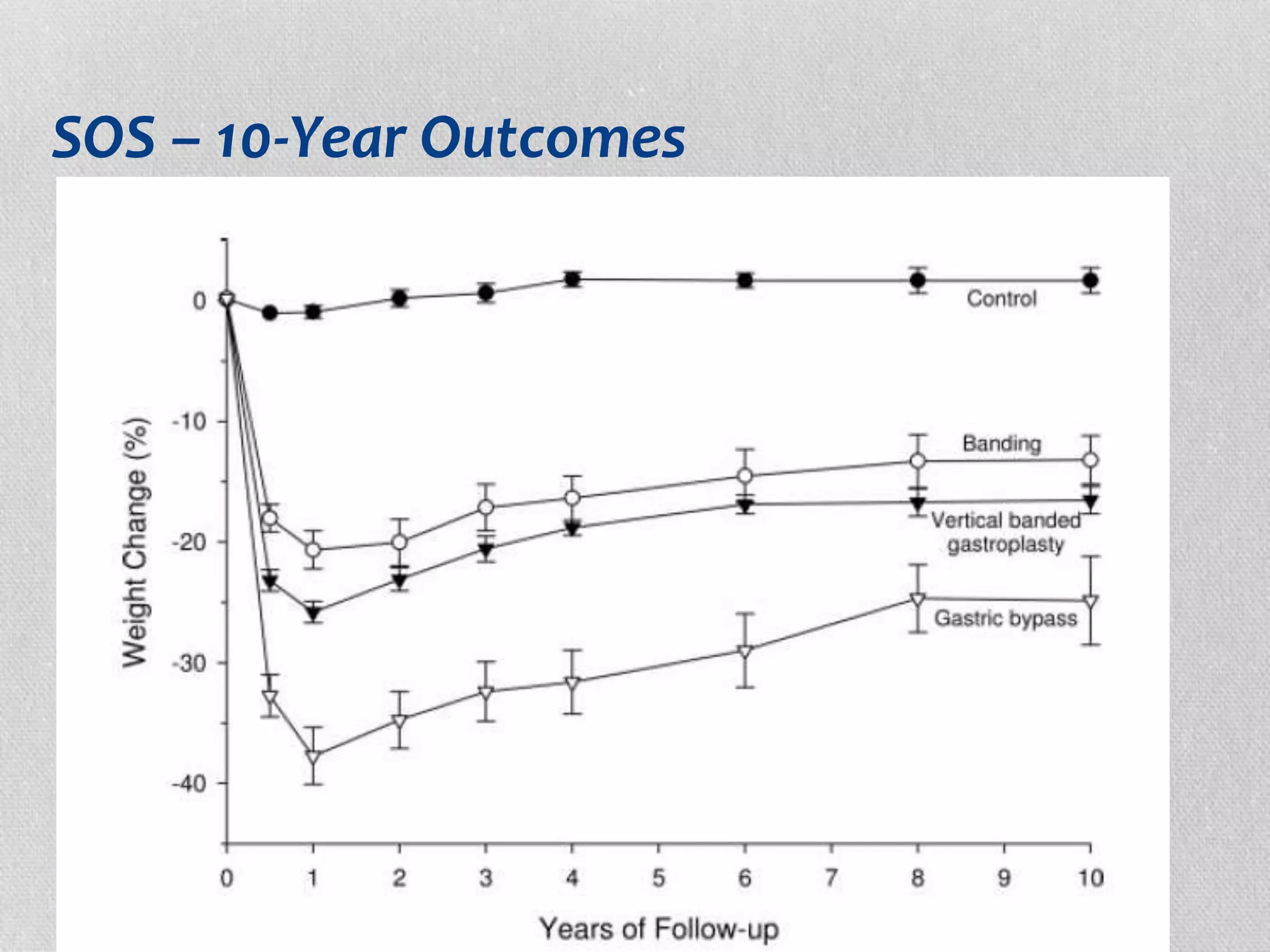
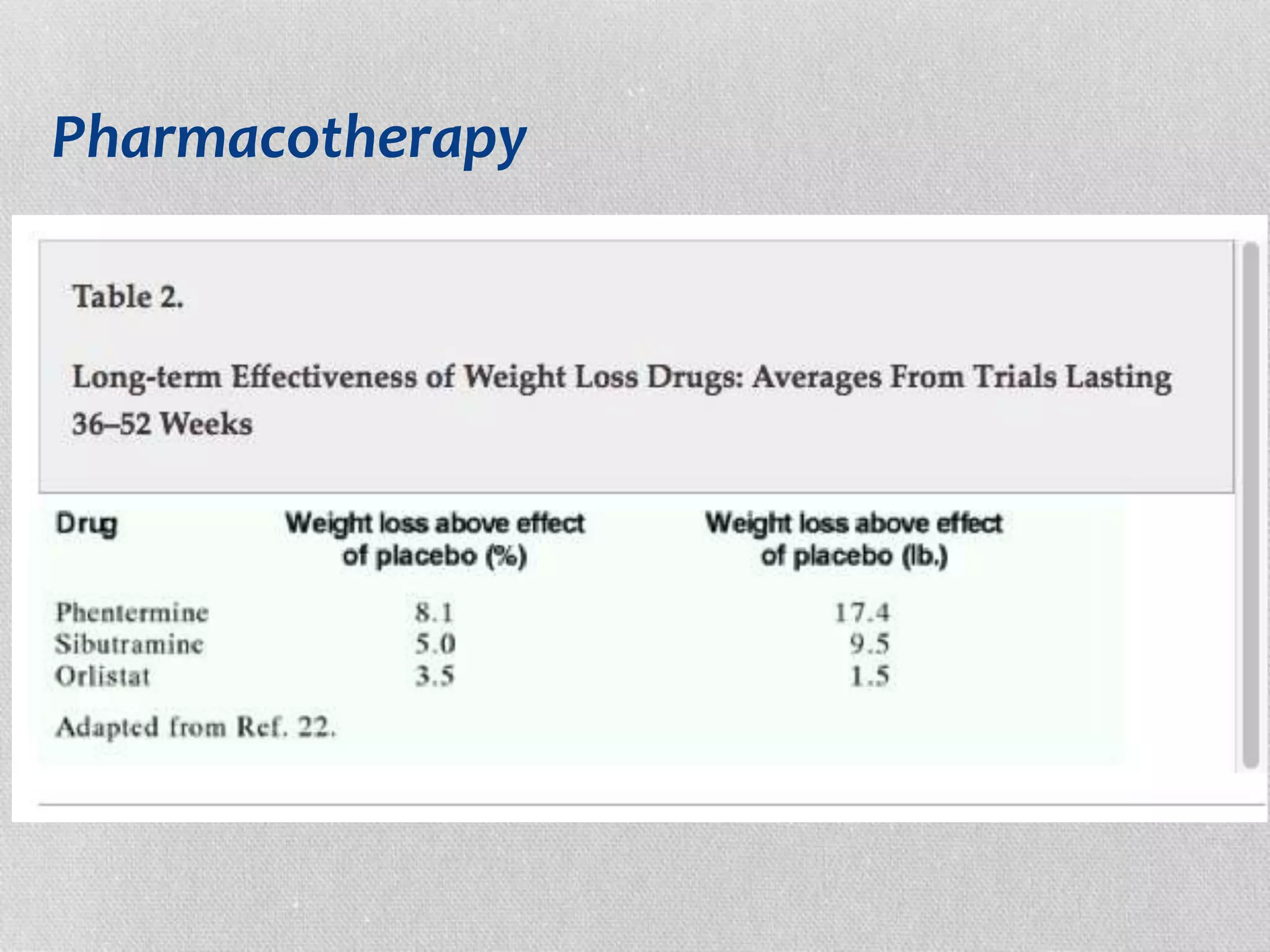
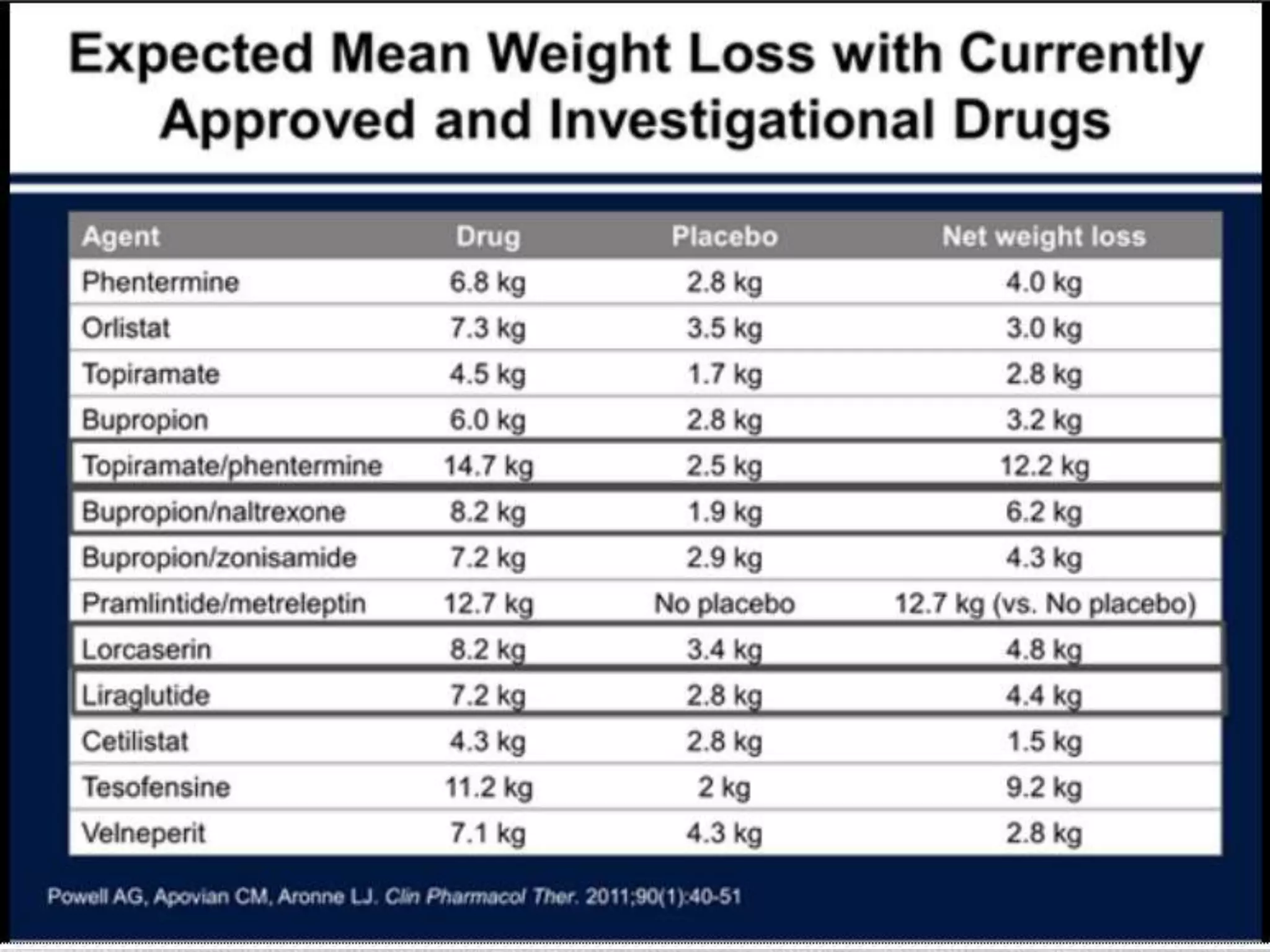
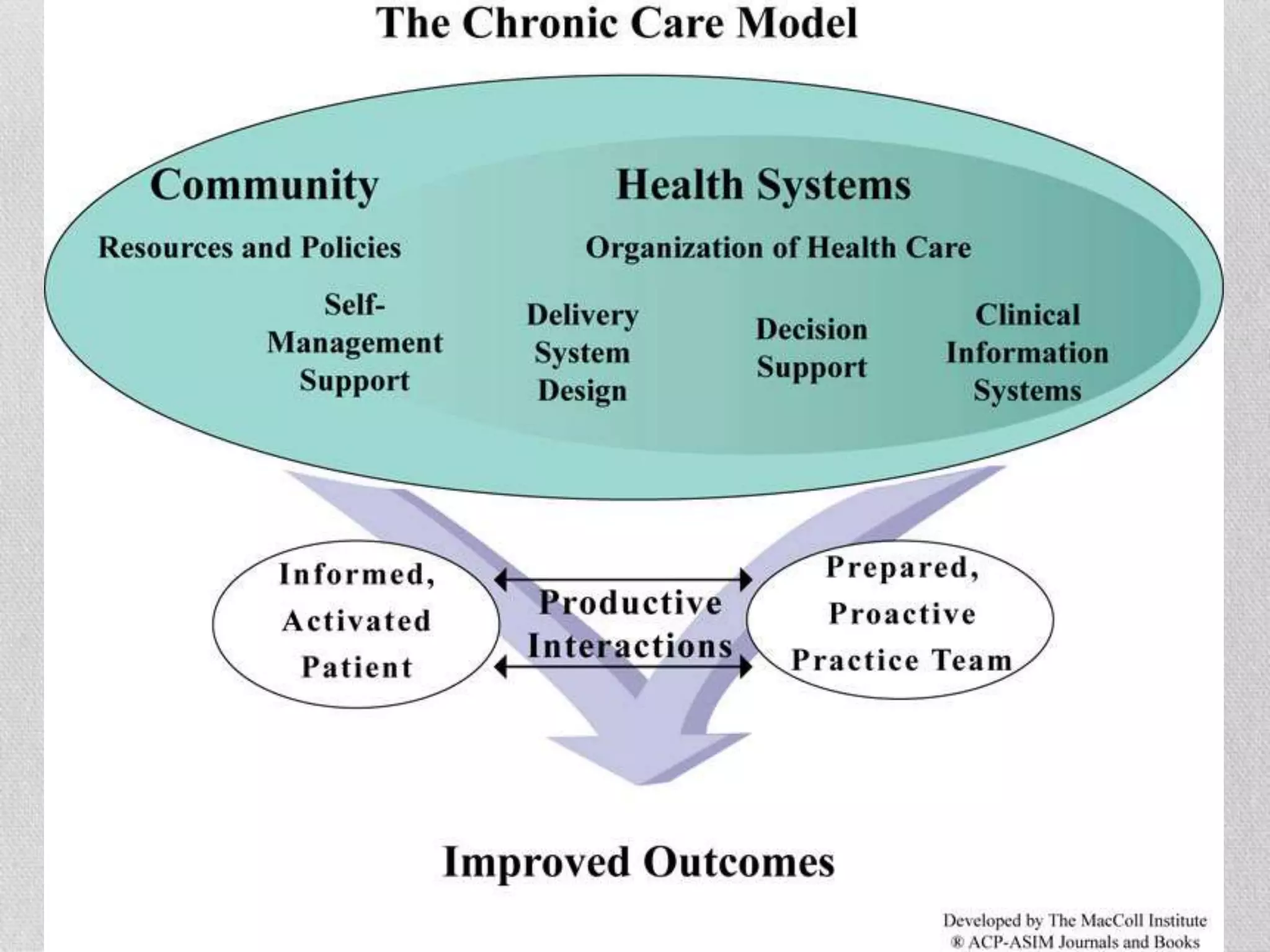
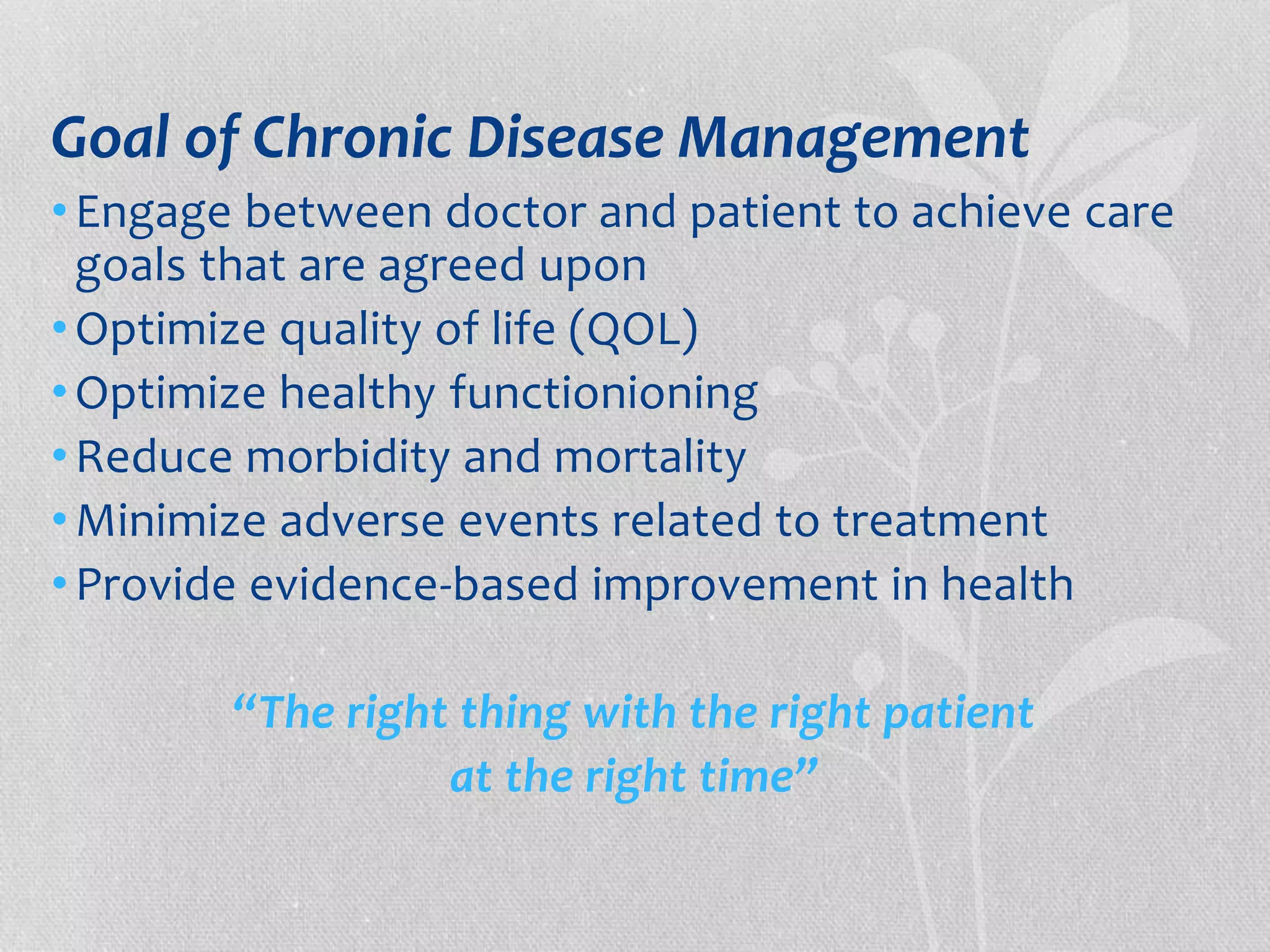
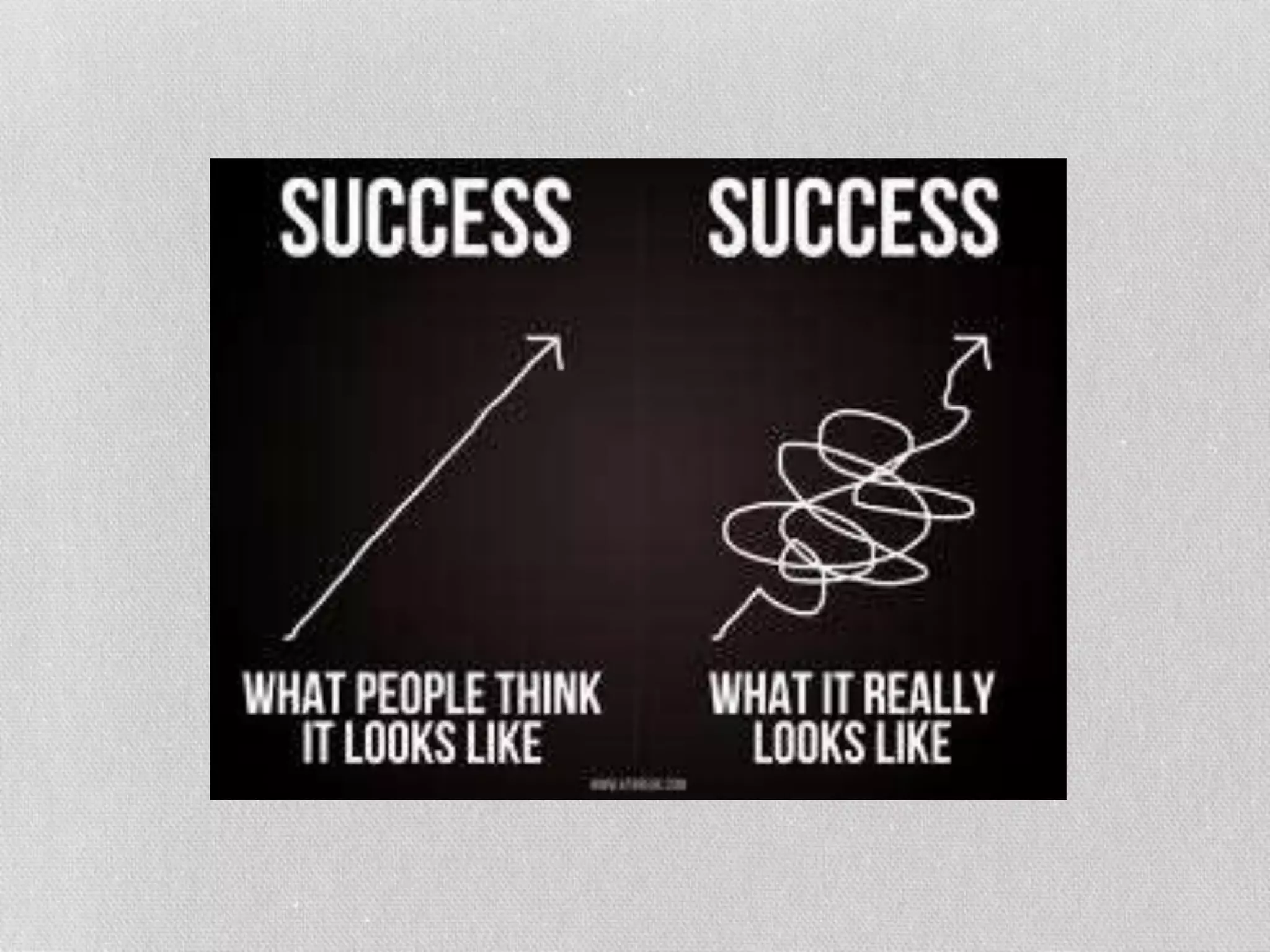
The document discusses the contrasting definitions of success and failure in obesity care between healthcare professionals and patients, highlighting how traditional metrics largely focus on weight loss rather than broader health outcomes. It emphasizes the need for alignment in understanding these definitions to improve treatment and patient satisfaction, while also advocating for a shift towards chronic management of obesity as a disease. Ultimately, it argues that success should encompass a variety of health and quality of life measures, rather than solely body weight targets.