The document discusses various aspects of communication, teaching, and documentation in nursing. It covers:
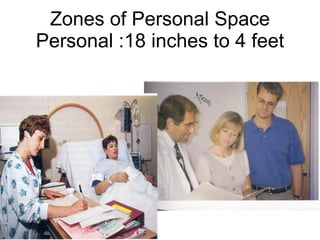
1) Different levels and elements of communication including intrapersonal, interpersonal, transpersonal communication and zones of personal space.
2) Therapeutic communication techniques nurses can use and non-therapeutic techniques to avoid.
3) The teaching role of nurses including standards, domains of learning, and how adults and children learn differently.
4) Guidelines for nursing documentation including what documentation must include, such as being factual, accurate, dated and using approved abbreviations.