The Rwanda Cure - Forbes Oct 2007
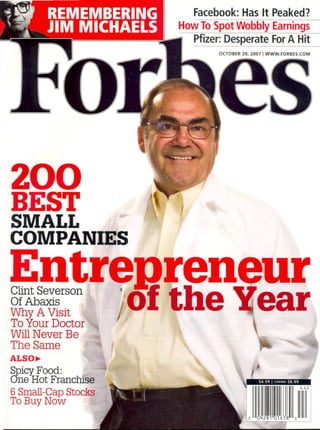
- 1. 200 BEST SMALL COMPANIES Entregreneur i &lin=rson 'jol the "'earWhy A VISIt / ~ ToYourDoctor ,WillNever Be ~ The Same j ,... . ALSO~ ~picy:Food: . ~J One Hot Franchise 6 Small-Cap Stocks To Buy Now t I Facebook:HasIt Peaked? I HowToSpotWobblyEarnings pfizer:DesperateForA Hit I OCTOBER29.2007I WWW.FORBES.COMI, , .. . . iI . i .-- I I
- 2. AidmAfrka AYANGE, RWANDA IS ONE OF THE POOREST towns in one of the poorest conntries on earth. This dusty settlement of25,000 farm- ers in the center of Africa has no rnnning water or electricity.It got its firstpaved road this summer. Mnch of the popnlation was mped out during Rwanda's 1994 genocide, and many current residents resettled here from elsewhere after the war. Some people here don't see as much as $50 in cash in a whole year. Until a ye", ago it was not uncommon in a single week to have the funerals ofthree young kids. Many of them died in their homes because their parents couldn't afford the town's 18-bed clinic, which was often out of drugs anyway. "I am used to the idea of death;' says 82-year-old Rosalia Kabera, who has lived in the town her whole life. "I have seen women die, young girls die and babies die during delivery:' Her I-year-old grandson, Daniel, died of malaria in 2006. His parents, who live in a nearby town, didn't seek treatment nntil it was too late because they conldn't afford a 30-cent co-payment. But this year is different. Only 28 children nnder the age of 5 have died, down from over 100. The difference is that the village now has a functioning health center. It is staffed by nurses, not doctors, and has little high-tech equipment other than a few microscopes. But it provides basic services like generic anti- biotics, rehydration fluids for diarrhea, malaria medicines, insec- ticide-treated bed nets and, beginning soon, AIDSdrugs. A little over a year ago the clinic was seeing 5 to 10 patients a day.Now it sees 200, and the biggest problem is overcrowding. The changes are possible because of a Columbia University program that has pumped $145,000 into the health center, money used to hire and train more nurses and install an order system so drugs don't rnn out. The program is run by Joshua Ruxin, a Columbia professor of public health. "We are trying to take health systems that have declined and bring them into the 21st century:' says Ruxin, who hopes to bring sintilar iroprove- ments to 32 other clinics in Rwanda. "In IS years people are going to say stuff happened here. It wasn't iropossible:' THERWANDACURE Western do-gooders are pouring billions of dollars into controlling malaria,AIDS and other killers ravaging the world's poorest continent. Nowcomes the hard part I ByRobert lc~mgreth 142 FORBES OCTOBER 29. 2007 ~ I I I
- 3. Of the 9.7 million annual deaths world- wide of kids under 5, at least 6 million could be averted with existing technologies, a 2003 study found. The million malaria deaths could be dramatically reduced with $5 bed nets. Oral rehydration fluids, at 25 cents per treatment, can prevent many of another 1.6 million deaths from severe diarrhea. And $1 generic antibiotics can cure the 1.8 mil- " lion who die every year from bacterial pneumonia. Measles still ~ kills 390,000 a year; the vaccine to stop fbat was invented in 1963. ~ Some of what sub-Saharan Africa needs is new technology, ~ like a malaria vaccine. But what's needed most, particularly in< " Africa, is better logistics. Much of Africas population lives in ~ rural villagesand farms miles from the nearest clinic. Many ~ countries have one doctor or less for every 10,000residents. It's A Webcam works wonders in signing up poor villagers for health coverage in rural Rwanda. OCTOBER 29. 2007 FORBES 143 - ,
- 4. . not uncommon for rural folks to die at home without ever seeing a doctor or nurse. "The hardest truth for people to come to terms with is that 'the practical solutions are already out there, but they are not being applied;' says Ruxin, who leads the effort in Mayange. (It is part of a larger Columbia University/United Nations undertaking called Millennium Villages, which focuses on making broad improvements in 12 clusters of poor villages across Africa.) Adds Fred N. Binka, a public health expert at the University of Ghana: "Donors always want to do something new. The simple things aren't so glamorous:' Economists debate whether the $600 billion (in today's dollars) spent on foreign aid to Africa in the last 46 years has done any good. But health spending has delivered visible results. Smallpox was eliminated in 1980 after a 20-year effort. Merck's .,. 20-year-program to donate its antiparasitic ivermectin has helped treat 530million cases of onchocerciasis (river blindness), spread by black flies in some parts of Africa; it has prevented 40,000 cases of blindness per year. Cases of Guinea worm, a par- asite that slowlyburns through the skin, are down from 3.5 mil- lion in 1986 to 25,000 last year, thanks to efforts of the Carter Center and others. Yet, until the last fewyears, the industrialized world neglected many developing-world diseases, even as malaria and AIDSspi- raled out of control in Africa. "When I went to medical school, global health was almost a nontopic; recalls Tadataka Yamada, 62, the former GlaxoSmithkline executive who now leads the Gates Foundation health efforts. Rich countries spent $100 mil- lion on malaria control in 2000,according to one study-20 cents per case. They spent $69 million annually on AIDSin Africa, according to a 2001 Lancet study. The pessimists said it was simply impractical to bring compli- cated drug regimens into poor regions with little infrastructure. 144 FORBES OCTOBER 29, 2007 A Bush Administration aid official told the Boston Globein June 200I that bringing more AIDSdrugs to Africa wouldn't work because many residents "don't know what Western time is:' One of the first to prove otherwise was H.rvard Medical School physician Paul Farmer, In 1985 he started a clinic in one of the most godforsaken parts of Haiti, among the poorest coun- tries in the Western Hemisphere; it soon expanded into a hospi- tal. For years skeptics told him his programs were too complex or expensive to work in dirt-poor settings. But by 2003 the centers had treated 1,050patients with AIDSdrugs. The Haitian patients turned out to be more reliable than low-income patients in Boston at adhering to their regimens. Celebrity economist Jeffrey Sachs, then at Harvard and now director of Columbia University's Earth Institute, started think- ing about health care after a business trip to Zambia in 1995."I Joshua Ruxin (left) aims to make Rwanda into a health care success story by improving management practices in isolated dinics; here he is with patients at one rural center. Above. a nu..e consults with a mother at Mayange. had never seen people dying before my eyes. It was the most shocking thing:' he says."I had no idea that people died of the most extreme lack of access to the most simple things; Sachs at first presumed that rich countries must be helping as much as they could, but the more he looked the more he real- ized how little was being done despite the rhetoric. He began exposing the meager response of the developed world. He also examined the relationship between malaria and poverty, concluding that a severe malaria problem reduced a country's economic growth by 1.3 percentage points a year, even after 0 other factors such as geography and governance were taken into ~ accpunt. Youdidn't need a humanitarian motive to stop malaria. ~ It made economic sense. ~ In 2000 Sachs started pushing in speeches and journal arti- ~ cles for a worldwide fund for treating poor-country plagues. ~ Instead of having to negotiate with dozens of donors, African; countries could set their own plans and apply for grants to buy ~ AIDSor malaria treatrnents:The grants would be evaluated on ~ technicalmerit, just like medicalgrants at the Nationallnsti- ~ tutesof Health. ~ r c ..I..
- 5. In 2002 the Group of Eight countries and others created the Global Fund to Fight AIDS,Tuberculosis and Malaria, much along the lines Sachshad advocated. It has distributed $8.6 billion so.far,half to Africa; it includes two-thirds ofall worldwide fund- ing for malaria and tuberculosis. It tries to hold countries accountable by using accounting firms to audit results. Out of 450 grants, only 9 have been canceled so far for poor perform- ance; another 3 have been suspended for corruption. Others also stepped up. Last year the Bill & Melinda Gates Foundation spent $360.5 million delivering health intervention to poor countries; in fiscal 2007 the Bush Administration spent $4.7billion on treating AIDSand other diseases in poor countries. Novartis sold 62 million courses of its malaria drug, Coartem, at cost to poor African countries. Bythe end of 2006, 1.3 million Africans were on HIVtreat- AidJoAfrka others. When they started, there was not one doctor in this impoverished region of 425,000 people near the Tanzanian bor- der, 7 miles from the nearest paved road. The drug storeroom was nearly bare. Partners in Health quintupled the nursing staff and brought in six Rwandan doctors and the first AIDSdrugs to the region It hired hundreds of part-time workers to visitpatients and make sure they were taking their drugs. The Rwinlcwavu'Hospitai has treated 1,995patients with illY drugs-and kept 96% of them alive.It delivers 100babies a month, versus 5 a month in 2005. Jennifer Uwimana was a living skeleton when she arrived at Rwinkwavu in January 2006. She was vomiting, had bad diar- rhea and weighed just over 8 pounds, 40% the normal weight for a I-year-old.She had AIDS and tuberculosis,an.especially lethal combination that has killed millions across Africa. With- out treatment she wonld have died within weeks. But doctors ment, up from 100,000 in 2003."When it comes to Africa, the belief is that not much can be done. My goal is to prove otherwise; says Abdirahman Mohamed, a Somali-born American doctor who leads a Gates-funded program to distribute insectidde-treated bed nets and control malaria in Zambia. In June an HIV"implementers" conference brought 1,500doctors and pub- lic health experts to Rwanda to discuss how to get AIDSdrugs to Africa. "This is all brand new. It is astounding;' says Harvard's Farmer. "Afewyears ago there were no implementers:' ~ Rwanda has 899 doctors fora nation of9.9 million,bntonly 185 E arein rural areas,wheremost ofthepopnlation lives.Per capitahealth ~ spending is $14 a year,versus $6,000in the U.S.But the Rwandan ~ government isstable,the cellphones work and the economyisgrow- ~ ing-notwithstanding a low scoreon the Heritage Foundation/Wall i Street Journal index of economic freedom. "The level of vision for ; what the country will do with the average health center is far more ~ ambitious than I have seen anywhere else" in Africa, says Colum- ~ biaSRuxin, who has also worked in Kenya,Ethiopia and Nigeria.< ~ In 2005 Farmer's Partners in Health charity renovated a ~ decrepit, barely functioning public hospital in rural Rwanda, with ~ $2 million in funding from the William J. Clinton Foundation and I Jennifer Uwimana, at left. with Mom. was weeks from death bef"", a remarkable recovery- Above, Ruxin's colleague Blaise Karibushi. At right, a community health worker in Mayango. were able to treat her with a cocktail ofTB medicines, antibiotics and generic AIDSdrugs. Jennifer's HIYis now under control, her tubercnlosis is cured and her cheeks are chubby. At 2112she cruises around the hospi- tal malnutrition ward (where her mother now works), boldly starting a game of peek-a-boo with a stranger and grabbing his camera to see the display. Her mom, Olive llibagiza, sometimes looks at her child, amazed at the turn of events. "Where I came from and where I am now, it is unbelievable;' she says. Ruxin became fixated on Africa after the big Ethiopian famine of 1984.While stillin high school he founded a student charity to raise money for hungry children; by his senior year it had chapters nationwide. But after gening a Ph.D. in the history of medicine, he concluded that charitablegroups didrit have the answersand went to wor!<:in the private sector asa consnltant to developingcountries. His work eventually led him to croSSpaths with Sachs,who hired him. He now supervises a staffof 85 aid workers in Rwanda. When Ruxin visited Mayange in 2005, there were no nurses I OCTOBER 29. 2007 145FORBES - -
- 6. AidJoAfrka present even though it was the middle of a workday. The health center had such a bad reputation that locals would walk miles to avoid going there, saysRanvn-Dhillon, an American medical stu- .dent who helped out in Mayange for 18 months. When he started, the village was in the midst of a drought, and malnutri- tion was so prevalent that Dhillon would shove 16 skinny kids into the project's SUVto drive them to a hospital where food was available. For the first few months so many people were dying that Dhillon spent much of his workweek delivering bodies back to grieving families and organizing and attending fimerals. A few radio ads brought in dozens of unemployed nurses from nearby; 11 were hired to bring the staff up to 15. This helped the clinic stay open all night to deliver babies; previously -most momshad deliveredin their homeswithout professional help. Now 80% of births take place at the center. The health center was only a few hundred yards from electric transmission lines, but nobody had ever bothered to connect it. Ruxin persuaded the government to do that. Alison Hager, a Pfizer finance official who volunteered in Rwanda for six months, got her company to donate 100 used laptops for Mayange and other nearby clinics, for use in tracking drug inventories. One. problem was getting people to come to the health center. Rwanda requires citizens to pay a $2 annual premium for health coverage and get a photo !D,but the nearest store with a camera was a 7-mile walk from Mayange. The solu- tion: a $35 Webcam attached to the laptop. Vumumlriya Mugorewase, 47, lives in Mayange with her six children. She makes $8 per month braiding hair. In the past she used traditional African healers, even though their medicines didn't work, because she couldn't afford the national health plan. Her 16-year-old daughter, Madeline, nearly died from malaria in June 2006. She survived only because Mugorewase ran into Dhillon on the street one evening a week after Madeline had developed a fever. They took turns carrying the nearly comatose child to a car to got her to a hospital in the nick of time. In the fall of 2006 Mugorewase was able to sign up for the health plan at a reduced rate (subsidized by the Millennium Villages project) via the Webcam. Since then she has used the 146 FORB'S OCTOBER 29, 2007 - ,." health center for everything from various fevers to her kids' night terrors. "1have never had proper care like this before;' she says. Can the progress at Mayange (or Rwinkwavu) be dupli- cated elsewhere? New York University econ,omist William Easterly is what you might call a compassionate skeptic. He says: "People like Jeffrey Sachs and Bill Gates see themselves as messiah-like figures who are going to change the world. In the real world money and technology is 5% of the solution; 95% is implementation. Youneed a functioning public I)ealth system, and that is exactly what is missing in most of Africa. ... If only we had good Latin names for diseases like 'missing health worker' or 'stolen drugs' -those should be the diseases that donors should treat:' . Easterly says efforts to help places like May,mge are "like trying to create a miniature utopia in the middle of a dysfunc- Weighing babies at the Mayange health center (left). Rosalia Kabera, 82, has watched many people die from treatable diseases. Kids play in a typical Mayange street (right). tional society you cannot fix. They cannot be replicated, they cannot be scaled up;' (Sachs dismisses his crit- ics as "professional complainers. If they want to do something some other way, do it. If all they want to do is complain, stay out of the way:') Mayange is snccessful in part because the Millennium Villagesproject pays the salaries of 14of the 17nurses now there. The Rwandan government is supposed to eventually take over more nurse salaries. The typical rural clinic in Rwanda is a lot farther than Mayange'sfrom the electric grid. With funding from the Glaser Progress Foundation, Ruxin and his Rwandan colleague Blaise Karibushi are trying to help 32 isolated clinics better manage the limited resources they have. Laptops, for example, help nurses keep track of who has been treated for what, so clinics can qualify for government bonuses. But where does the electricity come from? One forlorn clinic in Mareba, miles down a hilly dirt road from ~0 Mayange, has two laptops to track drug inventory and ~ expenses. The clinic's solar-powered batteries are able to ~ run only one at a time, along with some dim fluorescent ~ bulbs. Ruxin doesn't have enough money to put in a better ~ solar energy system. F ~