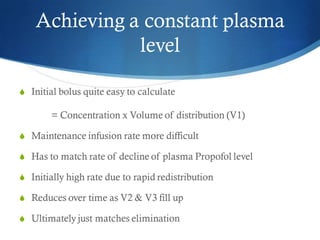
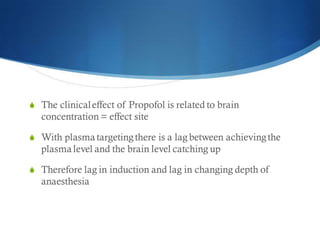
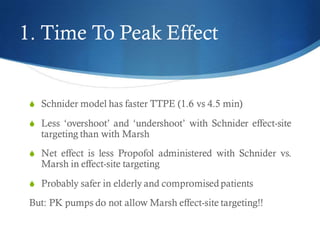
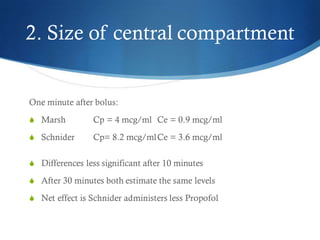
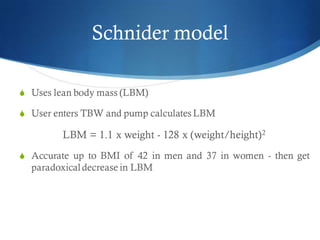
This document discusses total intravenous anesthesia (TIVA) and target-controlled infusion (TCI) systems. It compares the Marsh and Schnider pharmacokinetic models for propofol TCI. The Schnider model accounts for patient characteristics like age, weight, height and gender, while the Marsh model only considers weight. The Schnider model also has a faster time to peak effect of 1.6 minutes compared to 4.5 minutes for Marsh. Overall, the document recommends using Schnider for effect-site targeting and Marsh for plasma targeting in TCI systems to optimize propofol delivery and reduce the risk of patient awareness.




















































![Janmahasatian Formula
Male = [9270 x weight (kg)] / [6680+216 x BMI]
Female = [9270 x weight (kg)] / [8780+244 x BMI]](https://image.slidesharecdn.com/tci-models-for-dummies-230826013234-fa60ed74/85/tci-models-for-dummies-pdf-62-320.jpg)