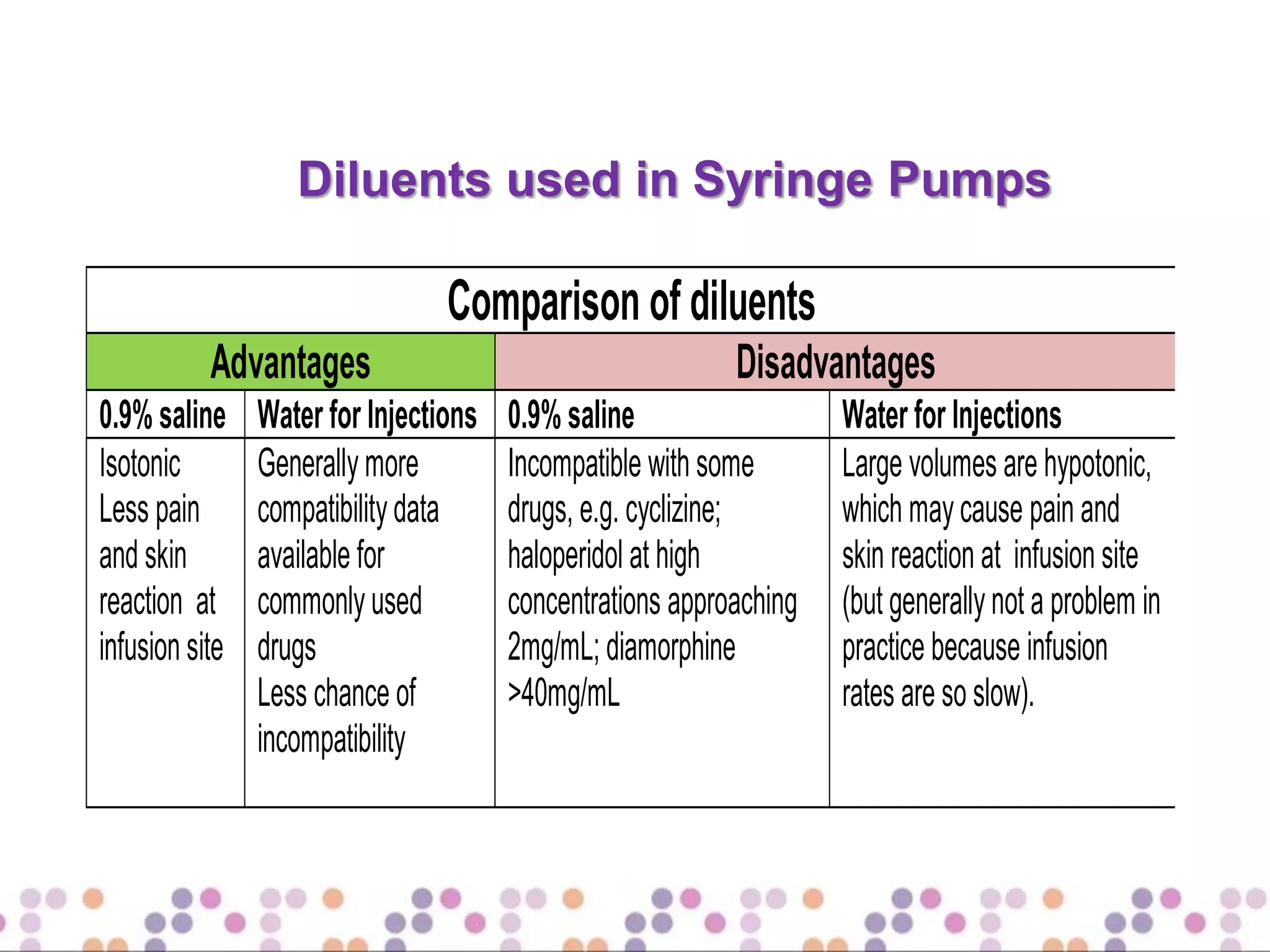
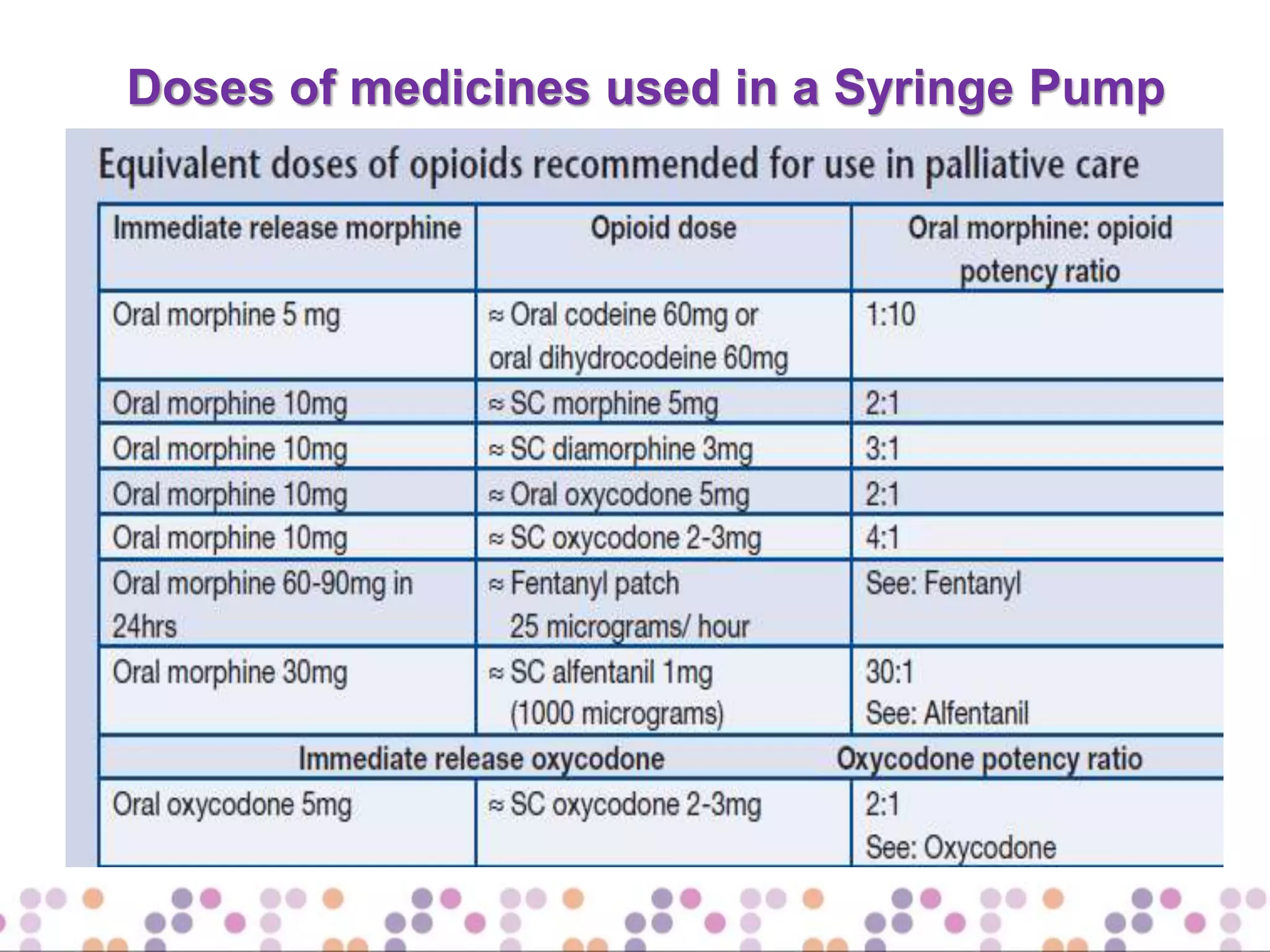
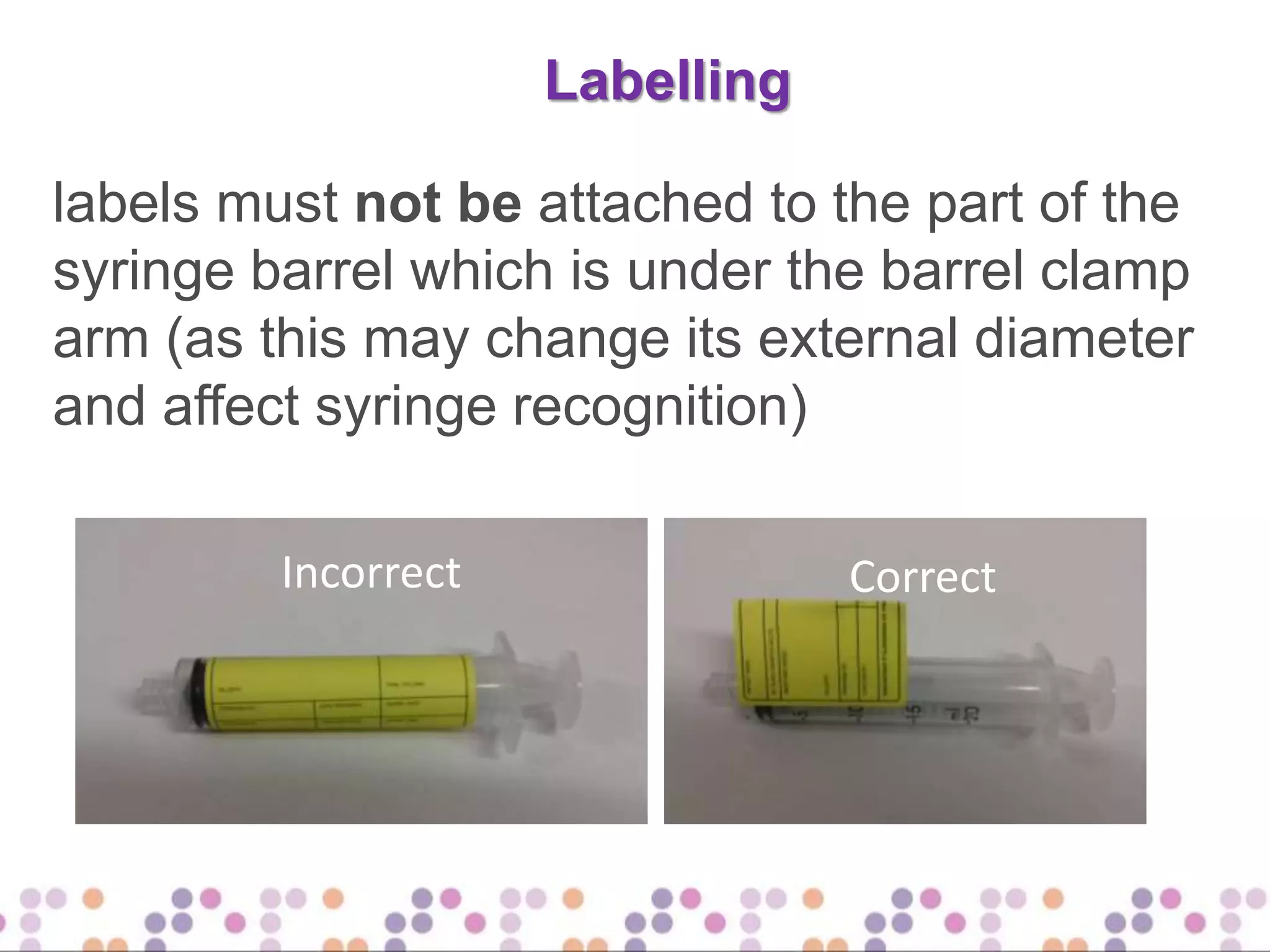
This document provides information about using a syringe driver or pump. It discusses what a syringe driver is, the advantages and disadvantages of using one, and when they should be used. It describes common medications administered via syringe pump for pain, anxiety, respiratory secretions, nausea, and more. Guidelines are provided around medication doses, diluents, compatibilities, volumes, and labeling for syringe pumps.