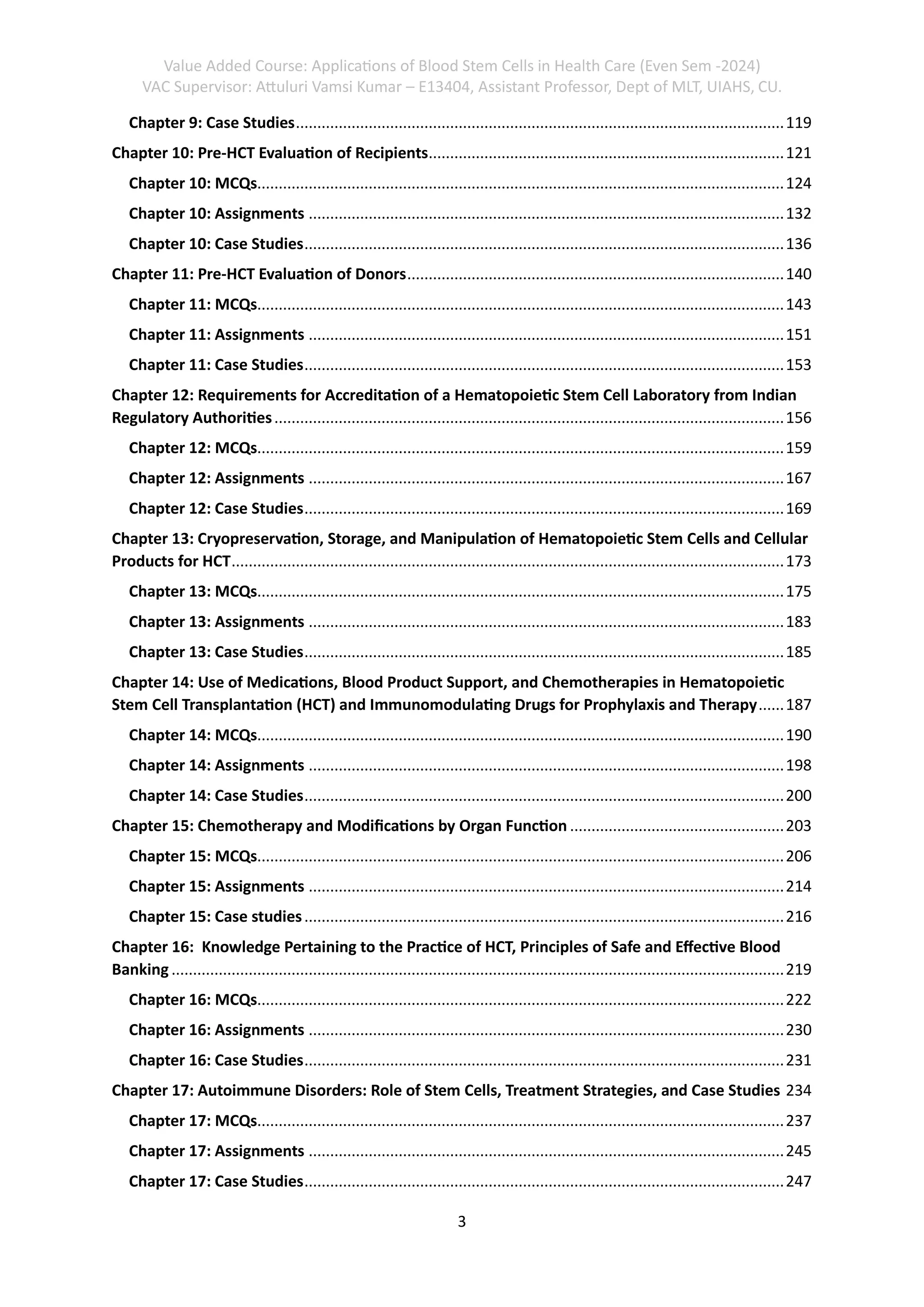
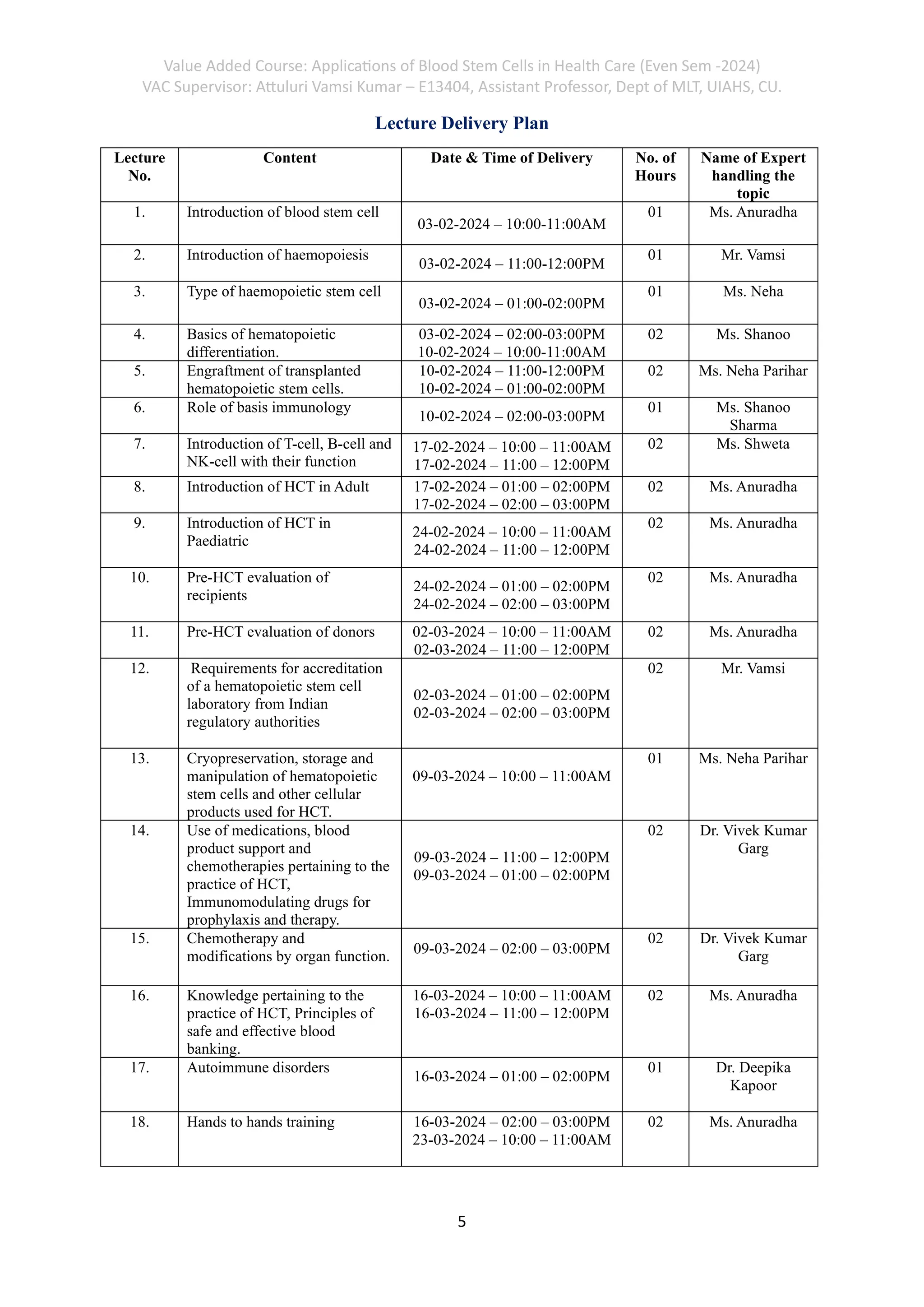
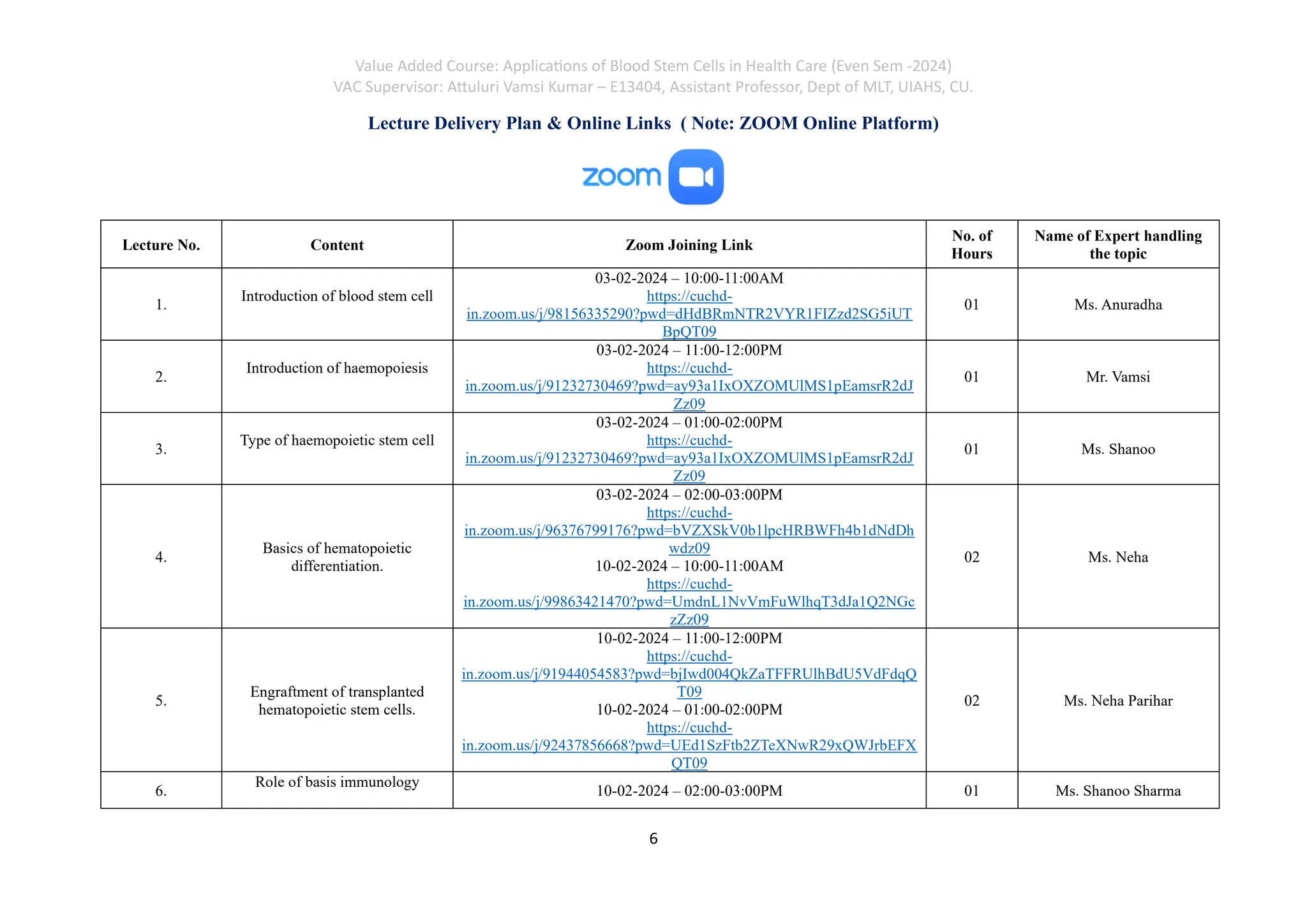
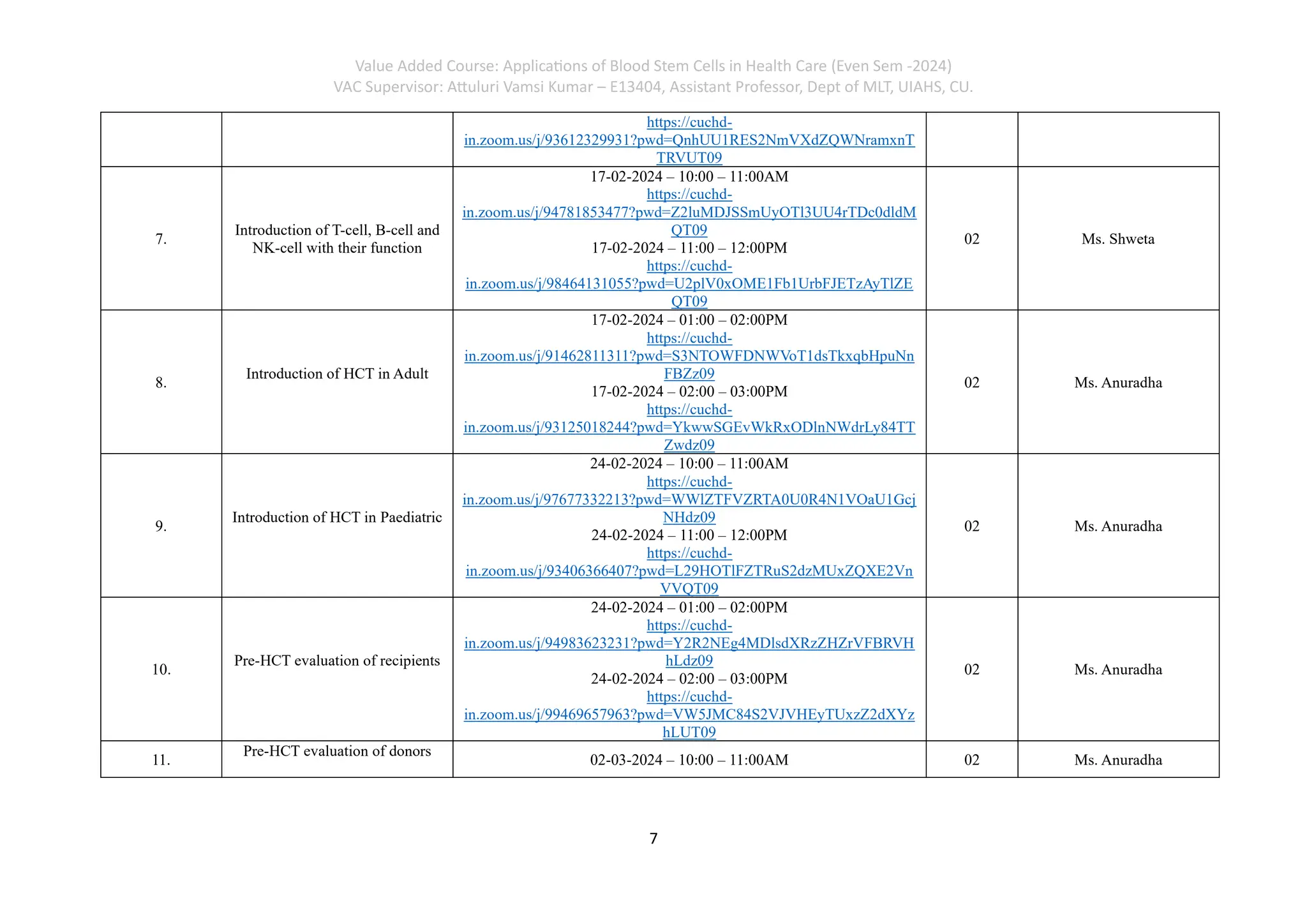
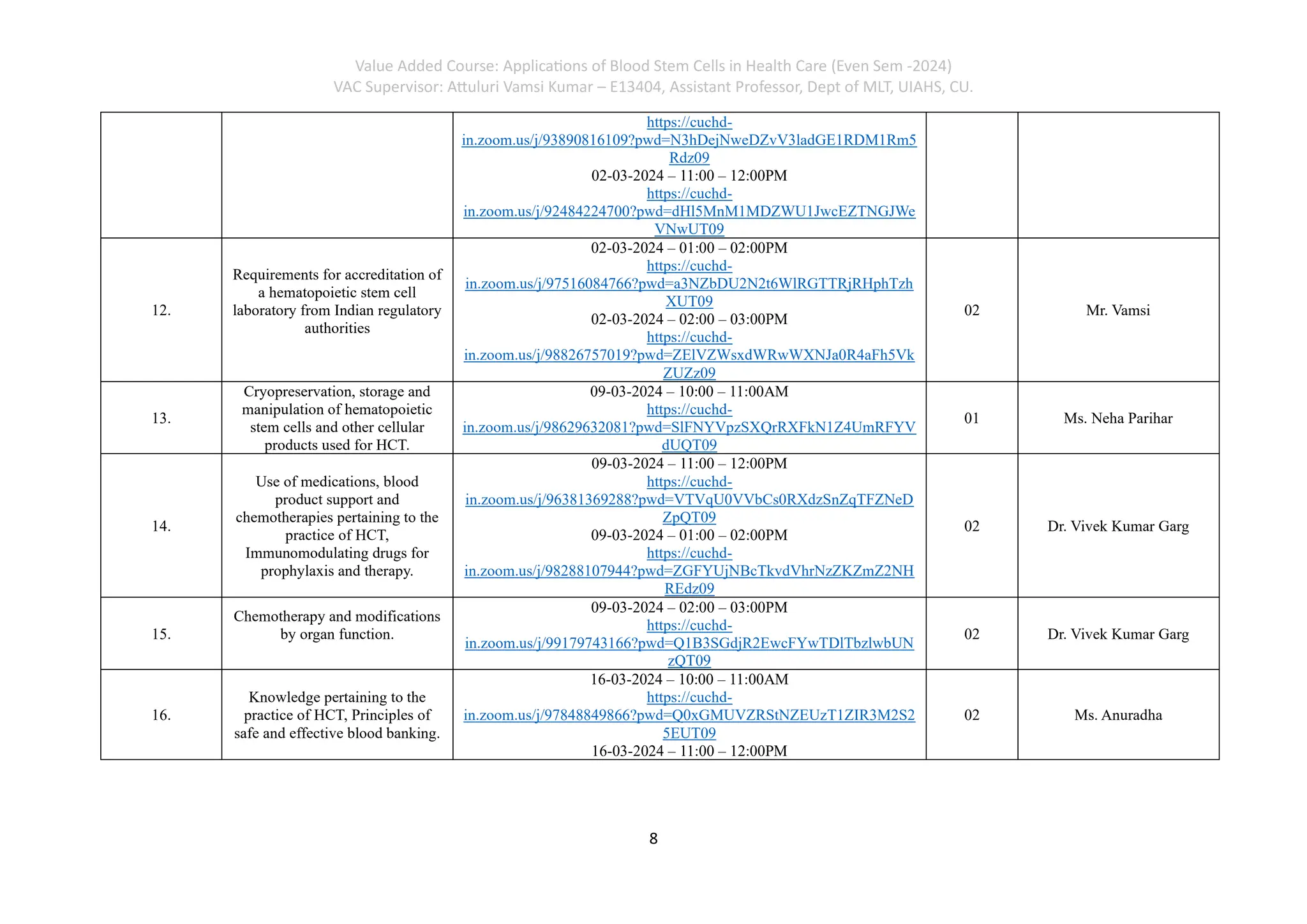
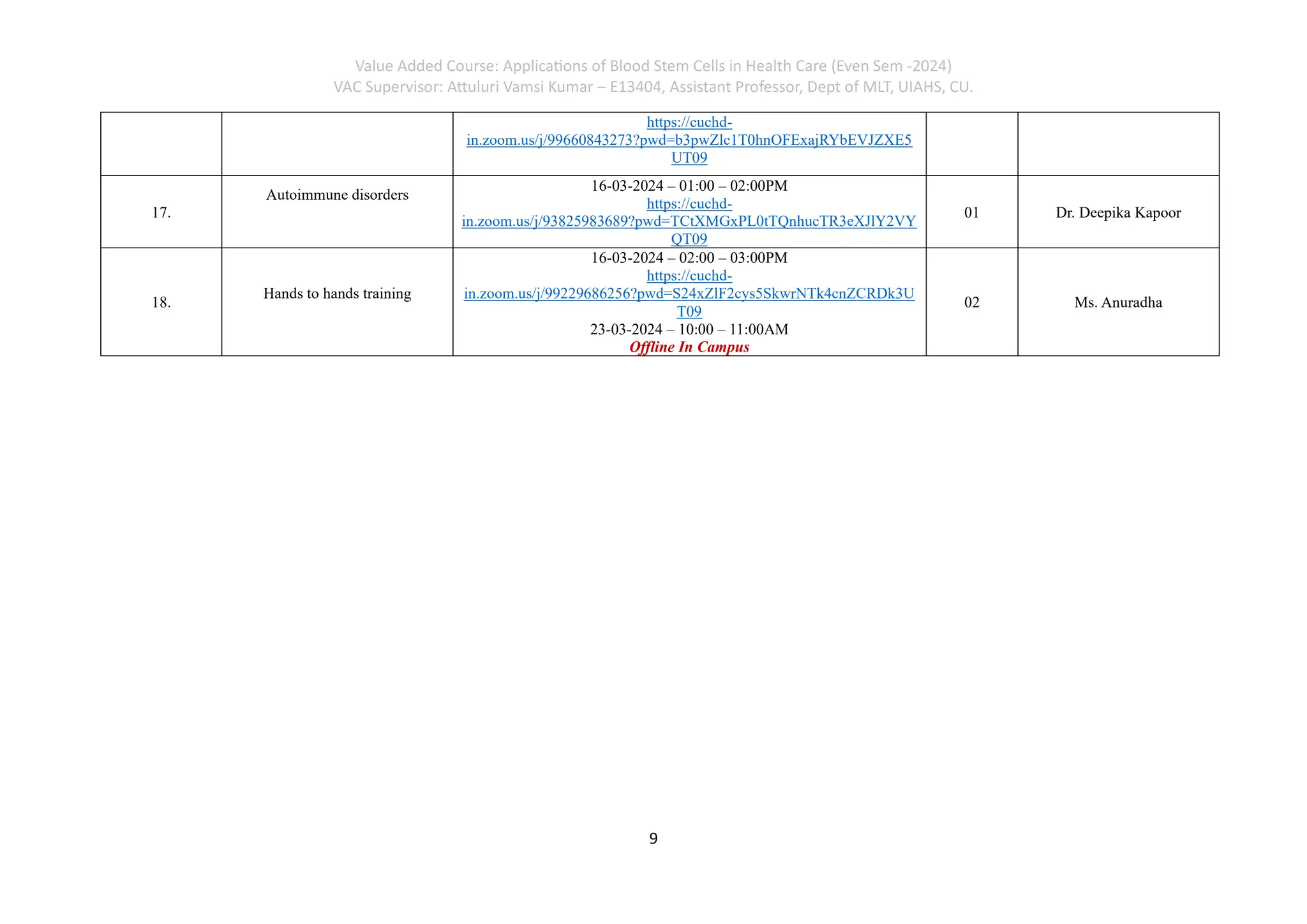
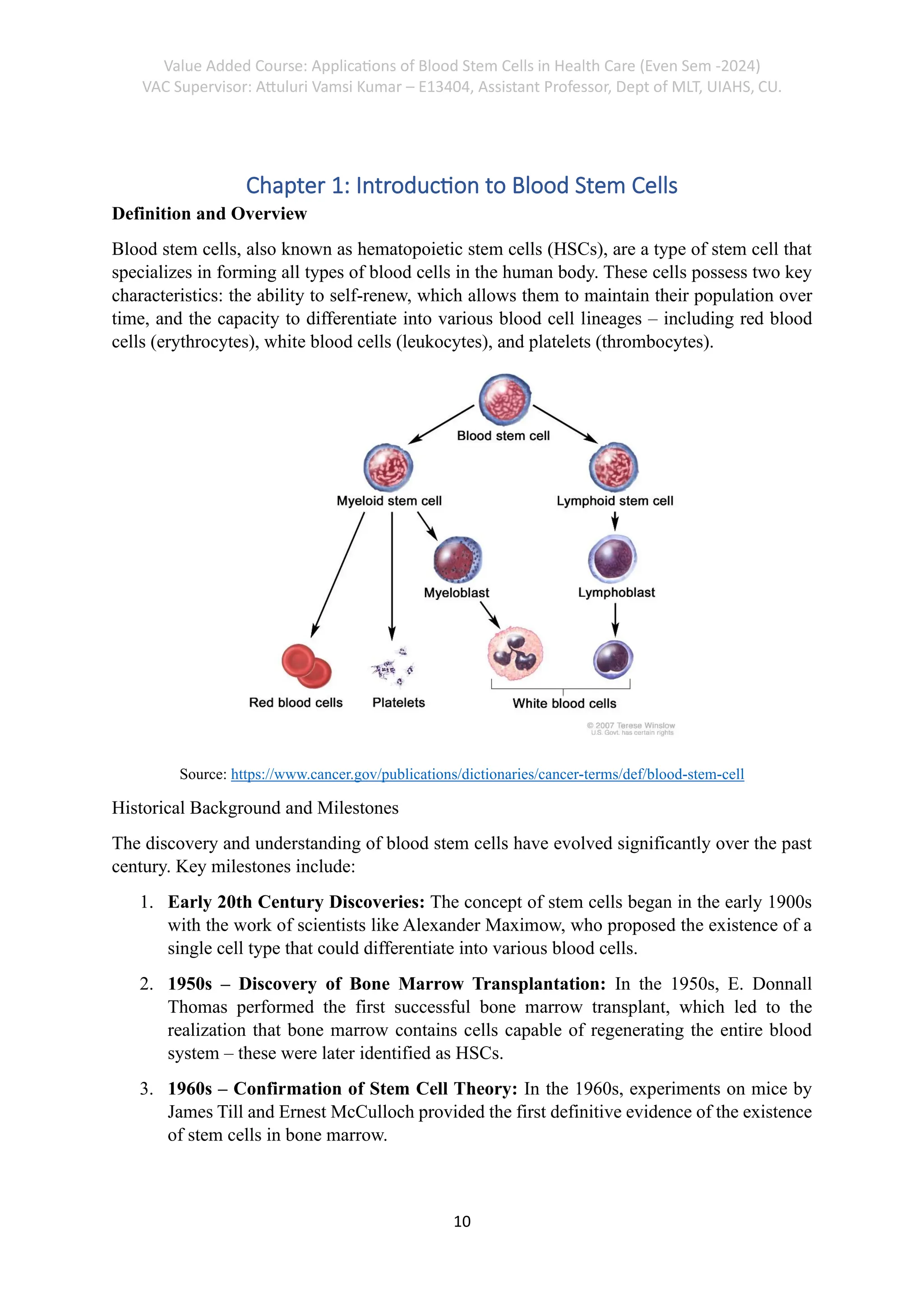
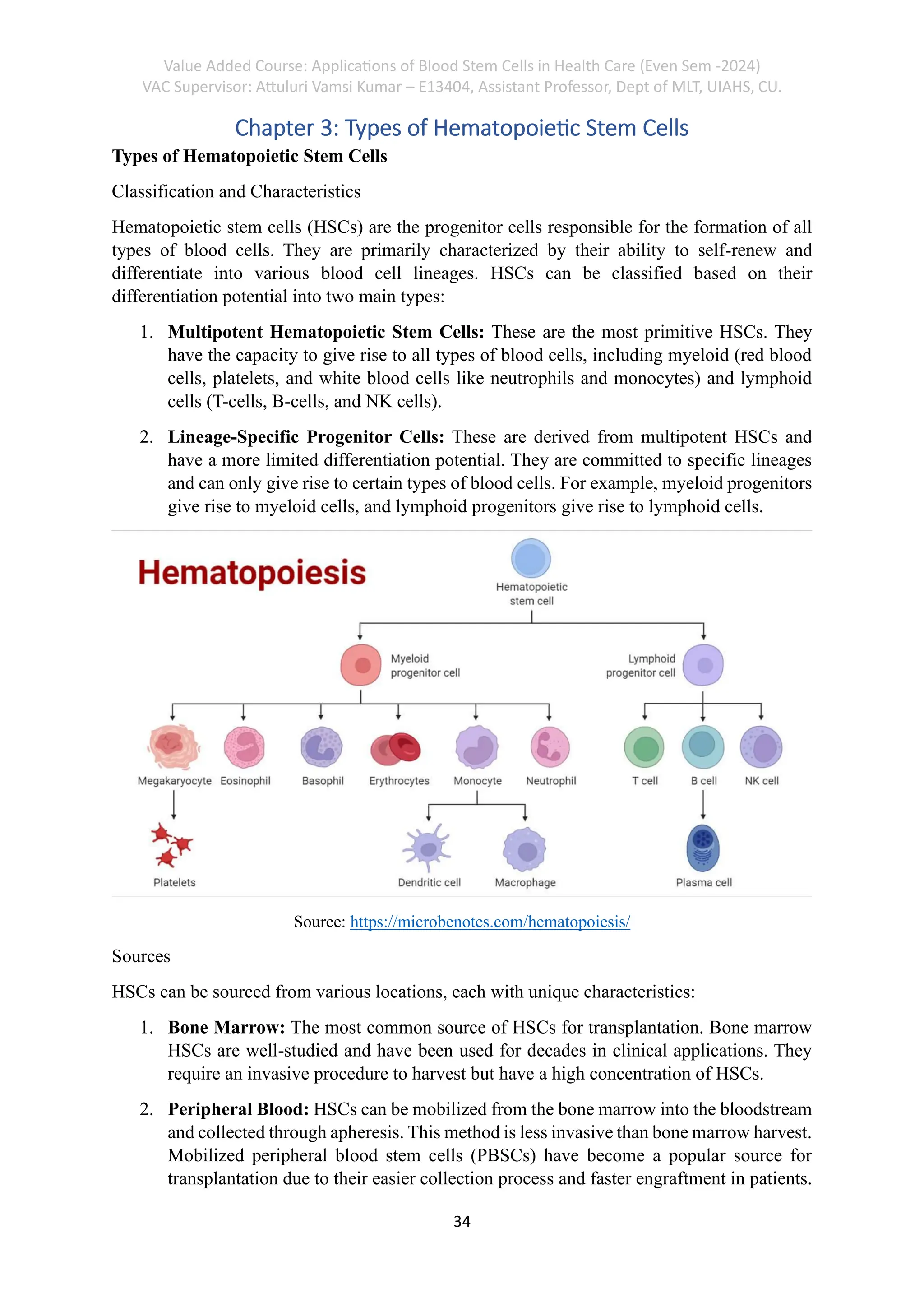
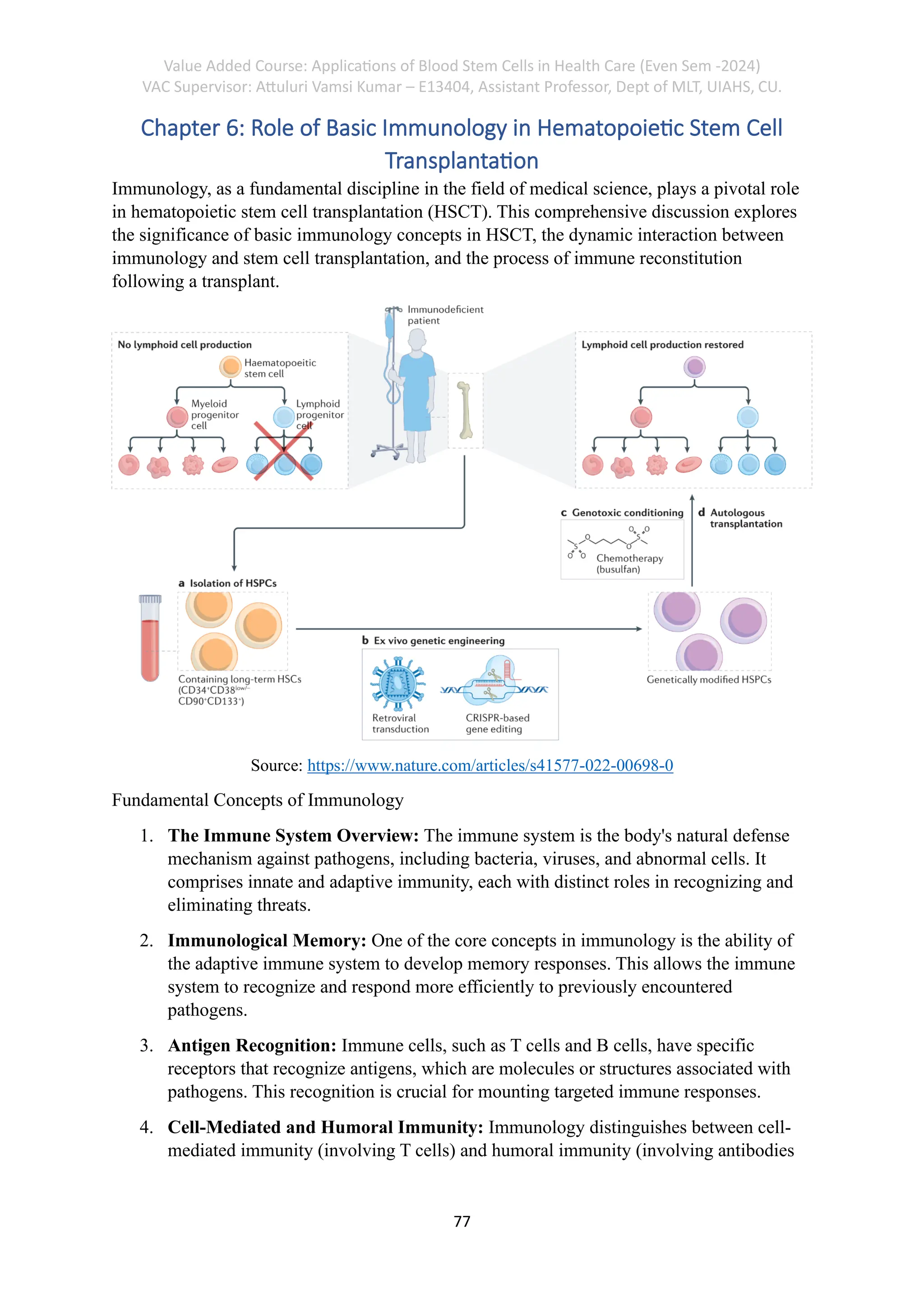
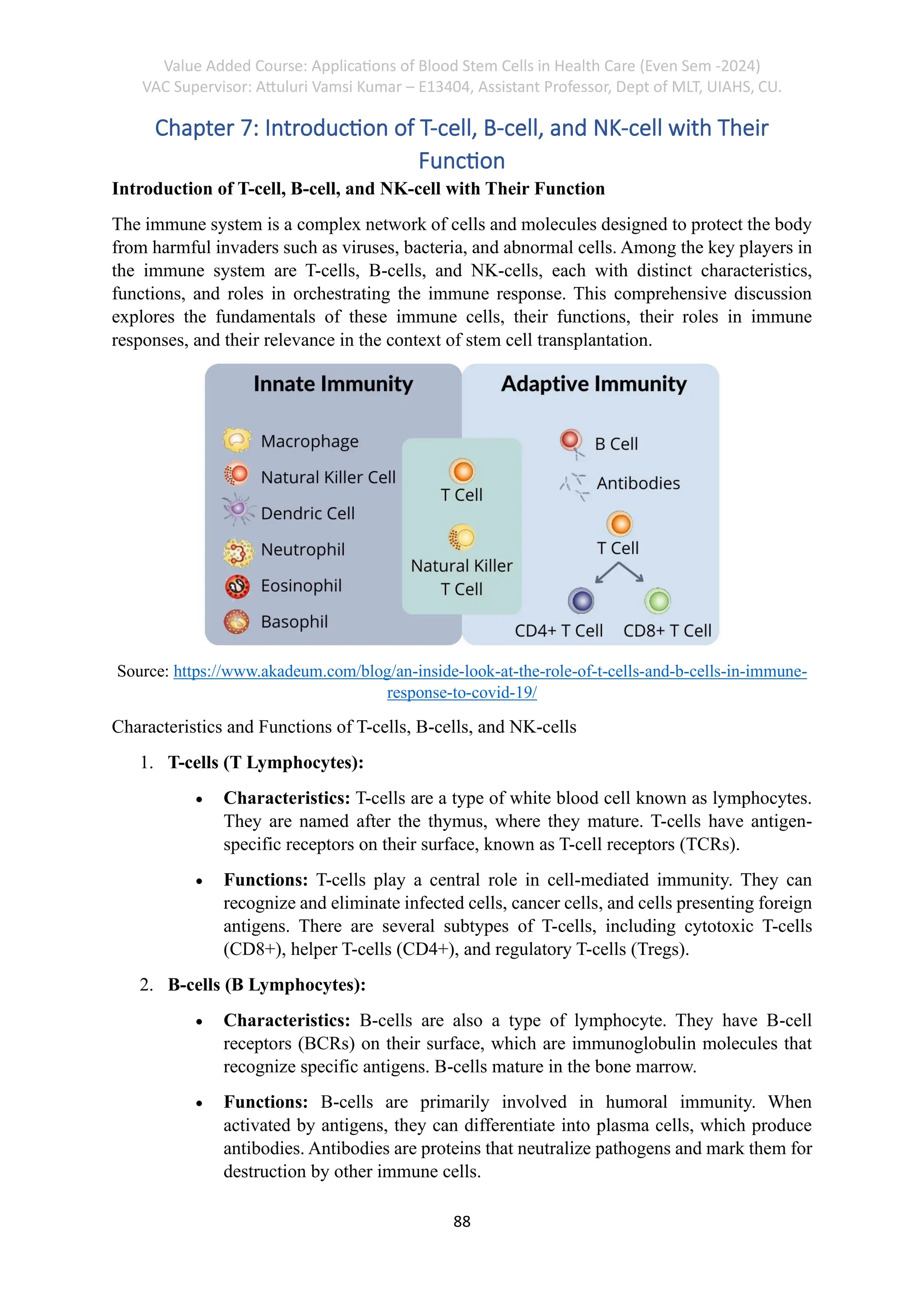
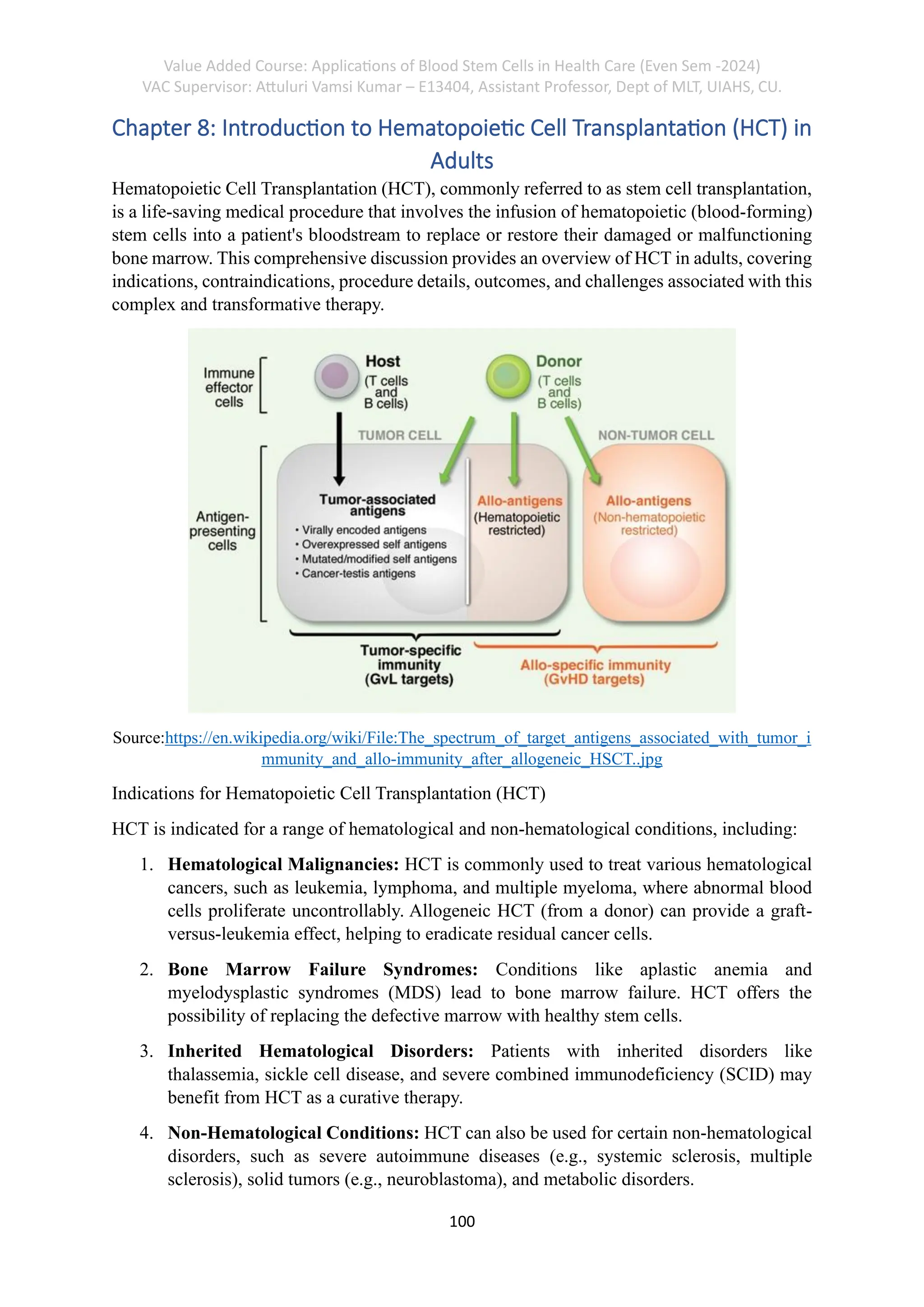
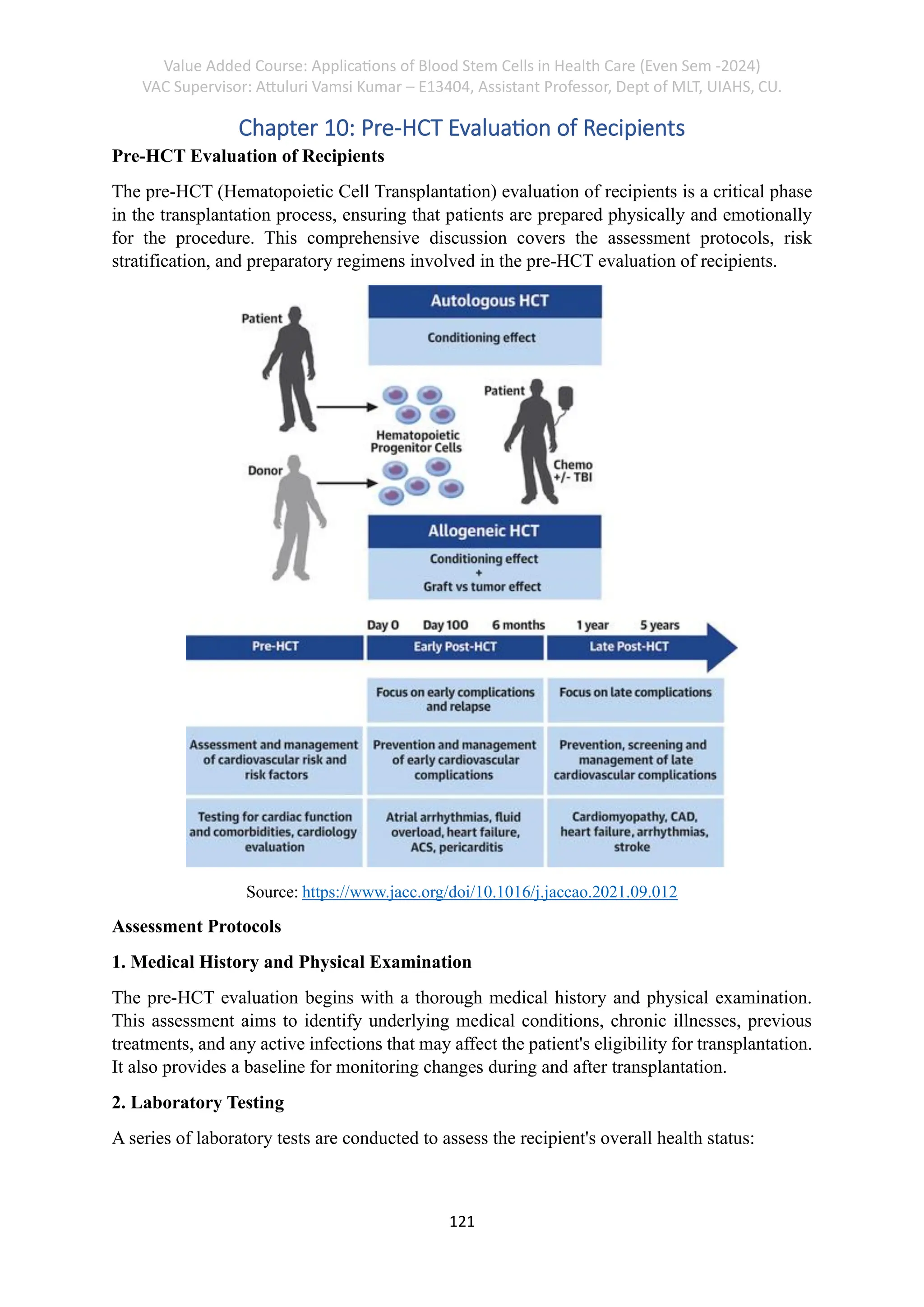
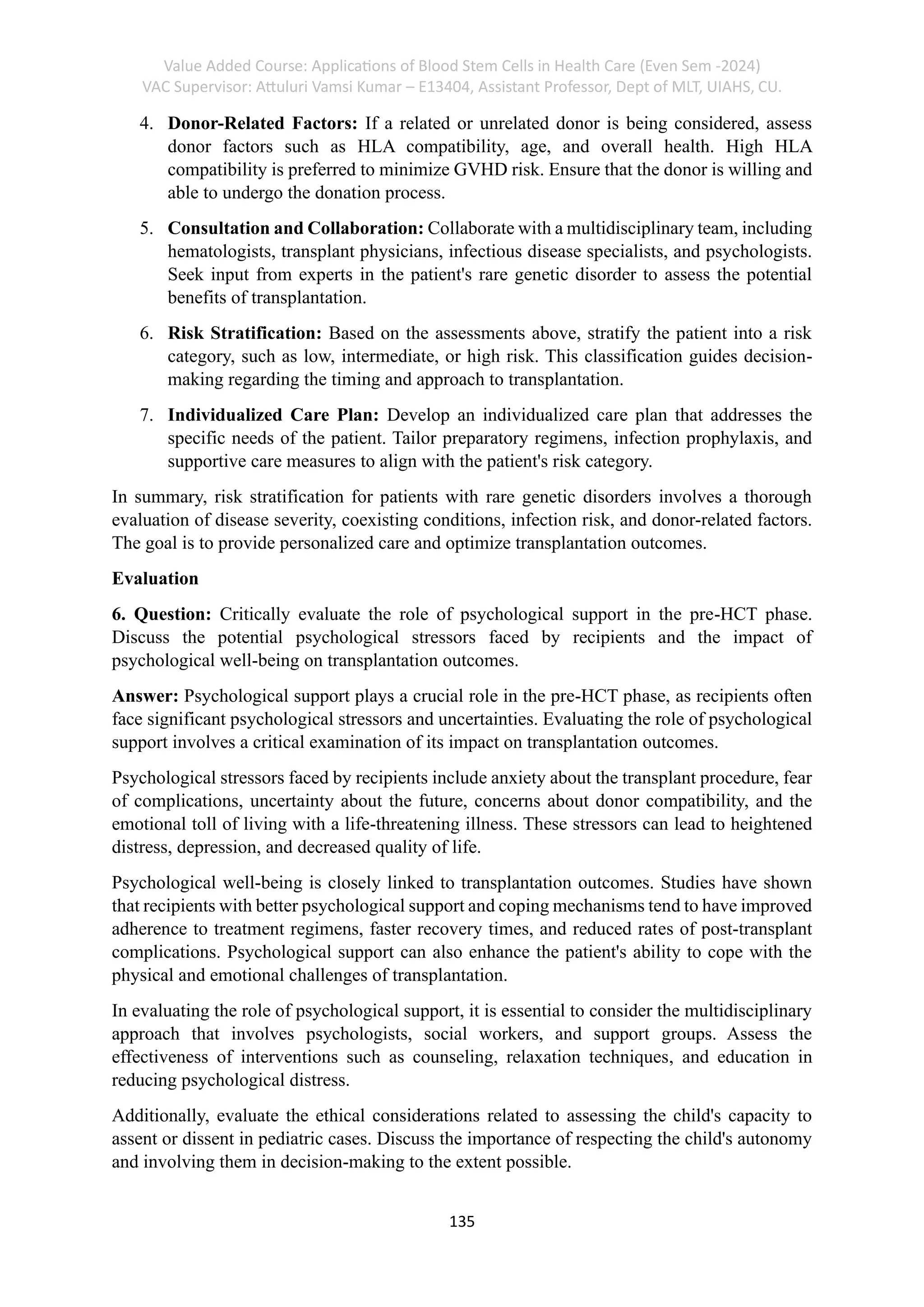
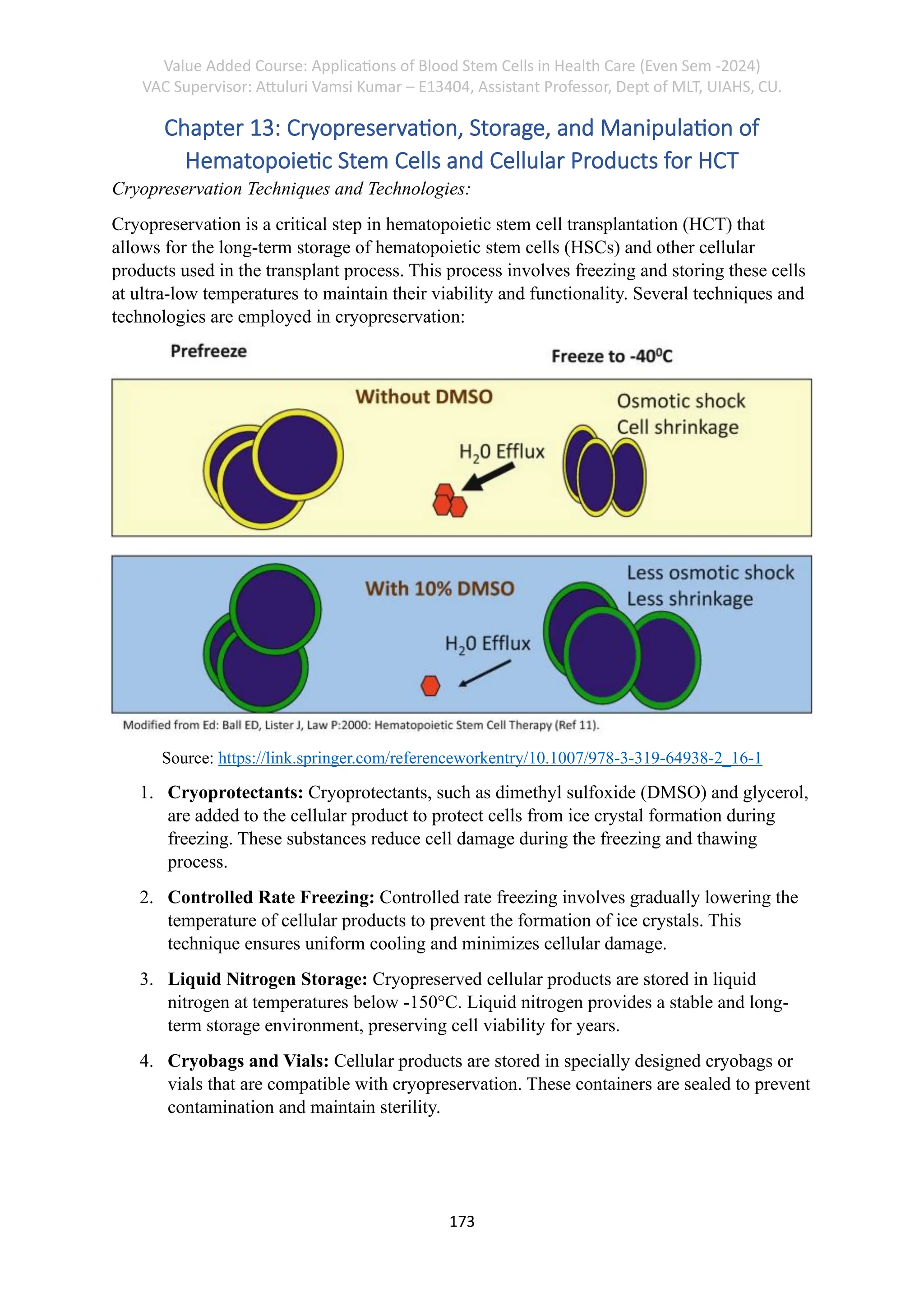
The document outlines a value-added course titled 'Applications of Blood Stem Cells in Health Care' for the even semester of 2024, supervised by Attuluri Vamsi Kumar from the Department of Medical Lab Technology. It includes comprehensive study materials, detailed outlines of lectures, and a table of contents featuring chapters on blood stem cells, hemopoiesis, and hematopoietic transplantation among others. The course covers theoretical and practical aspects, with various assessments and case studies to facilitate learning.