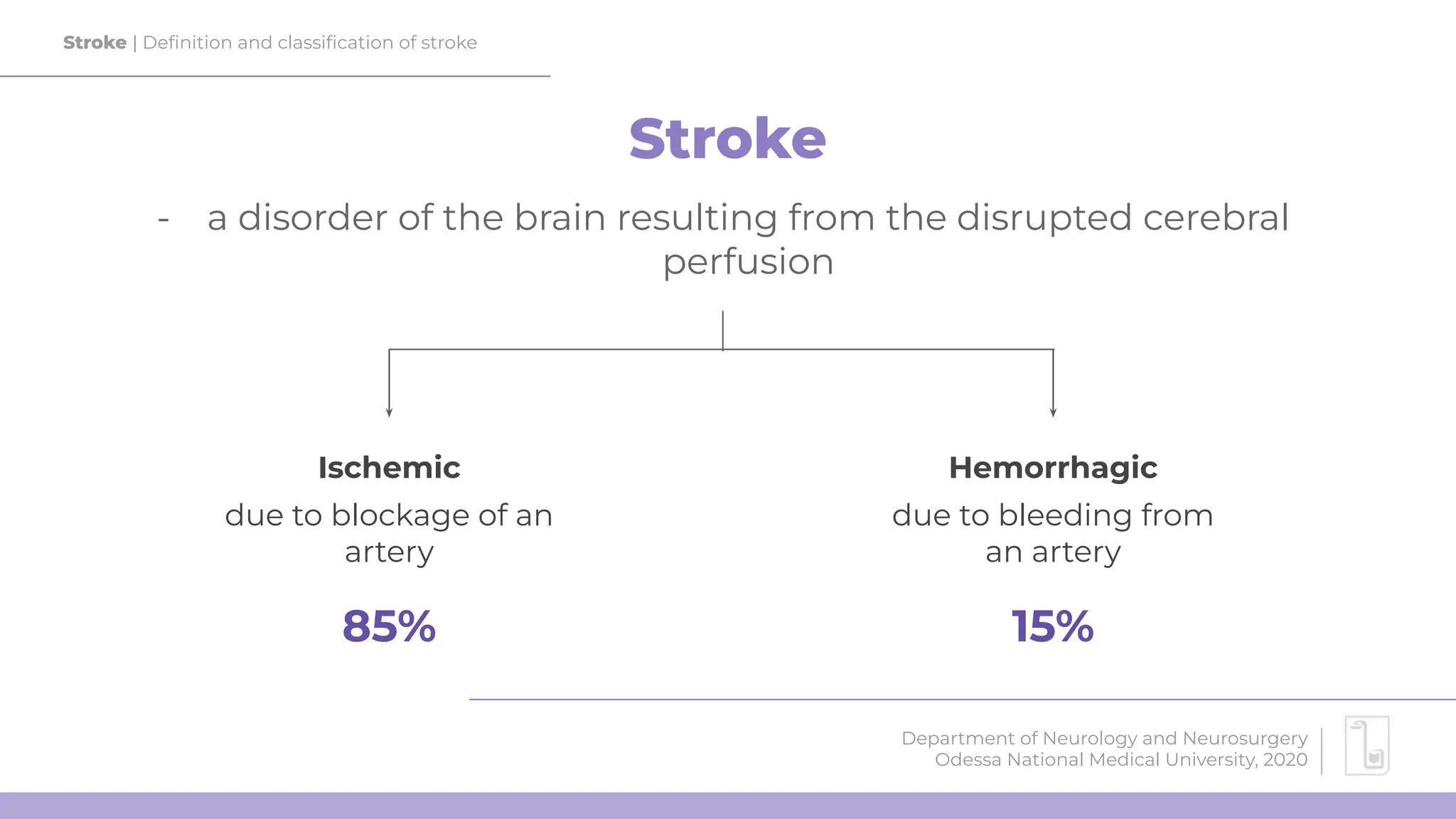
The document provides an overview of strokes, detailing the definition, classification, and risk factors associated with ischemic and hemorrhagic strokes. It discusses the urgency of treatment, the importance of diagnostics like CT scans, and the role of thrombolysis in managing stroke cases. Additionally, it highlights prevention strategies for both first-time and recurrent strokes.























![Stroke | Ischemic stroke: Treatment
Department of Neurology and Neurosurgery
Odessa National Medical University, 2020
What to do if
the time has
passed?
Source: Powers et al (2019) Guidelines for Management of AIS
Intra-arterial thrombolysis
(<6 hours)
[only MCA stroke]
Mechanical
thrombectomy (up to 24
hours)
[only large-artery stroke]](https://image.slidesharecdn.com/stroke-240714125350-c14dae8d/75/Stroke-of-different-types-Hemorrhagic-Ischemic-25-2048.jpg)








