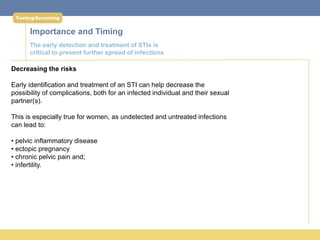
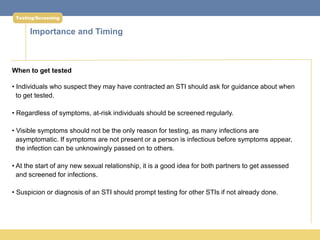
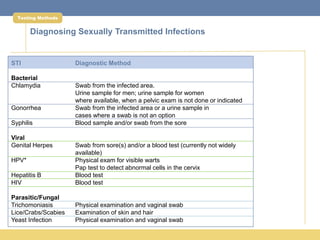
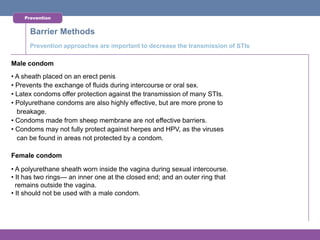
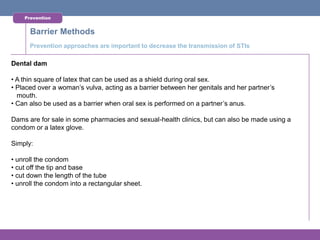
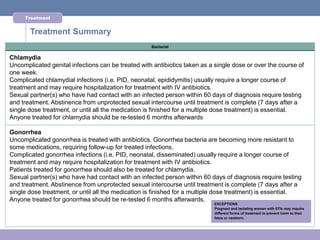
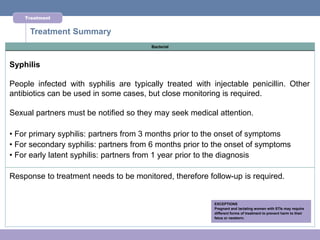
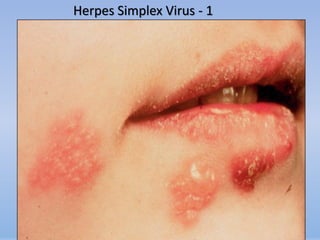
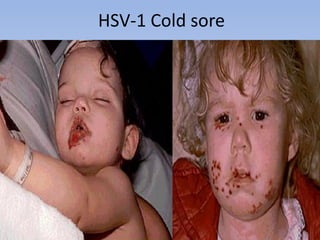
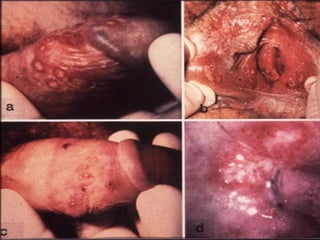
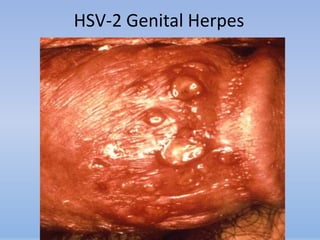
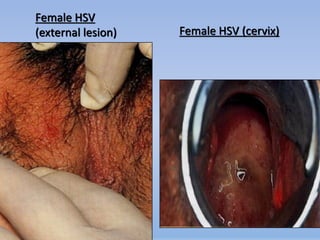
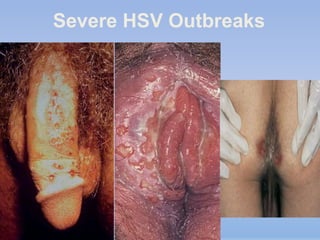
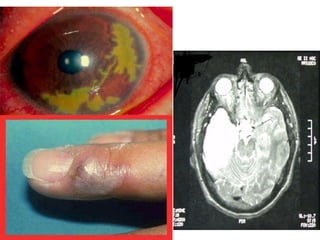
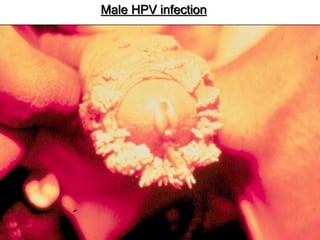
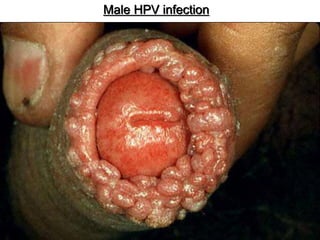
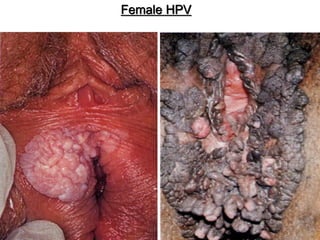
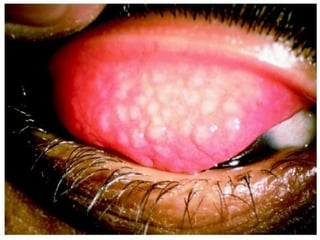
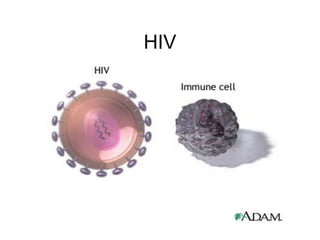
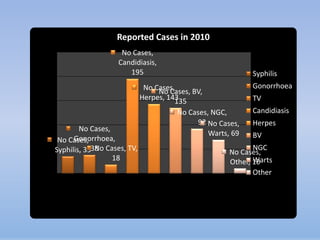
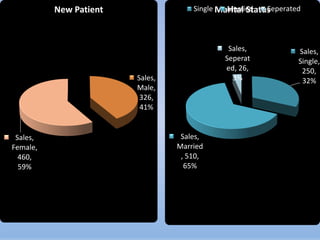
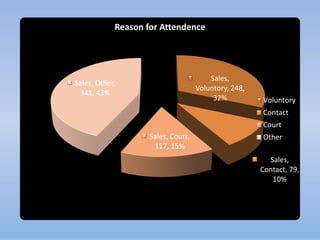
This document provides information about sexually transmitted infections (STIs). It discusses several common STIs including chlamydia, gonorrhea, genital herpes, HIV, and human papillomavirus (HPV). For each STI, it describes symptoms, prevalence rates, treatment recommendations, and risks of complications if left untreated. It emphasizes the importance of abstinence or safer sex practices, as well as getting tested and treated, to prevent the transmission of STIs.
![ffjria
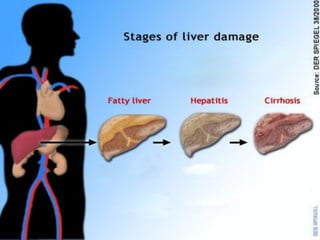
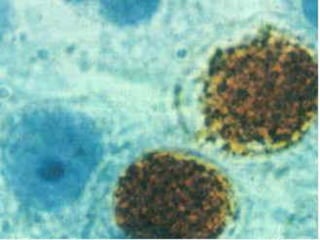
fymghsáia (Hepatitis B)
A vaccine-preventable viral infection that affects the liver
hkq
wlaudj wdidokh lrk (Hepatitis B Virus)
reêrh" YÍr ;r," ,sx.sl ;r, j," uõ lsß yd fl<j, ffjria wvx.= fõ
wdidÈ;hska 90] m%;sfoay uÕska md,kh fõ
10] ksoka.; frda.Ska njg m;a fõ
fndajk l%u
wdidÈ;hl= iu. mj;ajk wkdrÌs; ,sx.sl weiqr ^uqL$fhdak$.=o&
s
reêr mdrú,hkh $ bÈ lgq $ isßkacia
wdidÈ; ujf.ka orejdg](https://image.slidesharecdn.com/std-130403003549-phpapp01/85/Std-prensentation-26-320.jpg)