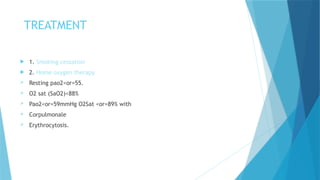
Chronic obstructive pulmonary disease (COPD) is characterized by progressive, irreversible airflow limitation, primarily caused by smoking, affecting an estimated 384 million people globally. Symptoms include excessive cough, sputum production, and shortness of breath, with exacerbations often triggered by infections or environmental factors. Diagnosis is determined through pulmonary function tests, and treatment includes smoking cessation, oxygen therapy, and medications such as corticosteroids and theophylline.



![Risk factors
Cigarette smoking is clearly the most important cause of COPD . It is
estimated that 80% of patients seen for COPD have significant exposure to
tobacco smoke.
The remaining 20% frequently have a combination of exposures to
environmental tobacco smoke, occupational dusts and chemicals, and indoor
air pollution from biomass fuel used for cooking and heating in poorly
ventilated buildings.
Outdoor air pollution, airway infection, familial factors, and allergy have also
been implicated in chronic bronchitis, and hereditary factors (deficiency of
alpha-1-antiprotease [alpha-1-antitrypsin]) have been implicated](https://image.slidesharecdn.com/random-250201193757-71e32b93/85/slide-4-320.jpg)