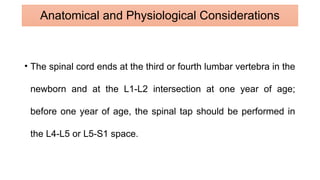
Spinal anesthesia (SA) has been utilized in pediatric patients since 1899, particularly in high-risk infants to minimize respiratory complications following surgery. The document discusses various anatomical and physiological factors influencing spinal anesthesia in young patients, contraindications, potential complications, and the efficacy compared to general anesthesia (GA). It concludes that while SA may reduce hospital stay duration, careful consideration of technique and additional sedation agents, such as dexmedetomidine, is crucial for safety and effectiveness.
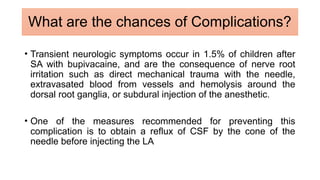
![• Epidemiological data suggest that infants have an increased
risk of complications with GA compared to older children and
adults.
• 102 vs 128 pts were compared.
• The hospital length of stay was shorter in the spinal anesthesia
group (median [IQR] of 5.3 hours [4.3, 7.2]) compared to the
general anesthesia group (17.1 hours [15.6, 17.5])
SAB vs GA](https://image.slidesharecdn.com/spinalanaesthinpeds-240812063647-bf9ef422/85/Spinal-Anaesthesia-in-Pediatric-Pateints-pptx-12-320.jpg)