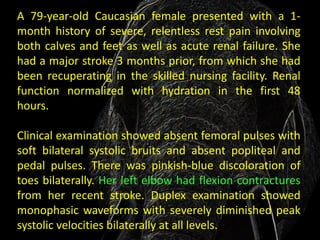
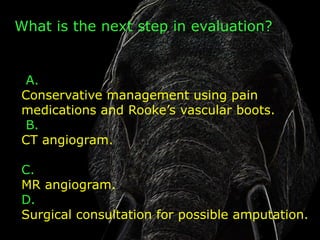
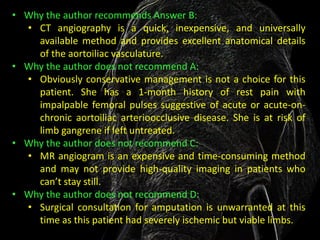
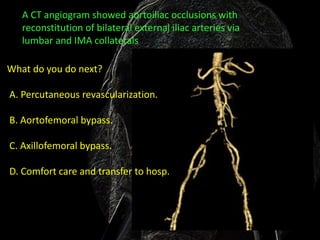
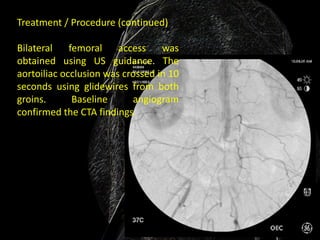
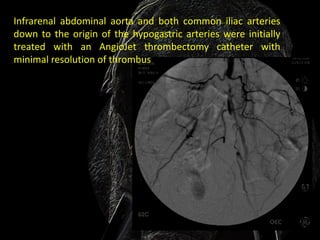
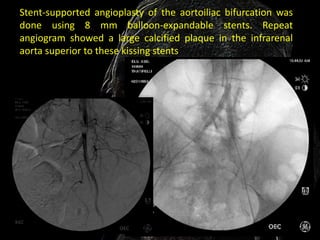
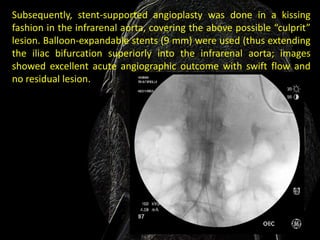
A 79-year-old woman presented with severe leg pain and acute renal failure. Examination showed absent leg pulses. Imaging showed aortoiliac occlusions. The next step was a CT angiogram, which confirmed aortoiliac occlusions. Percutaneous revascularization was then performed by obtaining femoral access and crossing the occlusion with guidewires. Angioplasty and stenting of the aortoiliac bifurcation and infrarenal aorta were performed, resulting in excellent blood flow.