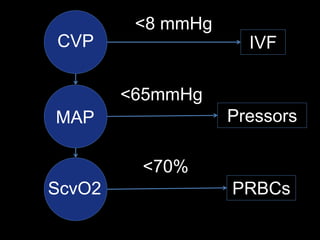
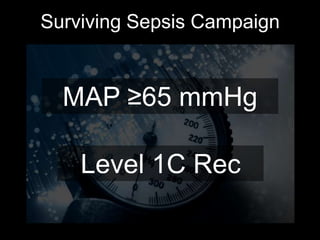
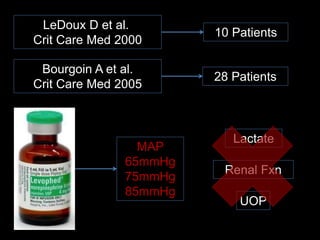
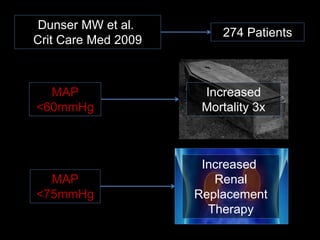
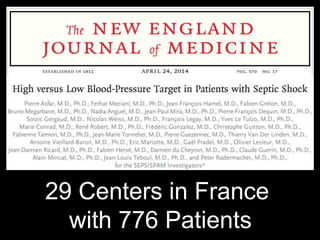
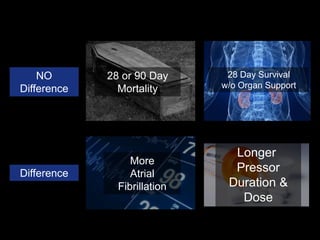
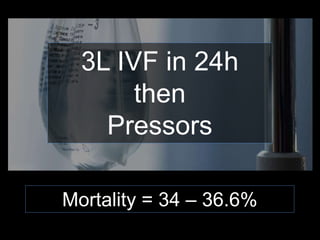
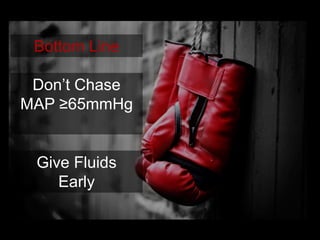
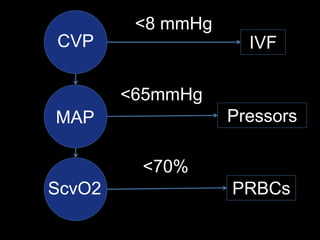
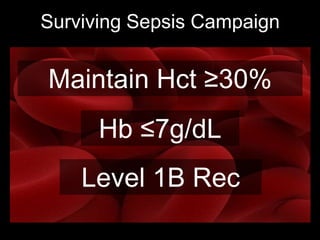
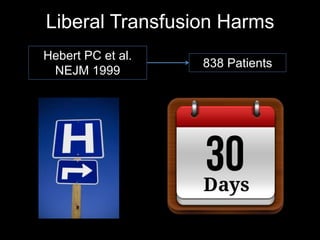
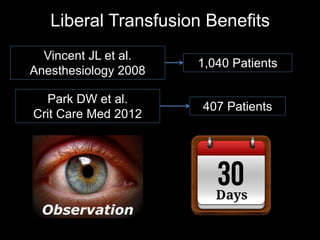
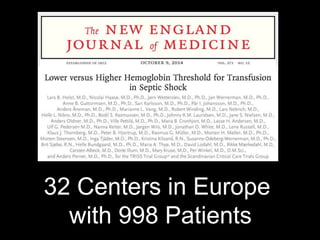
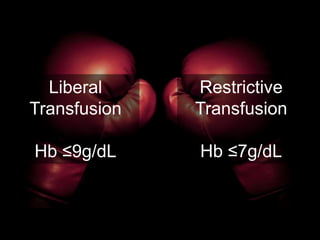
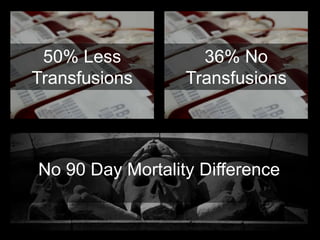
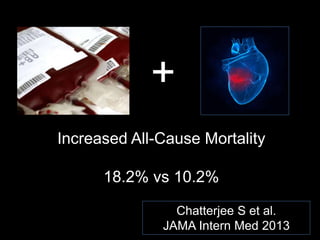
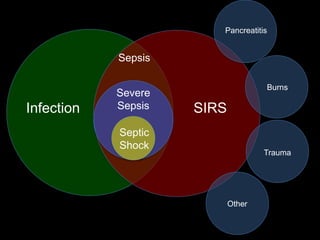
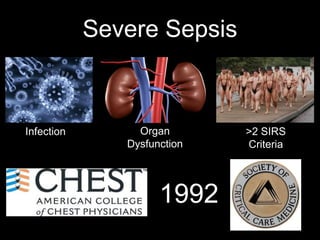
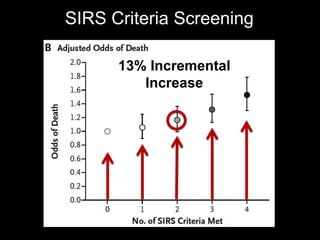
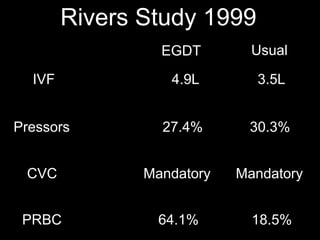
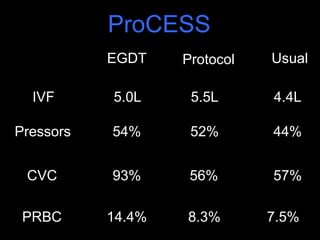
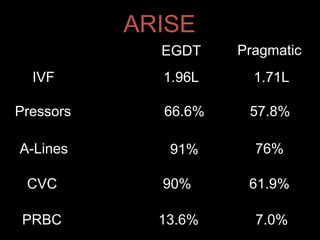
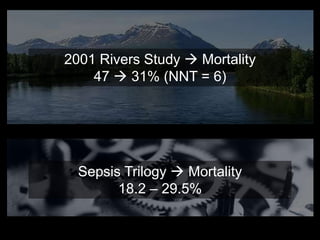
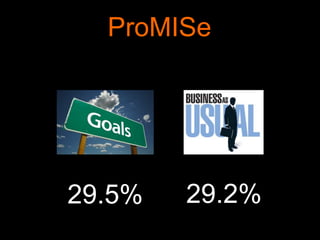
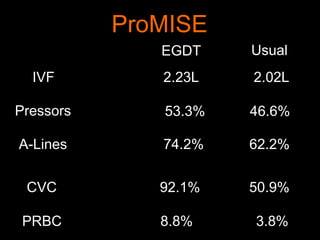
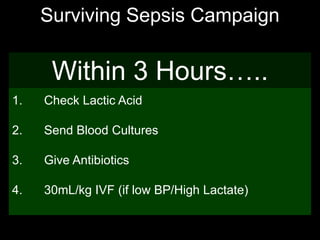
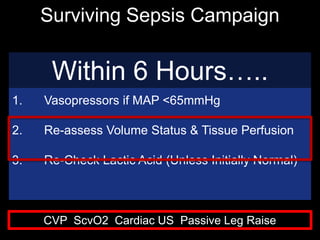
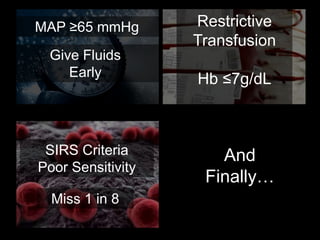
The document discusses updates on sepsis care protocols, including blood pressure targets, transfusion strategies, and the effectiveness of the Surviving Sepsis Campaign guidelines. Key findings suggest that early fluid administration and a restrictive transfusion strategy are beneficial, while SIRS criteria are not sufficiently sensitive for detecting severe sepsis. Additionally, recent trials show no mortality benefits from enhanced goal-directed therapy compared to usual care practices.