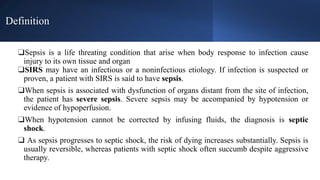
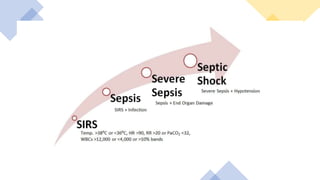
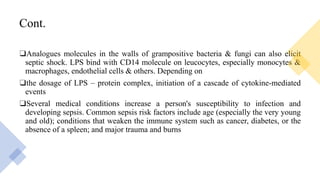
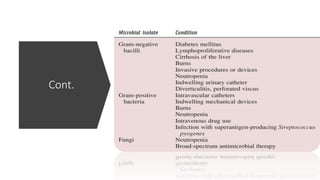
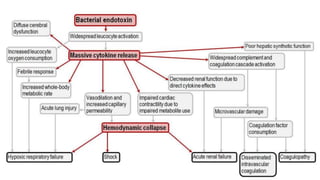
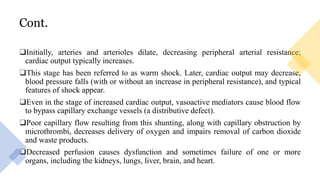
Sepsis is a life-threatening condition caused by the body's response to infection leading to organ and tissue damage; it can progress to severe sepsis and septic shock, which have high mortality rates and require prompt diagnosis and treatment. Key risk factors include age, immunocompromising conditions, and major trauma, with millions affected each year, especially in hospitalized patients. Management involves early administration of antibiotics, intravenous fluids, and supportive care, with the 'sepsis six' bundle of interventions highlighted for effective treatment.