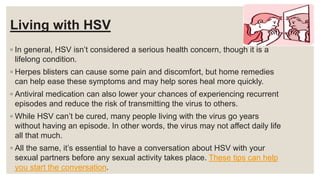
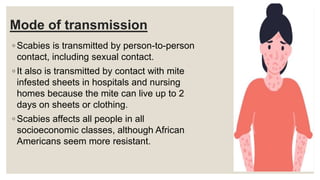
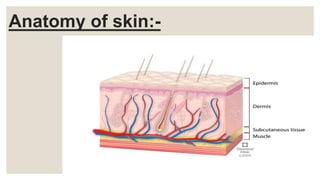
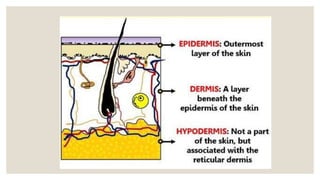
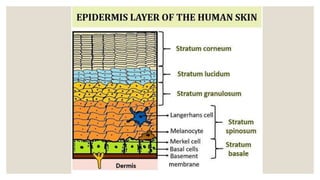
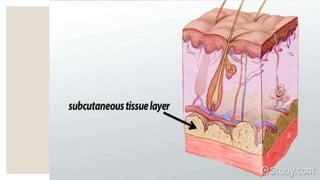
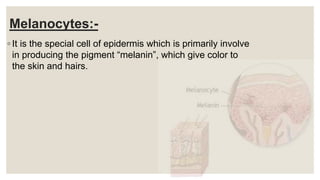
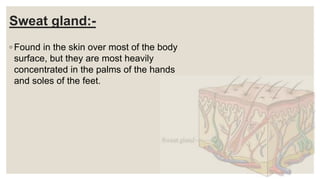
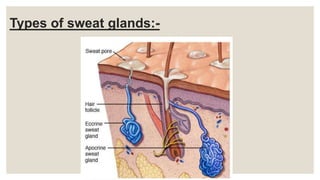
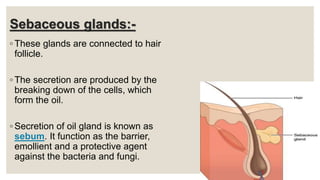
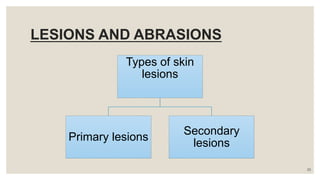
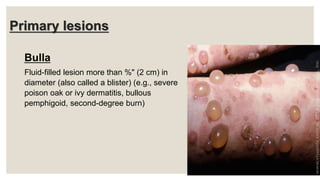
1. The document discusses the integumentary system, specifically focusing on the anatomy and physiology of the skin. It describes the layers of the skin (epidermis, dermis, hypodermis) and structures within each layer.
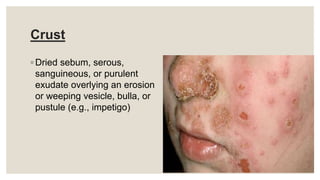
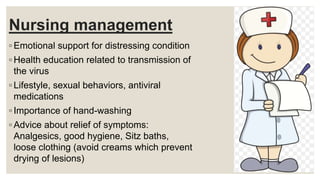
2. Key functions of the skin are outlined, including forming a protective barrier, regulating temperature, protecting from pathogens, and providing sensory input. Common skin glands, cells, and lesions are defined.
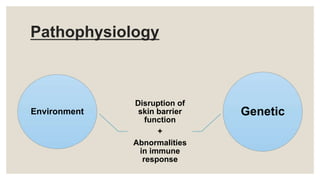
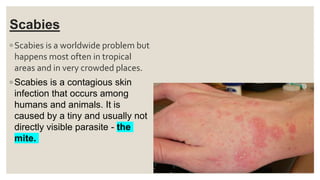
3. The presentation also examines atopic dermatitis in more depth, covering causes, pathophysiology, signs/symptoms, diagnostic evaluation, and management strategies like eliminating allergens and applying topical corticosteroids.
![VIVEKANANDA COLLEGE OF NURSING
Seminar
PRESENTED BY:- APURVA DWIVEDI [M.Sc. Nursing 1ST Yr.]](https://image.slidesharecdn.com/seminarintegumetrysystem-220717101125-f4d9c4b7/85/Seminar-integumetry-system-pptx-1-320.jpg)

![Comedo
Plugged pilosebaceous duct,
exfoliative, formed from sebum
and keratin (e.g., blackhead
[open comedo], whitehead
[closed comedo])](https://image.slidesharecdn.com/seminarintegumetrysystem-220717101125-f4d9c4b7/85/Seminar-integumetry-system-pptx-25-320.jpg)

![Patch
◦ Flat, pigmented, circumscribed
area more than " (1 cm) in
diameter (e.g.; Herald patch
[pityriasis rosea])](https://image.slidesharecdn.com/seminarintegumetrysystem-220717101125-f4d9c4b7/85/Seminar-integumetry-system-pptx-30-320.jpg)


![Wheal
◦ Raised, firm lesion with intense
localized skin edema, varying in
size and shape; color ranging from
pale pink to red, disappears in
hours (e.g., hive [urticaria], insect
bite)](https://image.slidesharecdn.com/seminarintegumetrysystem-220717101125-f4d9c4b7/85/Seminar-integumetry-system-pptx-35-320.jpg)

![Fissure
◦ Linear cracking of the skin
extending into the dermal layer
(e.g.; hand dermatitis [chapped
skin]).](https://image.slidesharecdn.com/seminarintegumetrysystem-220717101125-f4d9c4b7/85/Seminar-integumetry-system-pptx-38-320.jpg)