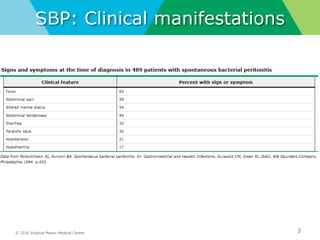
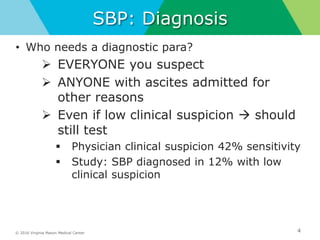
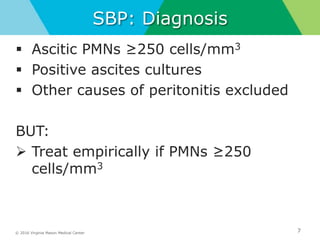
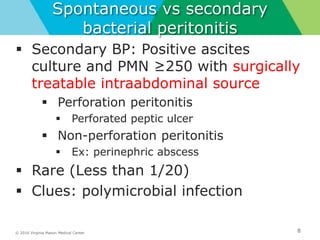
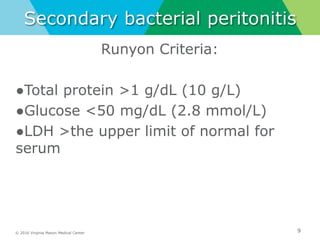
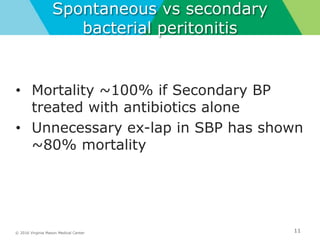
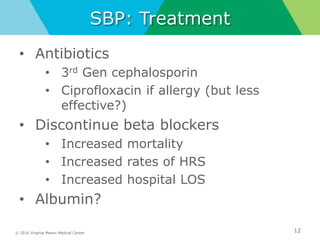
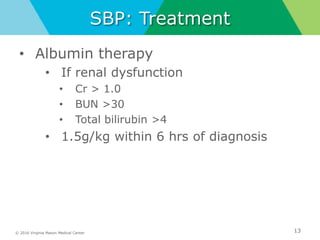
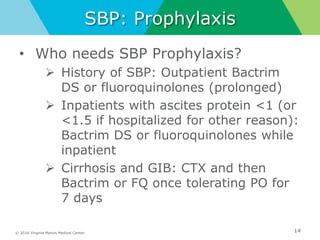
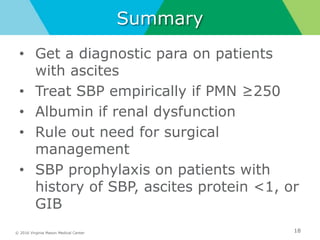
This document discusses spontaneous bacterial peritonitis (SBP). It recommends that a diagnostic paracentesis be performed on all patients with ascites to test for SBP. SBP should be treated empirically if the ascitic fluid polymorphonuclear leukocyte count is ≥250 cells/mm3. Albumin therapy is recommended for SBP patients with renal dysfunction. The document differentiates between spontaneous and secondary SBP, noting that secondary SBP requires surgical management. It also provides guidance on SBP prophylaxis.