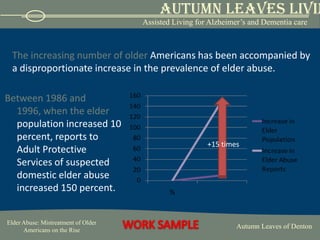
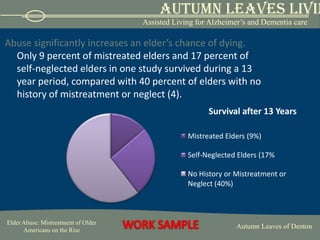
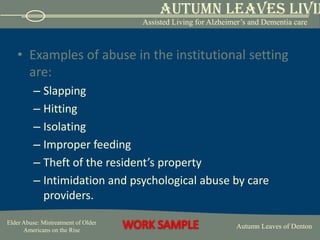
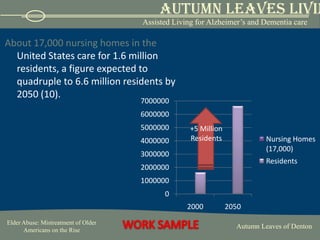
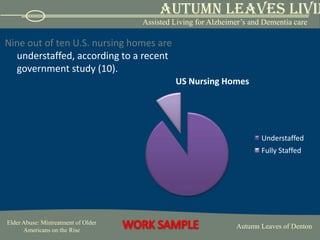
Elder abuse is on the rise as the population of older Americans grows. There are four main types of elder abuse: physical, psychological, financial, and neglect. Nurses can help prevent abuse by being alert for signs of mistreatment, assessing patients privately for injuries, and reporting any suspected abuse to authorities. They should also provide resources to caregivers to help relieve stress that could lead to domestic abuse. In institutional settings, increased nursing staff levels are associated with fewer violations, so legislation aims to establish minimum staffing standards.