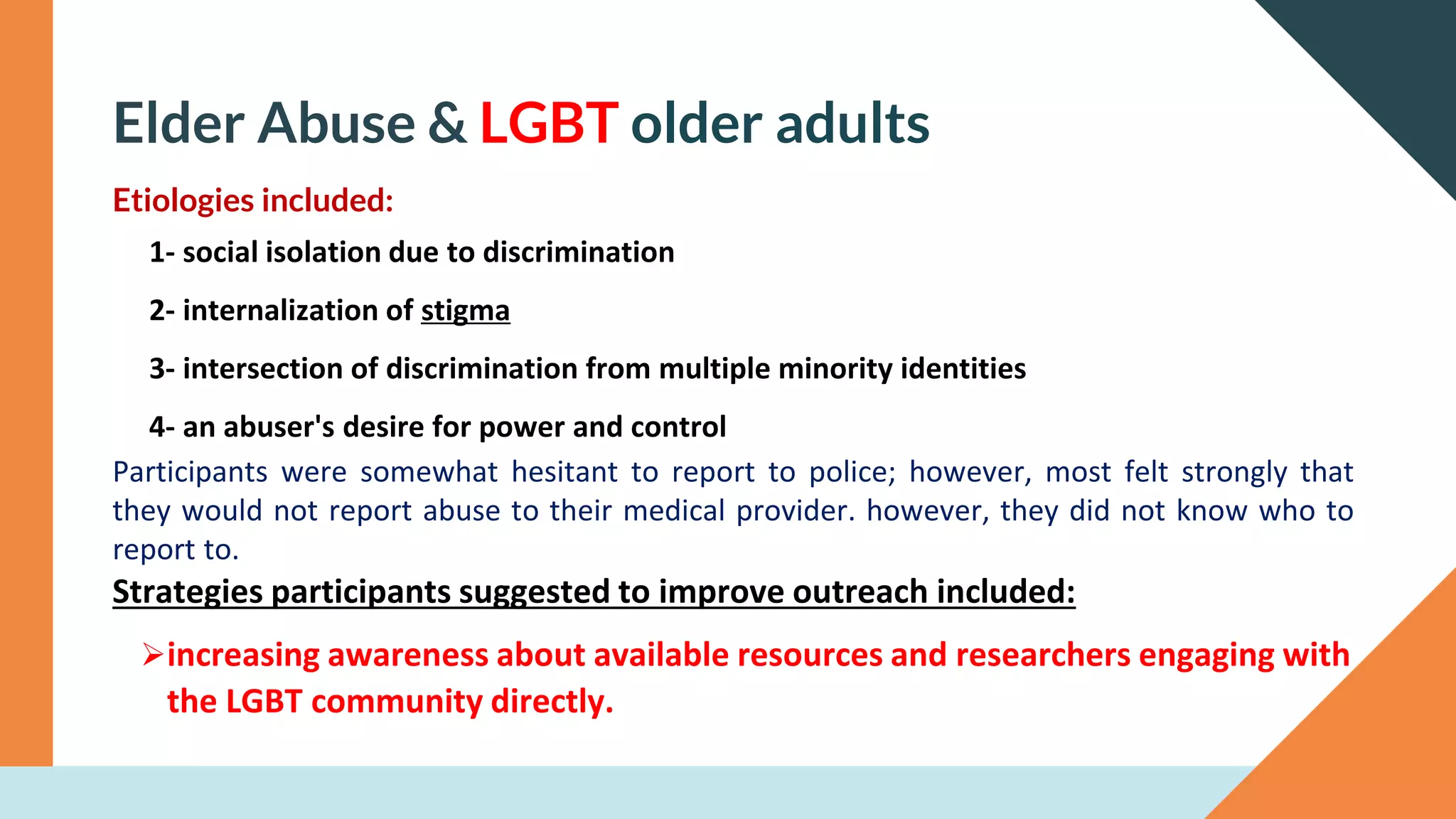
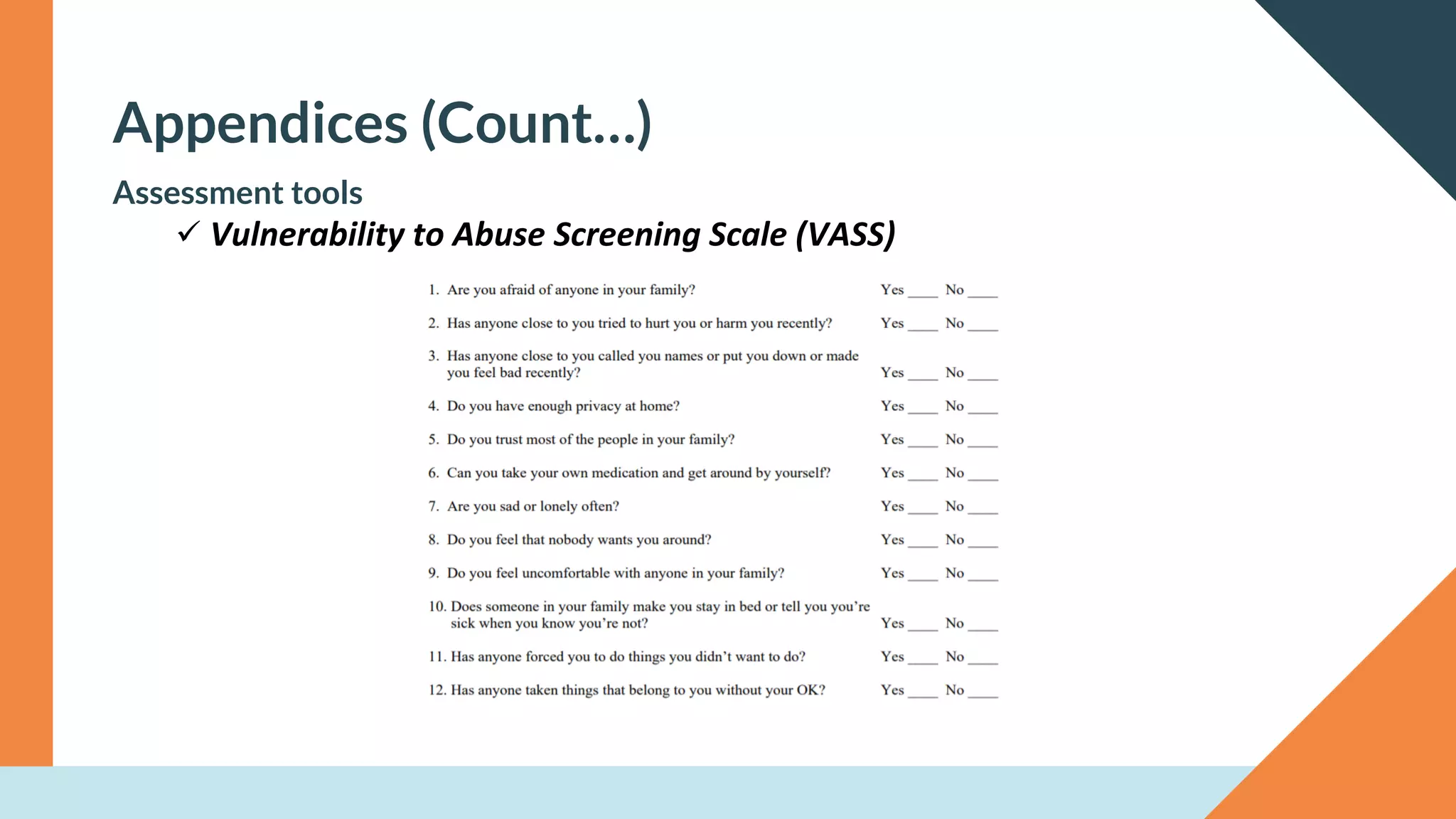
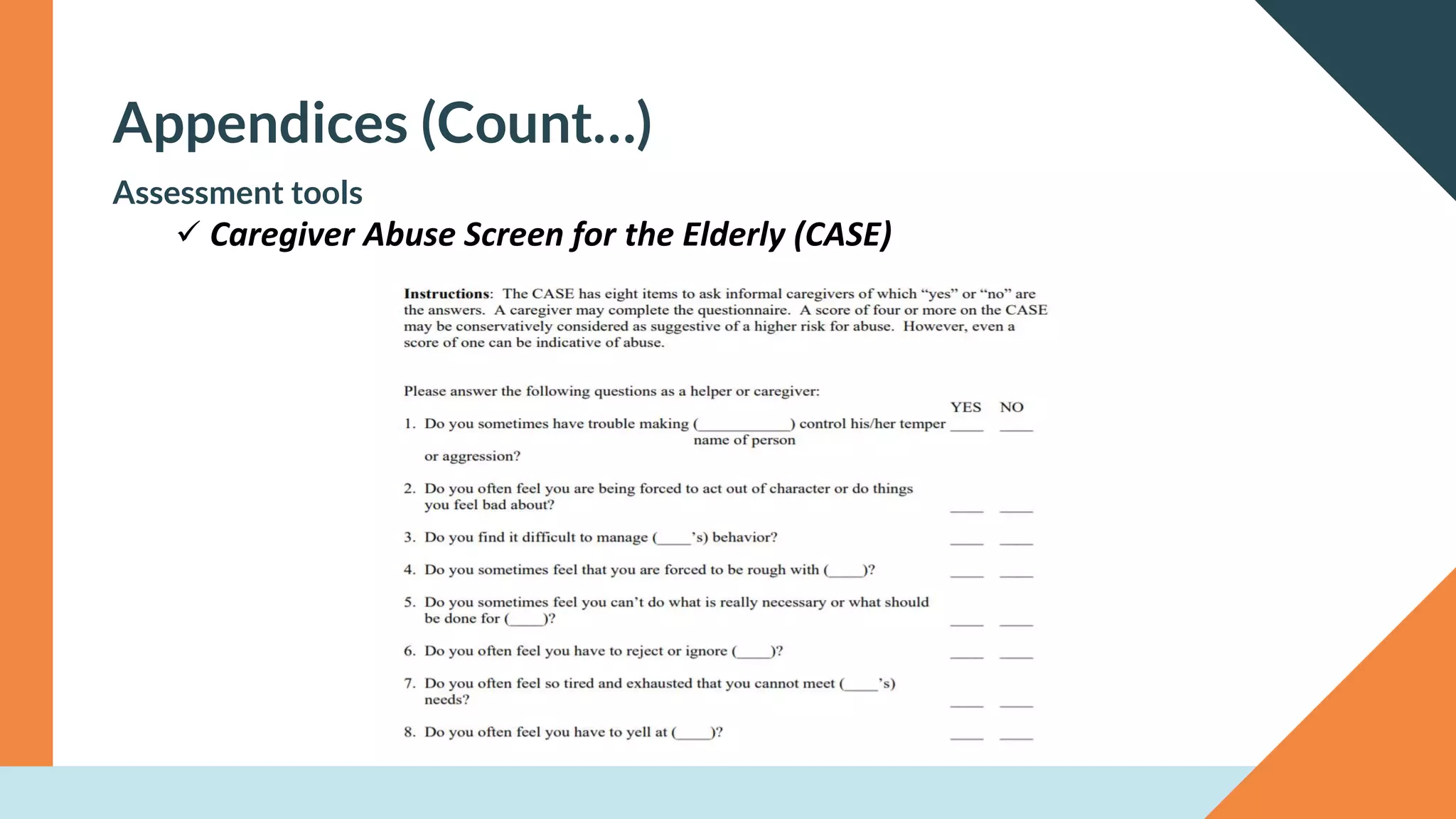
This document provides an overview of elder abuse. It discusses risk factors for elder abuse including caregiver stress and the elder's level of dependency. The main types of elder abuse are physical, psychological, sexual, financial, and neglect. Signs of abuse include unexplained bruises or injuries, poor hygiene, and inconsistent stories from the elder and caregiver. Nurses should assess for abuse and document and report any suspicions. Preventing abuse involves educating families, providing support services, and encouraging self-care among caregivers. During COVID-19, risks increased due to elders' greater social isolation and dependency on others.