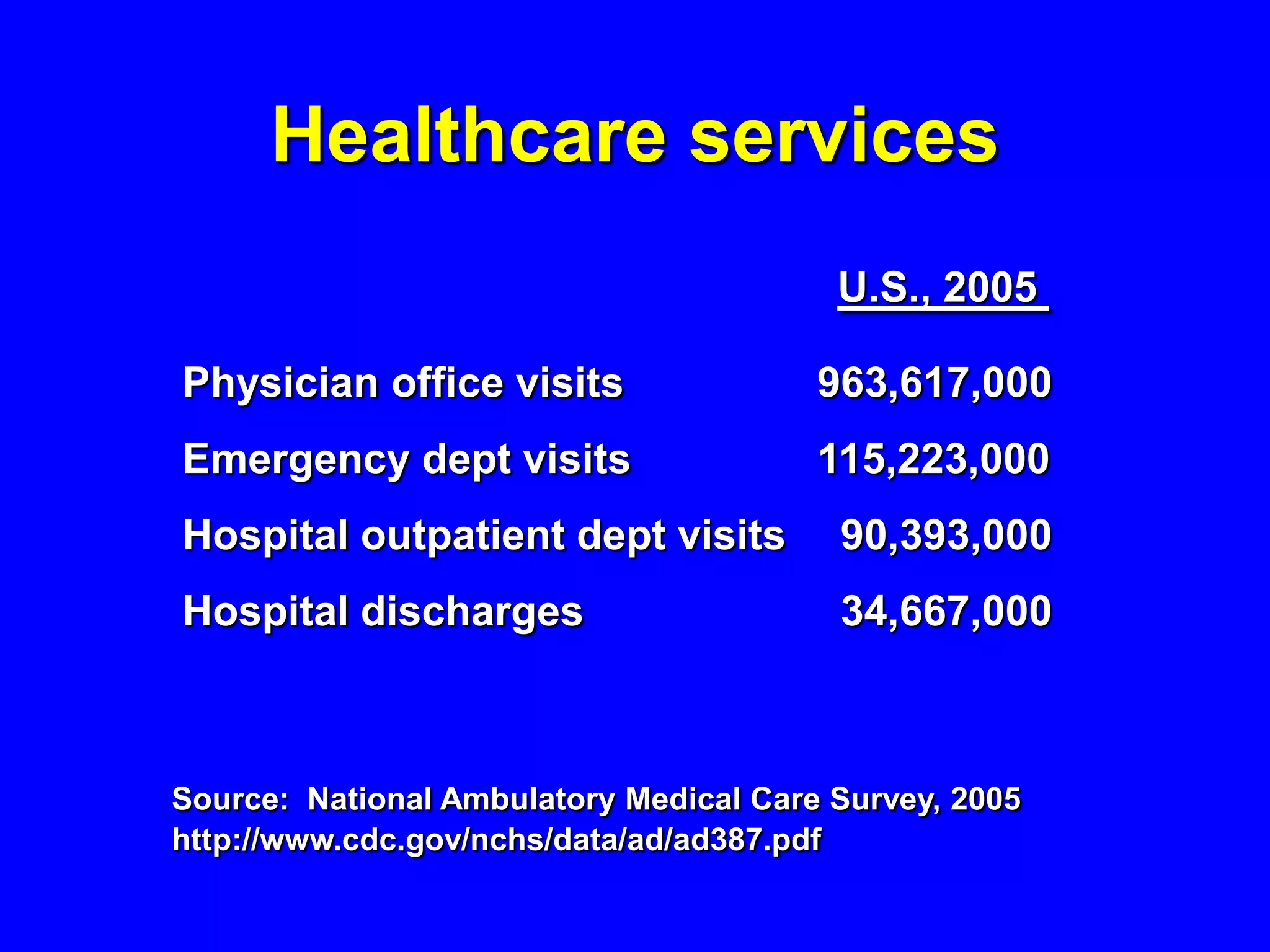
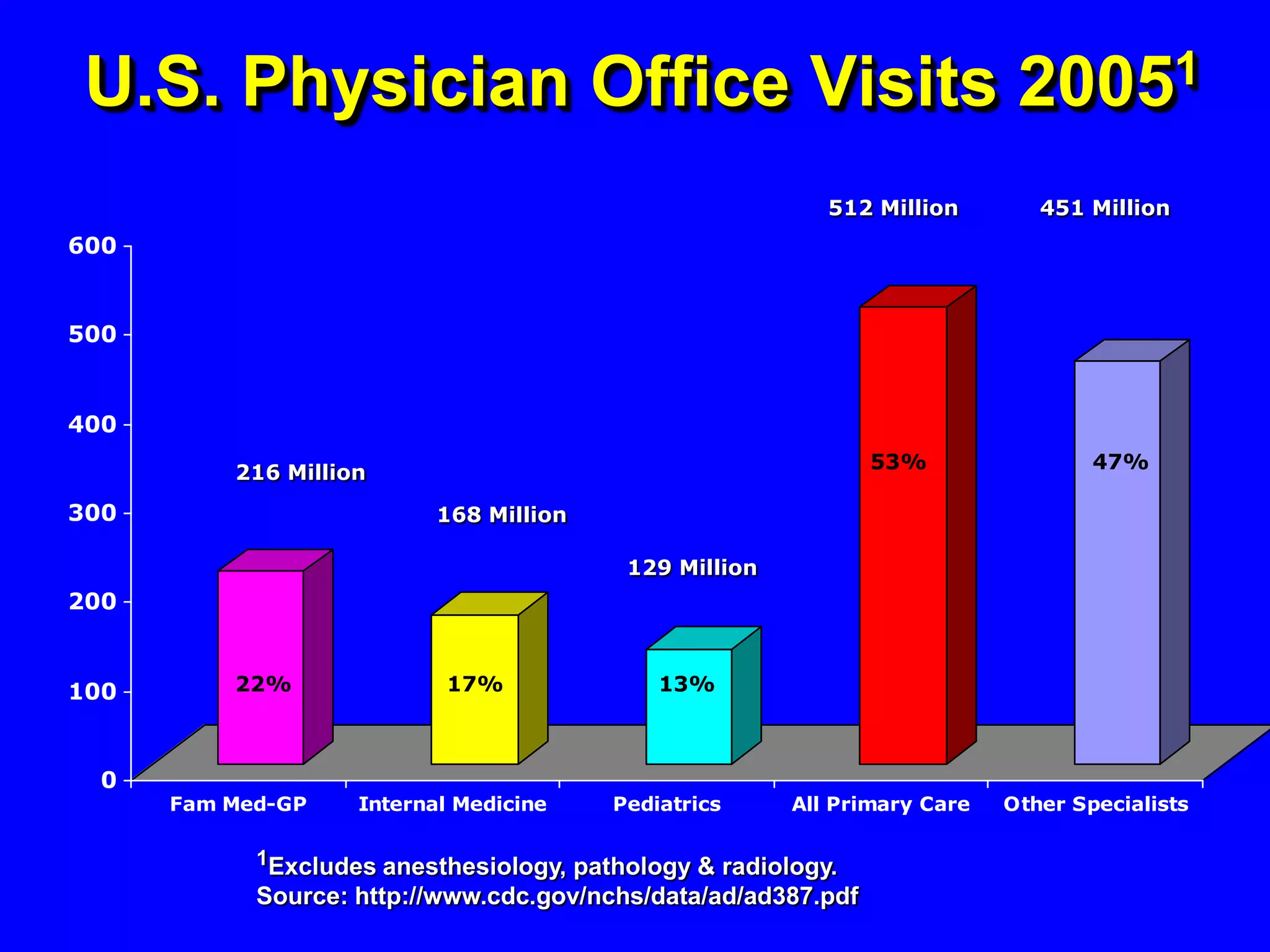
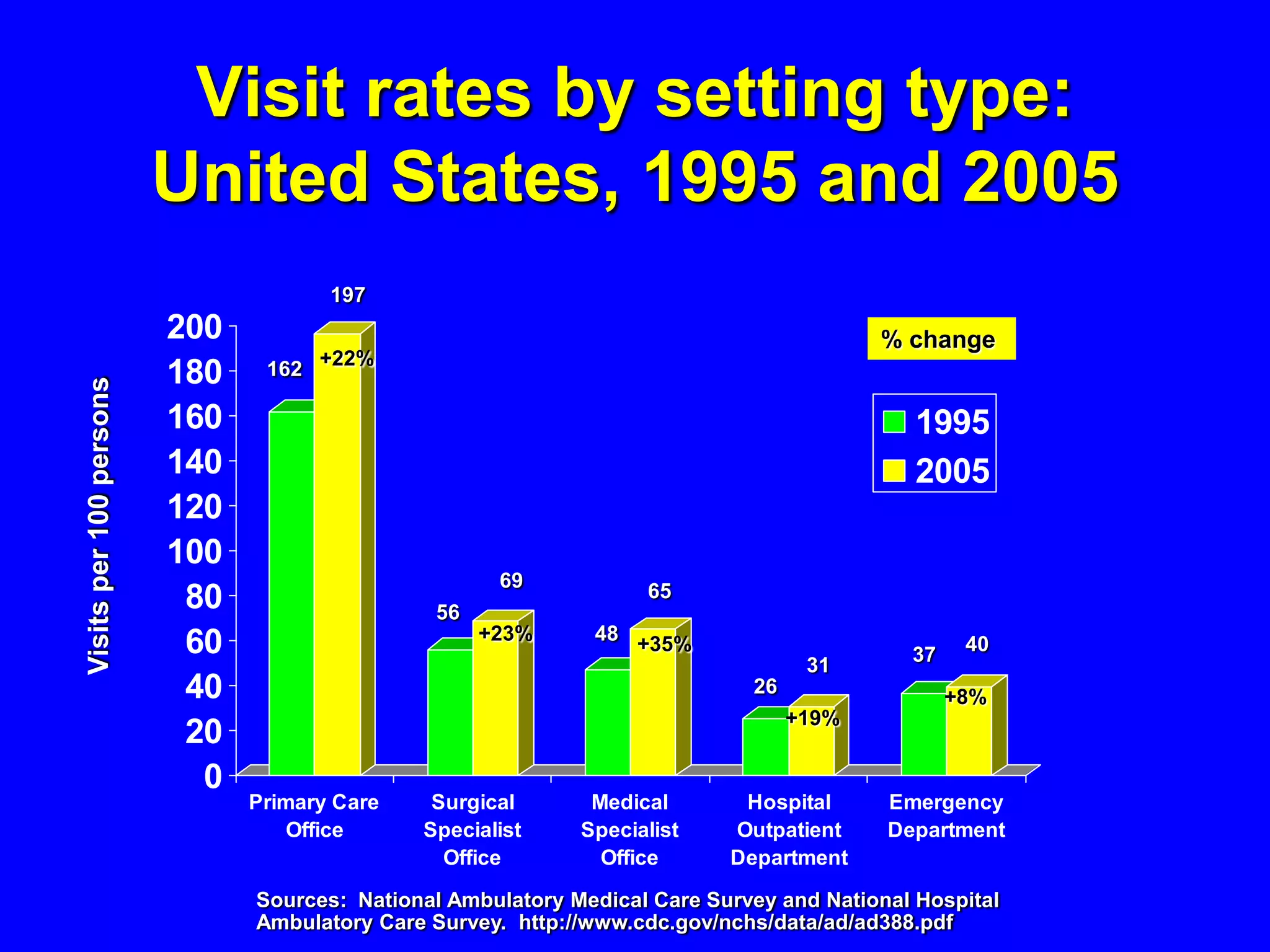
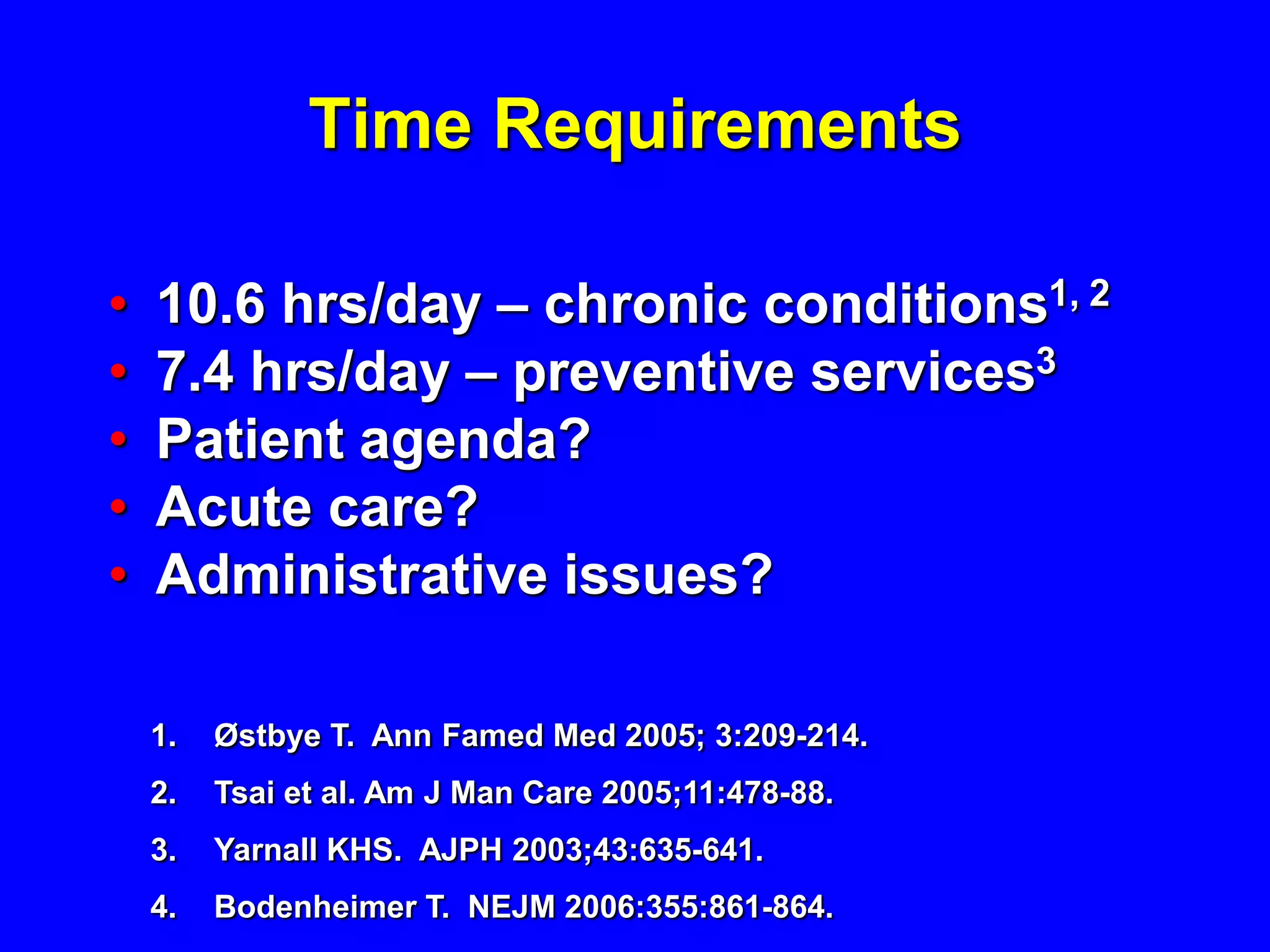
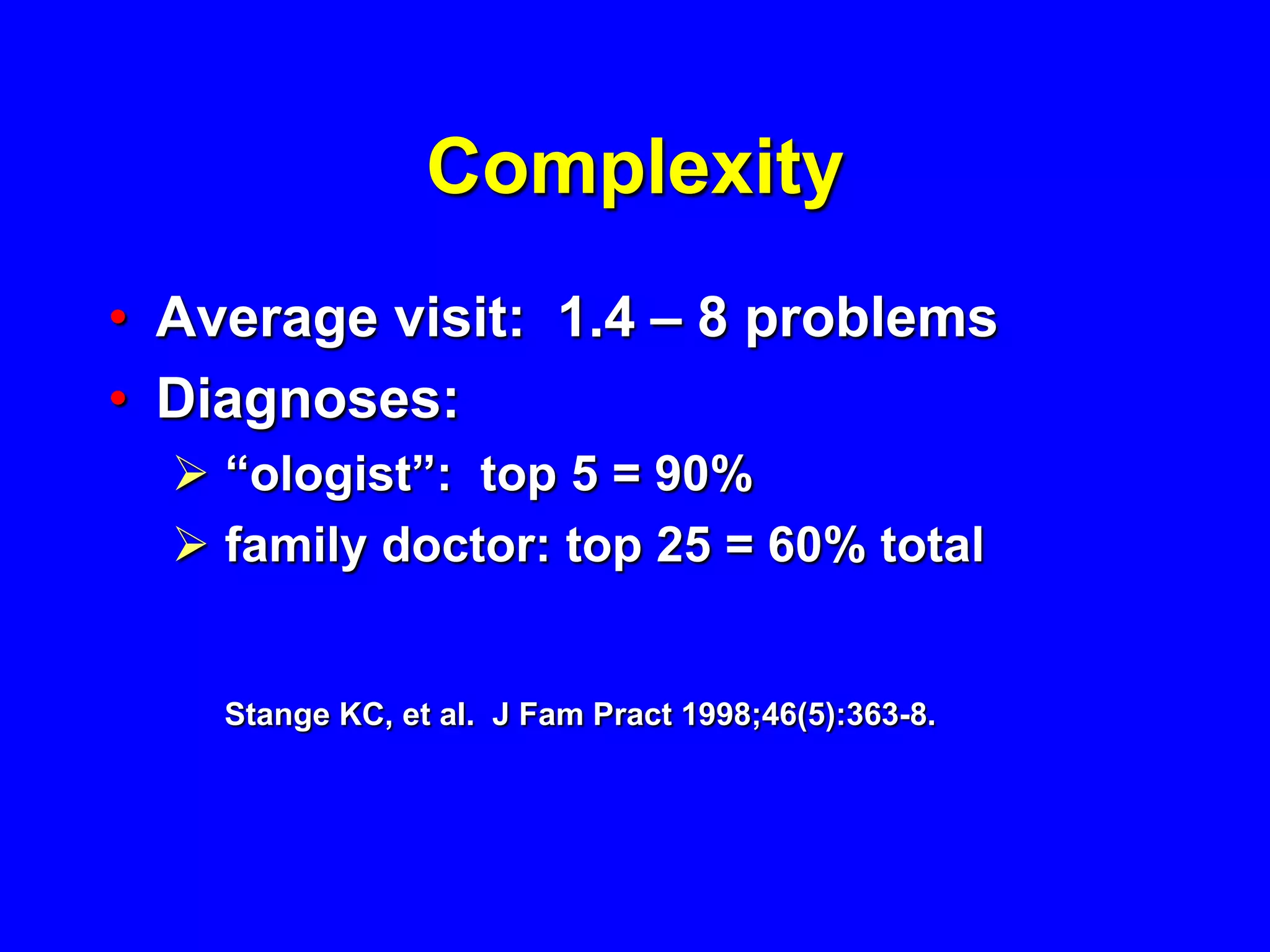
The document discusses the integral role of primary care in occupational health, emphasizing that most health care services, including occupational health, should occur within primary care settings. It highlights the importance of continuity and comprehensive care, citing that relationships between primary care and occupational health professionals significantly influence health outcomes. The document also notes the challenges faced in effectively integrating workplace health issues into primary care, such as cultural barriers, complexity, and time constraints.