This document provides information on rheumatoid arthritis (RA), including:
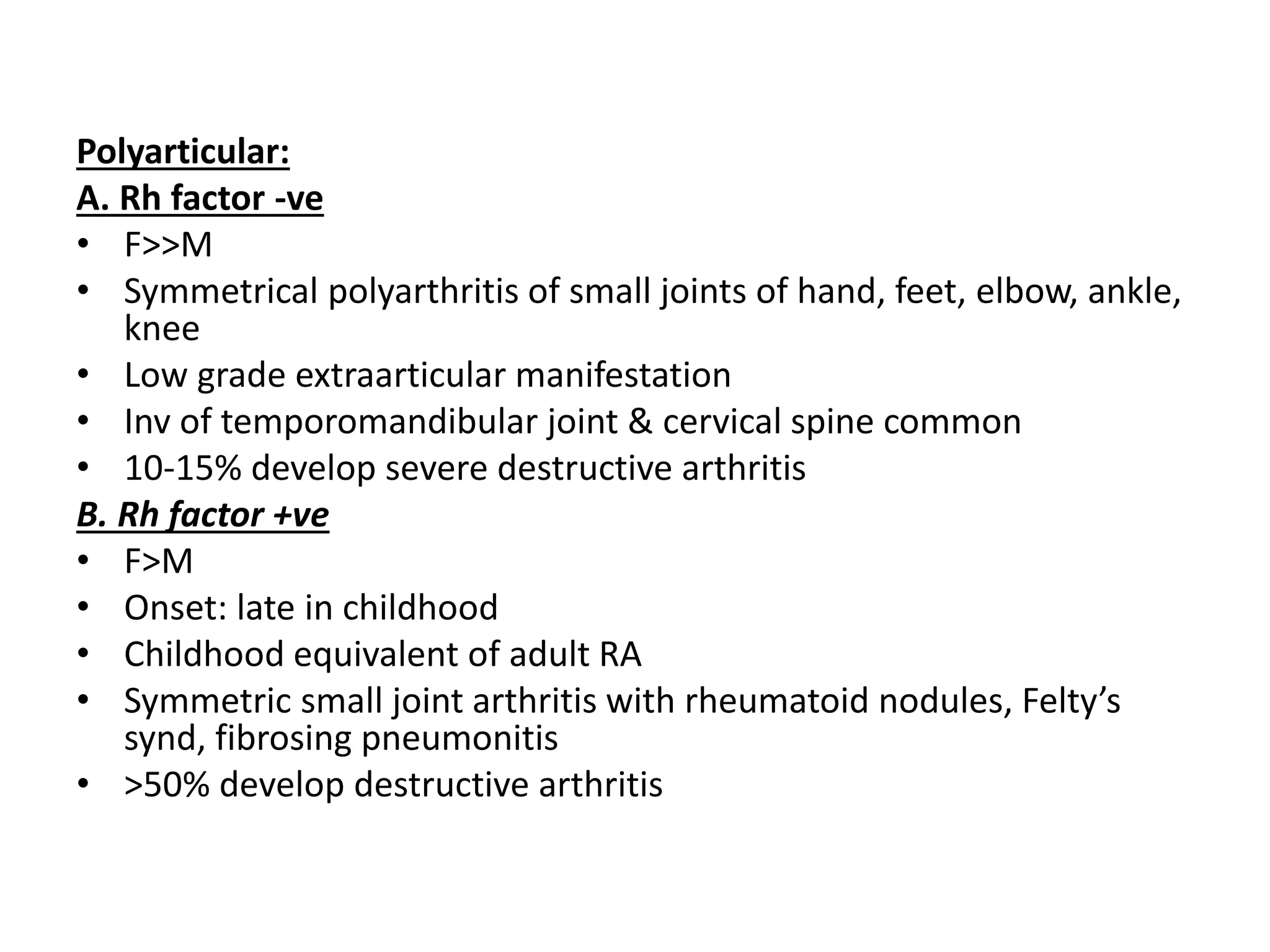
- RA is an autoimmune disease that results in chronic systemic inflammation, principally attacking synovial joints. It affects 1-3% of adults and is more common in women.
- Clinical manifestations include symmetrical joint pain, stiffness, and swelling typically in the hands, wrists and feet. This can lead to deformities like ulnar deviation.
- Extra-articular effects can include heart, lung, eye, nerve, and skin involvement.
- Diagnosis is based on criteria like joint symptoms lasting over 6 weeks and serological markers. Treatment aims to reduce inflammation and prevent joint damage.