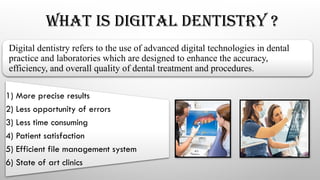
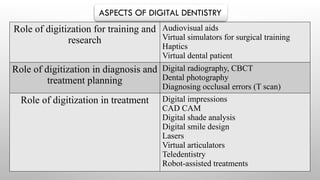
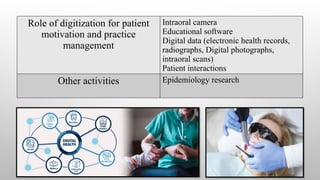
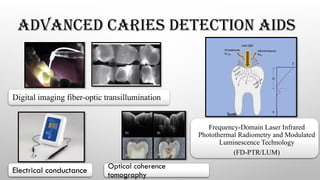
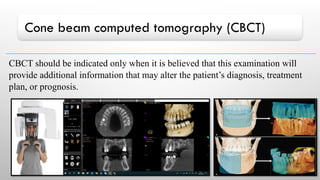
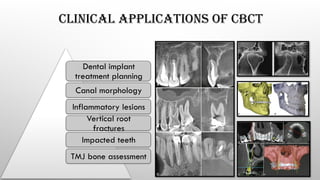
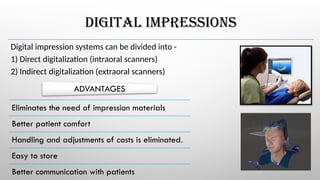
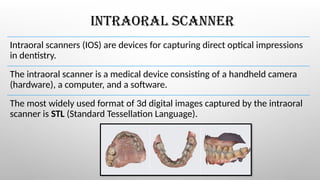
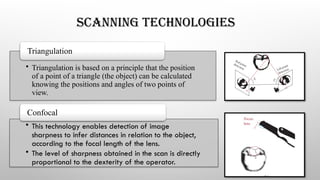
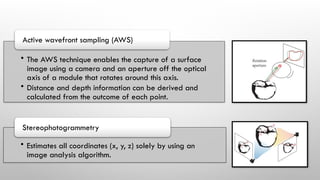
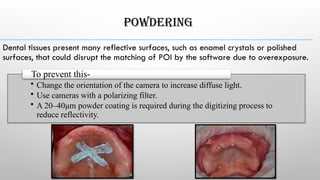
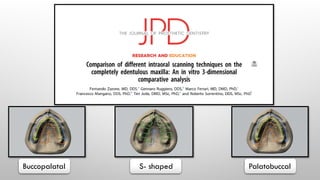
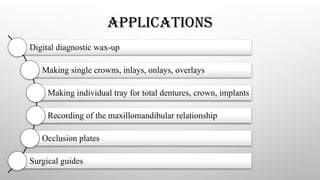
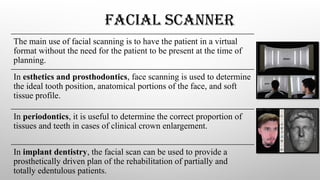
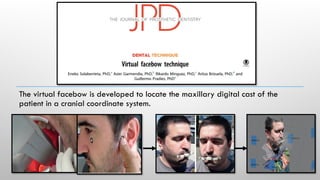
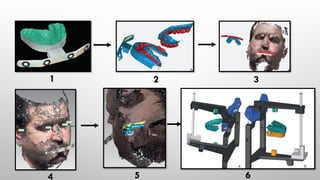
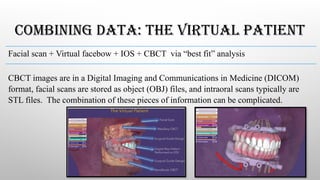
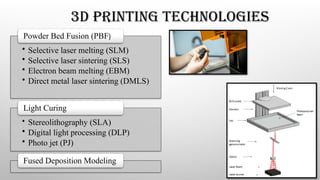
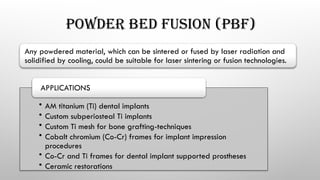
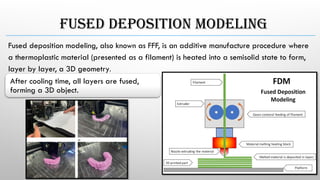
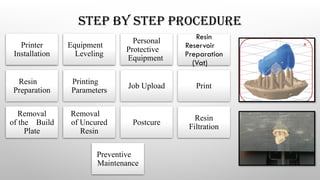
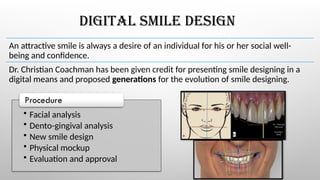
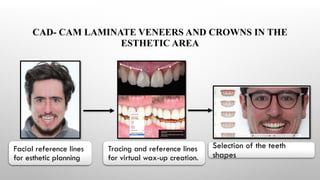
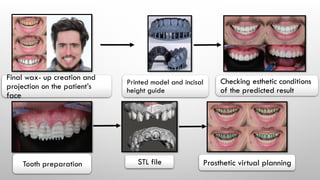
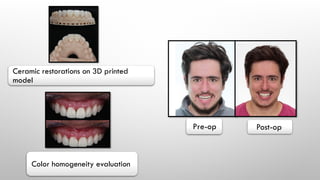
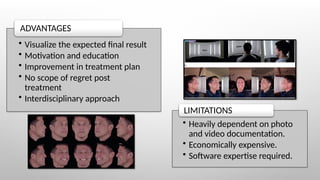
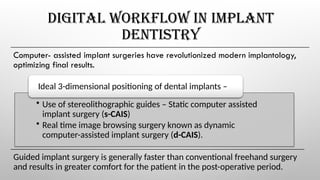
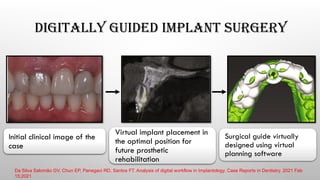
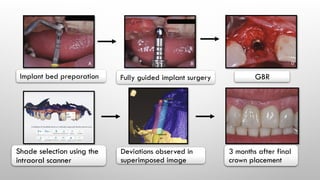
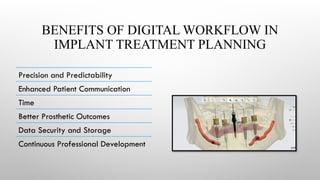
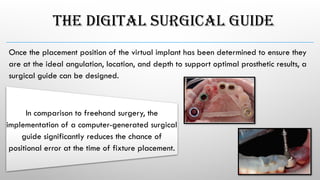
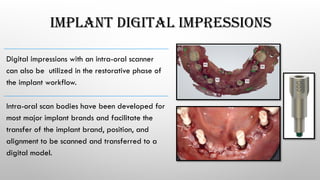
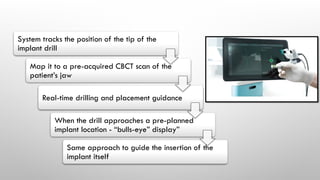
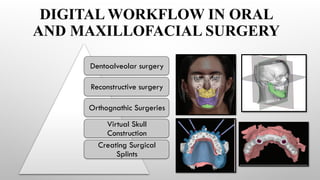
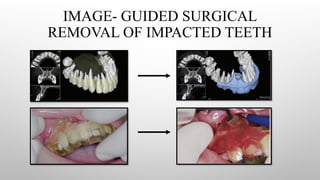
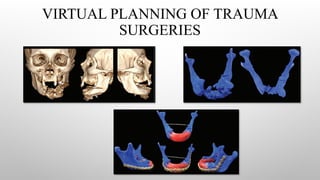
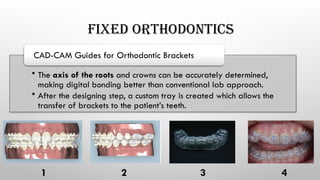
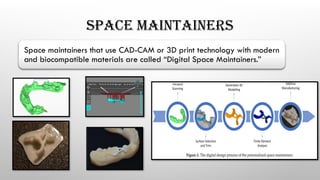
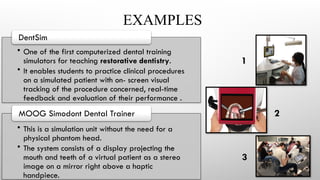
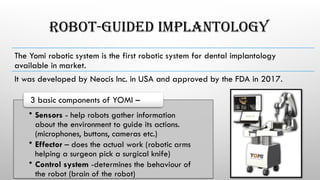
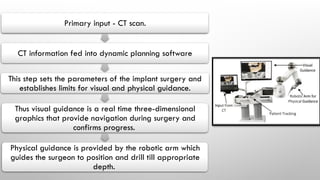
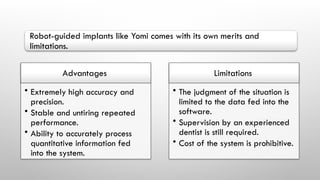
The document outlines advancements in digital dentistry, emphasizing improved accuracy, efficiency, and patient satisfaction through various digital technologies such as CAD/CAM, digital imaging, and 3D printing. It illustrates the role of digital tools in training, diagnosis, treatment planning, and patient management, depicting a shift from conventional techniques to more technology-driven processes. Additionally, it discusses various digital workflows, including digital smile design and computer-assisted implant surgeries, highlighting the benefits of precision and enhanced communication in dental practices.