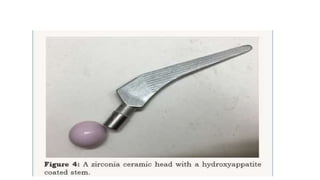
This document discusses recent advances in ceramic materials used in orthopaedics. It describes different types of ceramics including bioinert ceramics like alumina and zirconia, bioactive ceramics like hydroxyapatite and bioglass, and bioresorbable ceramics like tricalcium phosphate and calcium sulphate. It provides details on the composition, properties and biomedical applications of these ceramics for uses like bone grafts, prosthesis coatings, and filling bone defects.