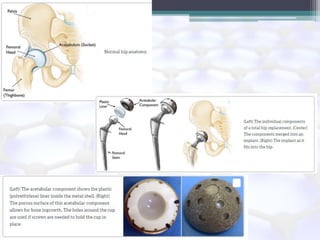
This document discusses various ceramic biomaterials, including their properties and applications. It describes how ceramics have superior chemical compatibility with tissues like bone and are similar in composition. The main ceramics discussed are alumina, calcium phosphates like hydroxyapatite and tricalcium phosphate, and bioglasses. Alumina is chemically inert and used in hip and knee replacements due to its hardness and strength. Calcium phosphates resemble bone minerals and have excellent biocompatibility. Bioglasses bond to tissue and their dissolution stimulates bone growth. These ceramics are important materials for biomedical applications like implants, scaffolds and drug delivery.