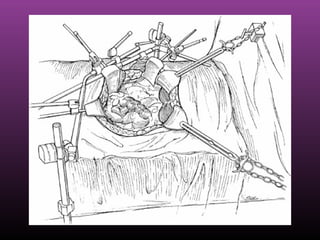
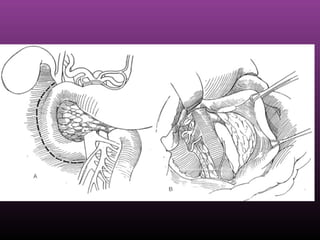
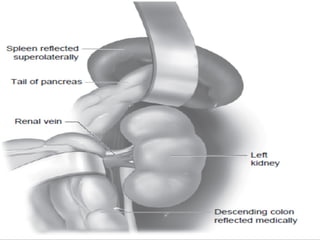
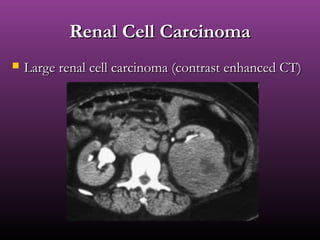
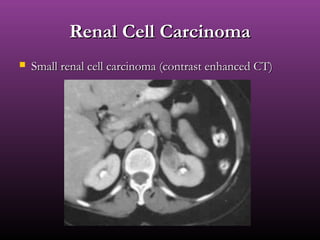
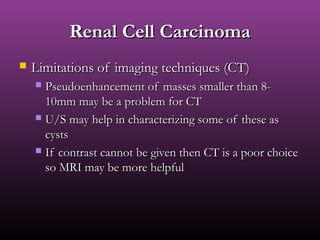
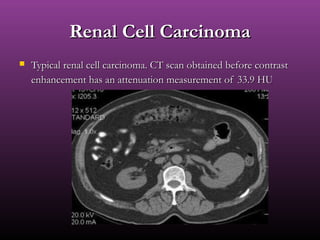
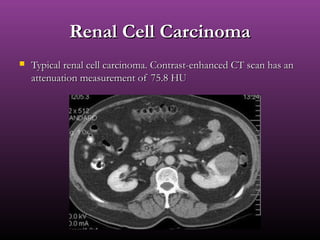
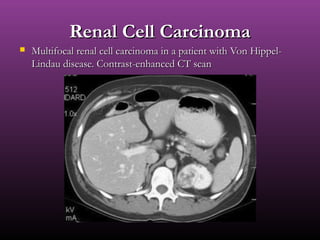
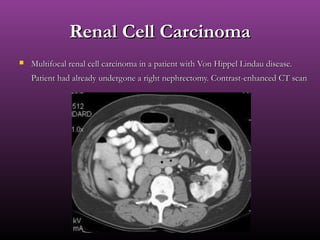
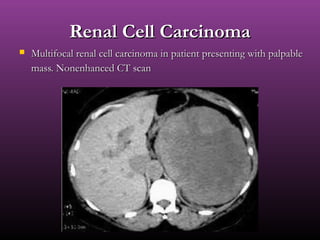
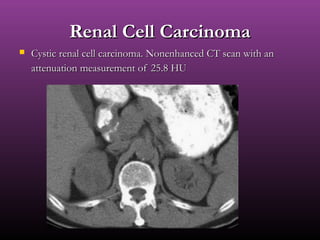
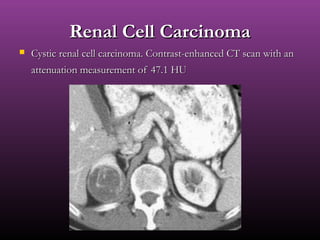
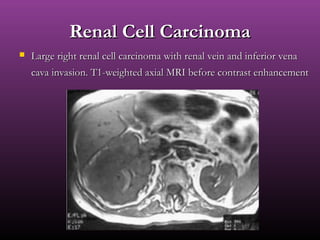
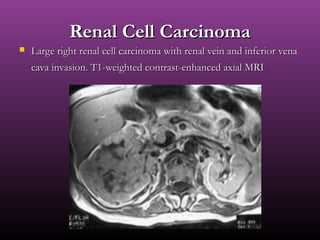
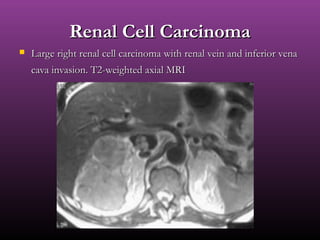
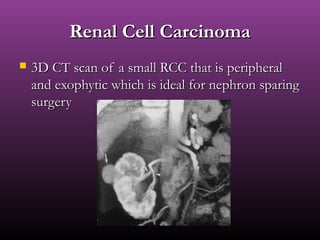
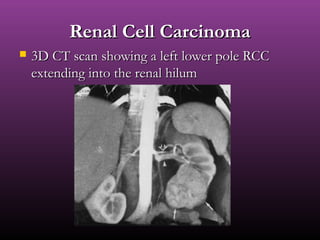
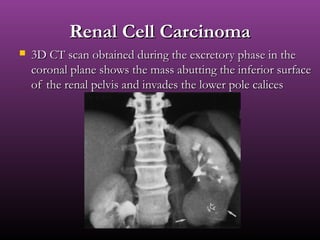
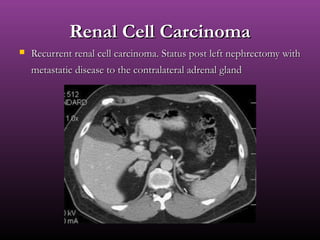
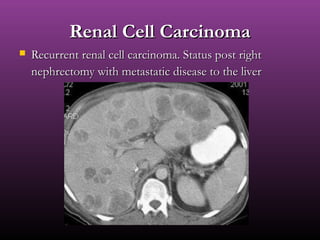
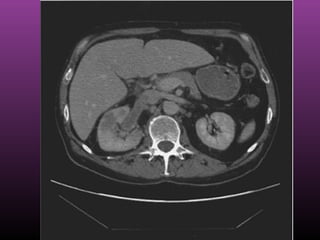
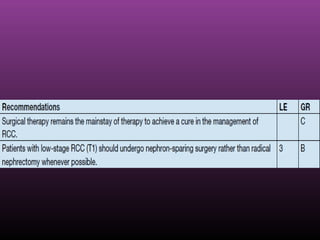
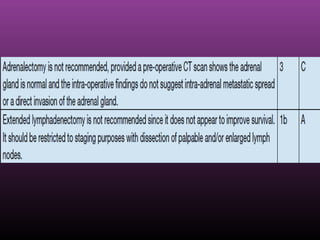
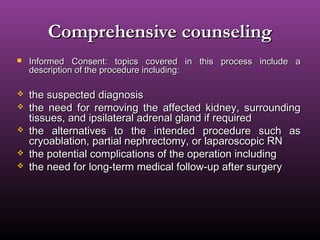
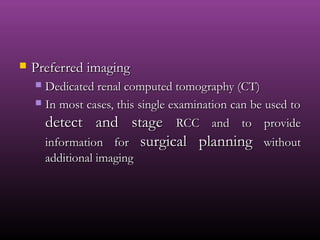
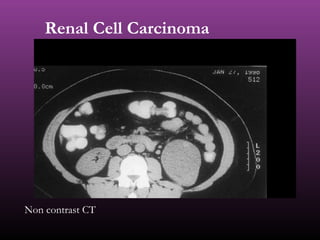
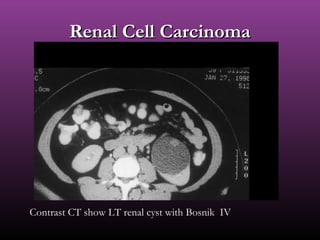
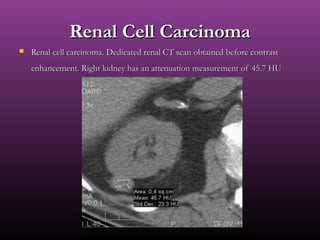
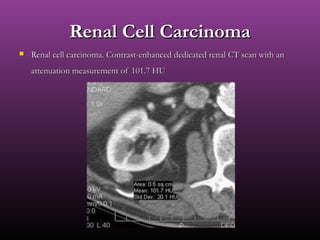
Radical nephrectomy involves the complete surgical removal of a kidney along with surrounding tissues including perirenal fat, regional lymph nodes, and sometimes the adrenal gland. The procedure was pioneered in the 1960s and became the standard treatment for renal cell carcinoma over the next 20 years. Contemporary radical nephrectomy involves careful patient selection, comprehensive counseling, and surgical removal while minimizing complications and maximizing oncologic outcomes. Dedicated renal CT is the preferred imaging to detect and stage renal cell carcinoma prior to radical nephrectomy.


![Open surgeryOpen surgery
RNRN
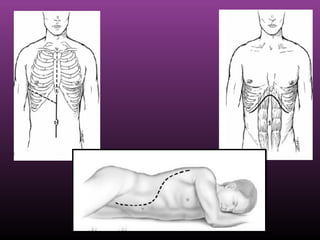
How to choose theHow to choose the
incision?incision?
surgeon's preferencesurgeon's preference
patient's body habituspatient's body habitus
tumor size & sitetumor size & site
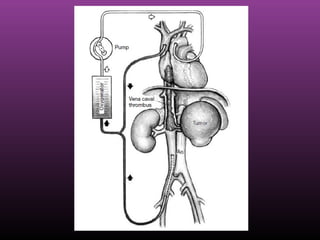
Other pathology [IVCOther pathology [IVC
thrombus]thrombus]
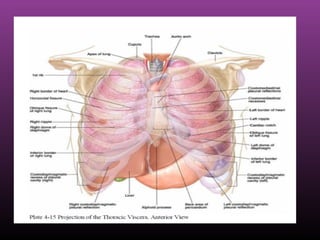
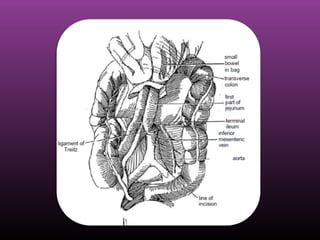
What are the types ofWhat are the types of
incisions?incisions?
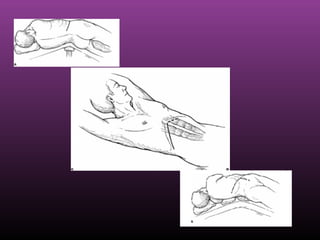
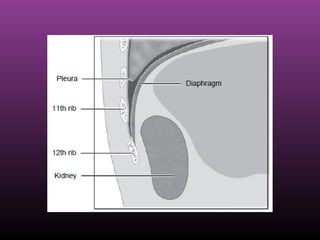
Supracostal flank incisionSupracostal flank incision
transperitoneal midlinetransperitoneal midline
transperitoneal subcostaltransperitoneal subcostal
incisionincision
ThoracoabdominalThoracoabdominal
incisionincision](https://image.slidesharecdn.com/rcc-181116140547/85/Rcc-30-320.jpg)