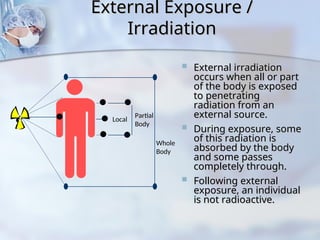
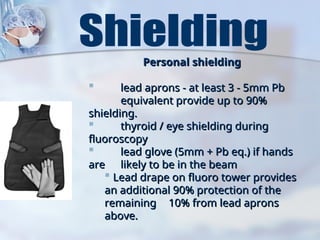
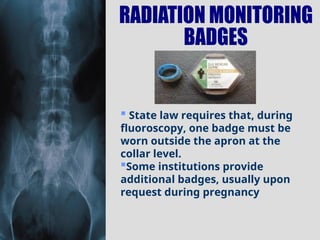
The document outlines the concepts and safety measures related to radiation, including its types, effects on the human body, and methods for protecting individuals from exposure. It describes ionizing radiation, internal and external exposure, biological effects, radiation dose measurement units, and the significance of distance, time, and shielding in reducing radiation risk. The document emphasizes adherence to the ALARA principle (As Low As Reasonably Achievable) to minimize radiation exposure for both personnel and patients.