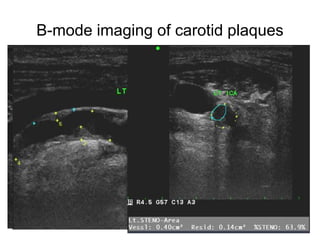
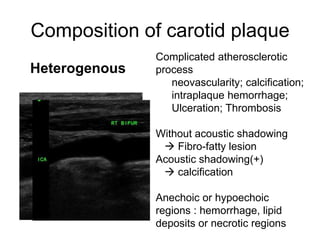
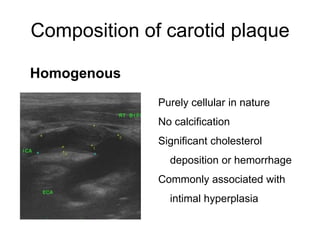
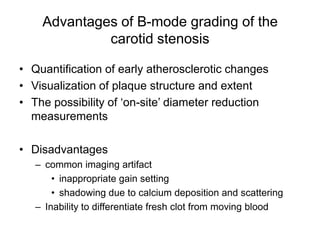
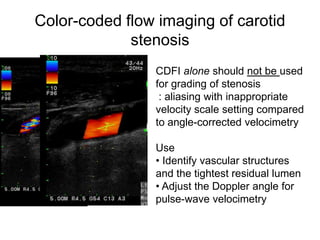
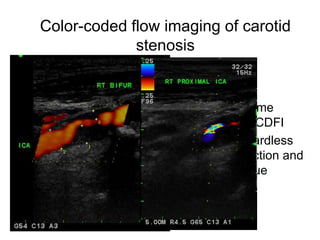
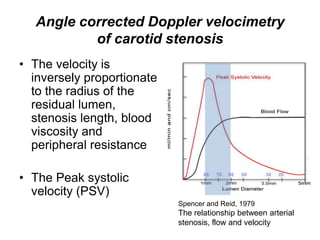
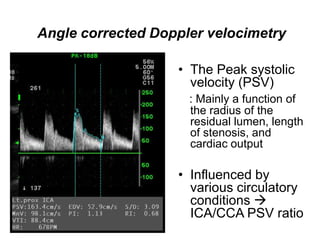
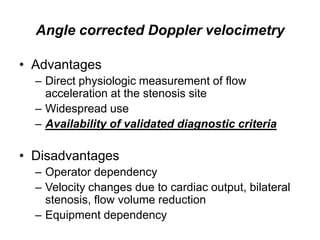
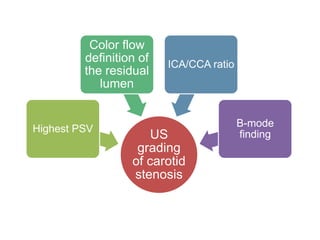
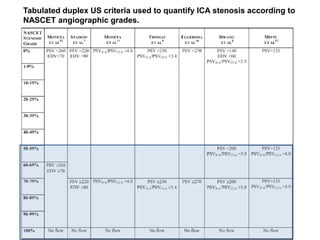
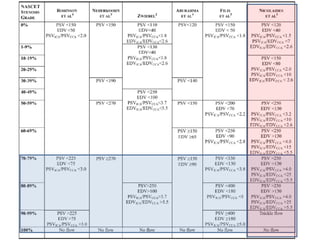
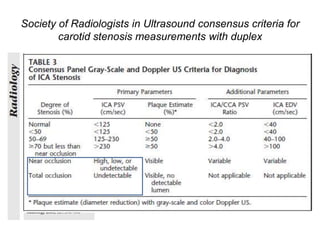
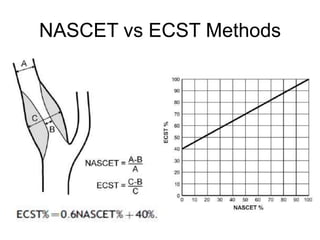
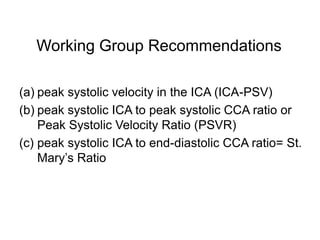
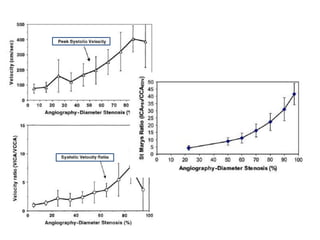
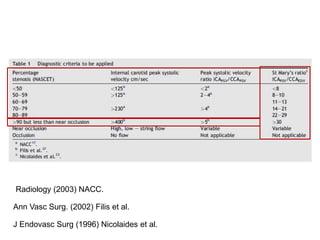
This document discusses various methods for quantifying internal carotid artery stenosis using duplex ultrasound. It describes using B-mode imaging to visualize carotid plaques and color flow imaging to identify the residual lumen and adjust the Doppler angle. Angle-corrected Doppler velocimetry measures peak systolic velocity, which is inversely related to the residual lumen radius and stenosis length. Ratios of internal to common carotid artery velocities are also used, with different standards from NASCET versus ECST angiographic studies. The recommendations are to measure peak systolic velocity in the internal carotid artery and velocity ratios of internal to common carotid arteries.